- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
TailorMed’s Manners: Addressing Financial Concerns in Cancer Care Improves Overall Patient Experience
Evidence-Based Oncology™ (EBO) spoke with TailorMed's Ian Manners about the financial assistance and consumer protection landscape, and what the cost of cancer care means to patient experience and outcomes.
Innovation in cancer care carries a price tag, one that has been well documented during the past decade. Studies of “financial toxicity” chronicle reports from patients with cancer who do not fill their prescriptions,1 and surveys find these patients have higher-than-expected rates of depression.2
Practices striving for high-quality care may try to fill the gap by connecting patients with financial assistance programs, but that can be challenging, too. Each program may have specific requirements; without support, the process can be labor intensive.
Filling this void is TailorMed, a software company with offices in New York City and Tel Aviv, Israel, whose platforms include a financial navigation technology that helps practices connect patients with financial assistance; the hope is that patients will not delay care and that practices and health systems will not have to absorb uncompensated care.3 Testimonials for TailorMed, such as the one from Highlands Oncology Group in northwestern Arkansas, describe moving from a system of manual workflows and sticky notes to a platform that increased co-pay assistance 24% in a single year.
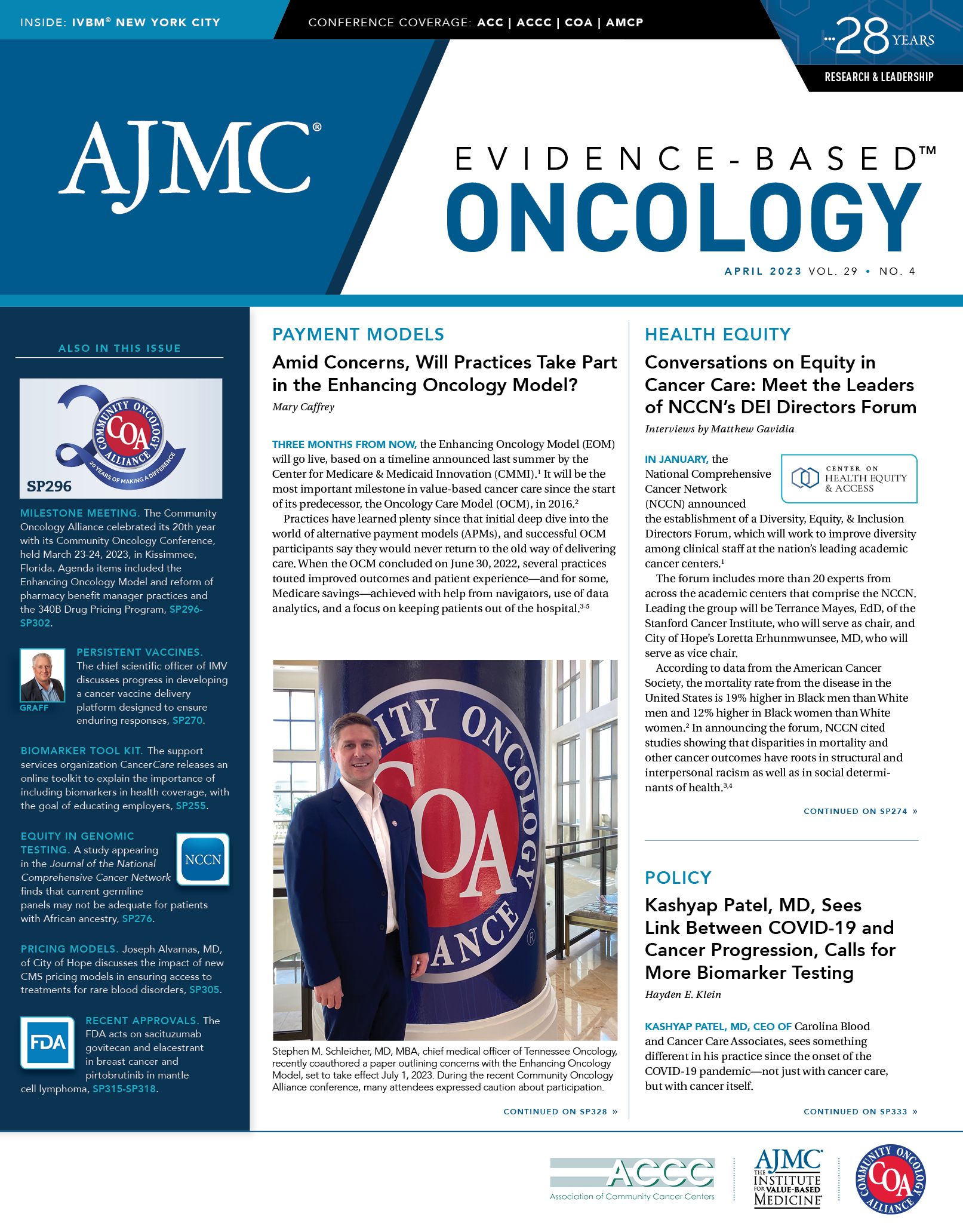
Manners

In 2021, TailorMed acquired Vivor,4 bringing Ian Manners, MBA, now the company’s chief strategy officer and head of life sciences, into the fold. In the year after the acquisition, the company reported securing $1.75 billion in patient funding, bringing the cumulative value of patient funding to $2.9 billion since its founding in 2016.5
Evidence-Based Oncology™ (EBO) spoke with Manners about the financial assistance and consumer protection landscape, and what the cost of cancer care means to patient experience and outcomes. This interview has been edited lightly for length and clarity.
