- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Conversations on Equity in Cancer Care: Meet the Leaders of NCCN’s DEI Directors Forum
In January, the National Comprehensive Cancer Network (NCCN) announced the establishment of a Diversity, Equity, & Inclusion Directors Forum, which will work to improve diversity among clinical staff at the nation’s leading academic cancer centers.1
The forum includes more than 20 experts from across the academic centers that comprise the NCCN. Leading the group will be Terrance Mayes, EdD, of the Stanford Cancer Institute, who will serve as chair, and City of Hope’s Loretta Erhunmwunsee, MD, who will serve as vice chair.
According to data from the American Cancer Society, the mortality rate from the disease in the United States is 19% higher in Black men than White men and 12% higher in Black women than White women.2 In announcing the forum, NCCN cited studies showing that disparities in mortality and other cancer outcomes have roots in structural and interpersonal racism as well as in social determinants of health.3,4
One way to narrow the gap in outcomes is to promote guideline-adherent care, which is the mission of NCCN. Having greater diversity among those who deliver care would also limit opportunities for bias and build trust among patients. However, there are very few minority doctors: only 5% of active US physicians are Black and only 5.8% are Hispanic; these percentages are less than half the population shares in the United States. Even fewer minority doctors serve in leadership roles.5
Addressing this gap will impact the bottom line of cancer centers: To retain federal funding, all designated centers will be required to design and implement a plan to boost faculty and workforce diversity. The NCCN DEI Directors Forum will offer support and resources to forward this effort.
“Increasing diverse representation among care providers is one overdue step toward improving the equity and quality of cancer care,” Robert W. Carlson, MD and CEO of NCCN, said in the announcement. “Unfortunately, we have a long way to go, and the people doing this crucial work are often underfunded and overburdened. We’re happy to be able to use NCCN’s existing infrastructure to address some of that burden.”1
Mayes and Erhunmwunsee spoke with Evidence-Based Oncology™ (EBO) about their new roles. Interviews have been edited lightly for clarity.
References
1. Terrance Mayes, EdD, and Loretta Erhunmwunsee, MD, FACS, announced as leaders for NCCN forum on equity. News release. National Comprehensive Cancer Network. January 17, 2023. Accessed February 25, 2023. https://www.nccn.org/home/news/newsdetails?NewsId=3601
2. Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer Statistics, 2022. CA: Cancer J Clin. 2022;72(1):7-33. doi:10.3322/caac.21708
3. Bristow RE, Powell MA, Al-Hammadi N, Chen L, Miller JP, Roland PY, et al. Disparities in ovarian cancer care quality and survival according to race and socioeconomic status. J Natl Cancer Inst. 2013;105(11):823-832. doi:10.1093/jnci/djt065
4. Ubbaonu C, Chang J, Ziogas A, Clair K, Tanjasiri SP, Bristow RE, et al. Disparities in the receipt of the National Comprehensive Cancer Network (NCCN) guideline adherent care in triple-negative breast cancer (TNBC) by race/ethnicity, socioeconomic status, and insurance type. J Clin Oncol. 2020;38(suppl 15):1080-10890. doi:10.1200/JCO.2020.38.15_suppl.1080
5. Morgan A, Shah K, Tran K, Chino F. Racial, ethnic, and gender representation in leadership positions at National Cancer Institute–designated cancer centers. JAMA Netw Open. 2021;4(6):e2112807. doi:10.1001/jamanetworkopen.2021.12807