EBO: We recently wrote about a survey that found patients receiving diagnoses of cancer are sometimes more concerned about the cost of treatment than the disease itself.6 I’m curious how this aligns with your experience.
Manners: It absolutely aligns with what I’ve seen over the years, which is the fact that when someone is facing a terrible diagnosis, immediately their mind jumps to, “What is this going to cost?” There’s so much that’s complex, not only in cancer care, but I think it’s such a striking example. There are so many complicated treatments, imaging, and drugs that are involved; it’s basically impossible to avoid having those costs—and the costs grow as a patient goes through the treatment process. What we’ve found at TailorMed is what patients will look at where they might seek treatment for a disease like cancer is, first, I’m looking for the best—the best surgeon, the best oncologist who’s going to help me, although it’s also important to think about the financial part of the journey. Some providers are very far along at helping the patient think about the financial experience, while others still have more work to do.
EBO: Last fall, The New York Times published a series about health care billing and transparency issues, including a piece that focused on abuses of the 340B Drug Pricing Program—and how this has trickled down to the patient level.7 This was the first time this issue has moved from health policy journals into the mainstream media. It appears this is an issue where there is bipartisan consensus that reform is needed to protect patients. What is your sense?
Manners: It’s a great question. I read the same pieces you did—some of those stories are really heartbreaking. At the policy level, we certainly did see attention in the last Congress on the question of how can we address health care affordability, with a lot of focus on medication expenses and negotiation provisions with pharma companies. What I expect to see next is a lot of attention on the problem. As you mentioned, we started to see that in the media. I’m less optimistic that there might be a policy solution that comes in a divided Congress, as we will have for the next 2 years. But I think having some more attention on the problem itself is certainly a beneficial part of the conversation. For me, and for us at TailorMed, I think what it highlights is the responsibility that health care providers, especially nonprofit [organizations], have to be thinking proactively about how they address the issue of affordability for their patients. That’s something that they can already be doing even absent policy questions and policy resolution, by doing things like implementing financial navigation services for their patients, by helping to identify resources that can help. They might even be able to do more than that, by proactively offering availability of internal hardship programs, to just explaining why they can benefit the community. I think for nonprofit providers, that’s especially important.
EBO: The high cost of cancer treatments no longer affects just the poor—it affects anyone of modest means. Unless you’re wealthy, cancer treatment can have an impact on an entire family. For providers in the nonprofit sector, would the ability to offer patients and families financial assistance programs be something they would want to advertise in their communities?
Manners: More and more, I think the answer is yes. As I was saying before, it’s usually not the first thought when someone’s thinking about, “Where should I seek treatment for this life-altering disease,” but it should be. We’re starting to see that more and more providers are talking about the financial experience that they offer as a reason why patients should choose their site to seek care. Clearly, it’s important. If financial concerns are sometimes even more top of mind than going through the disease itself, that’s a reason why people should be thinking about this when they choose where to seek care. And what we’re seeing with the provider organizations that we work with, especially at TailorMed but with others that we talk to, is that the financial experience is increasingly top of mind. CEOs are thinking about it, and revenue cycle heads are thinking about it. We always say, the more that providers can be proactive in addressing financial concerns that patients have—by offering interventions, offering resources—all of that comes together to a better financial experience, and ultimately a better overall experience for the patient.
EBO: Families are smaller than they were a generation ago. How does this affect the burden of cancer care? And how does it affect the work that you do?
Manners: One thing that’s important to highlight is that the financial impact of a cancer diagnosis is not just about the treatment itself. It’s all the other ways in which it changes someone’s life as you’re going through that experience. When it comes to caregivers, the impact extends to them as well. It might result in someone having to take more time off work, incurring transportation expenses—the list goes on. The way this affects our approach and what we do at TailorMed is that when we’re cataloguing all the financial resources that are available for patients and helping connect the right patients with those resources through our technology, we don’t just stop at the medication costs or treatment costs. We include local charities and forms of assistance that affect social determinants of health. We try to take that comprehensive approach.
EBO: In the past 2 years the costs of travel have become a more important issue with the rising cost of gasoline. How does the cost of travel affect treatment choices?
Manners: It’s not just travel—parking in cities is another cost. These things can really add up when you have to come in frequently for imaging, for radiation, for chemotherapy. It’s a big consideration, and it certainly causes patients to adjust where they might seek care. It’s prompted large providers to set up satellite facilities that are closer to home for more patients. That’s a good thing, but it does have consequences….We’re identifying these resources for patients that help to overcome some of those barriers, so that patients are able to choose the best place to seek care as opposed to the least expensive or the most convenient. Addressing transportation as well as other nontreatment factors is a big part of that.
EBO: How do health equity considerations affect your work?
Manners: I love that you asked that question, because it’s top of mind for what we do. What happens so often is that resources that are available to help patients—whether it’s for cancer treatment or other expensive diseases—all too often, they end up flowing to people who are most able to navigate the system. And that, unfortunately, perpetuates inequity because it means people who live in higher-income areas are more likely to get access to various assistance programs. The way we see it, the more that you can automate things—by streamlining them, by using technology—it helps to level the playing field. No one should have to choose between lifesaving care and being able to meet their basic living expenses. The more that we can use technology to identify how patients can reduce their out-of-pocket costs and gain access to lifesaving care, that means that in the long run, we’re going to be improving equity as well. And so that’s…very close to our mission here at TailorMed.
EBO: What else are you hopeful about in the next year?
Manners: The legislation that passed last year—the Inflation Reduction Act [of 2022]—specifically targeted the maximum amount out-of-pocket costs for Medicare beneficiaries and prescription drug plans, that won’t take full effect for another year or two.8 But that’s going to make a big difference—not for a large number of patients necessarily, but for those patients who are experiencing the highest out-of-pocket costs who are on Medicare. And I think that in particular is a big deal. We’ll be paying close attention to see how that tracks along in the implementation plan that they set out in the timeline.
Having these discussions about the role that providers have to play in addressing affordability challenges is…healthy….It won’t be easy at times. And I think there’ll certainly be a lot of open discussion and a lot of debate. But I think asking these questions is important, and providers that really are going above and beyond to do more for their patients and more for their financial experience will be in a better position over the next couple of years.
References
1. Dusetzina SB, Huskamp HA, Rothman RL, et al. Many Medicare beneficiaries do not fill high-price specialty drug prescriptions. Health Aff (Millwood). 2022;41(4):487-496. doi:10.1377/hlthaff.2021.01742
2. New study finds cancer-related anxiety and depression are costing Medicare $5B annually. News release. Blue Note Therapeutics. March 31, 2022. Accessed March 12, 2023. http://bit.ly/3JaHmRM
3. Removing financial barriers to care. TailorMed. Accessed March 12, 2023. https://tailormed.co/
4. TailorMed announces acquisition of Vivor to create the largest provider and pharmacy network tackling financial barriers to care. News release. TailorMed. November 29, 2021. Accessed March 12, 2023. http://bit.ly/3YHNXbV
5. TailorMed deepens commitment to healthcare affordability, closes 2022 with demonstrated growth and momentum. News release. TailorMed. January 30, 2023. Accessed March 12, 2023. http://bit.ly/3JzV4yS
6. Shaw ML. Financial toxicity from cancer is a patient-facing problem, MSK’s Chino states. The American Journal of Managed Care®. Published online December 6, 2022. Accessed March 12, 2023. https://www.ajmc.com/view/financial-toxicity-from-cancer-is-a-patient-facing-problem-msk-s-chino-states
7. Thomas K, Silver-Greenberg J. How a hospital chain used a poor neighborhood to turn huge profits. The New York Times. September 24, 2022. Accessed March 12, 2023. https://bit.ly/3DdPiiS
8. HHS releases initial guidance for Medicare prescription drug inflation rebate program. News release. HHS website. February 9, 2023. Accessed March 12, 2023. http://bit.ly/3LoYOoq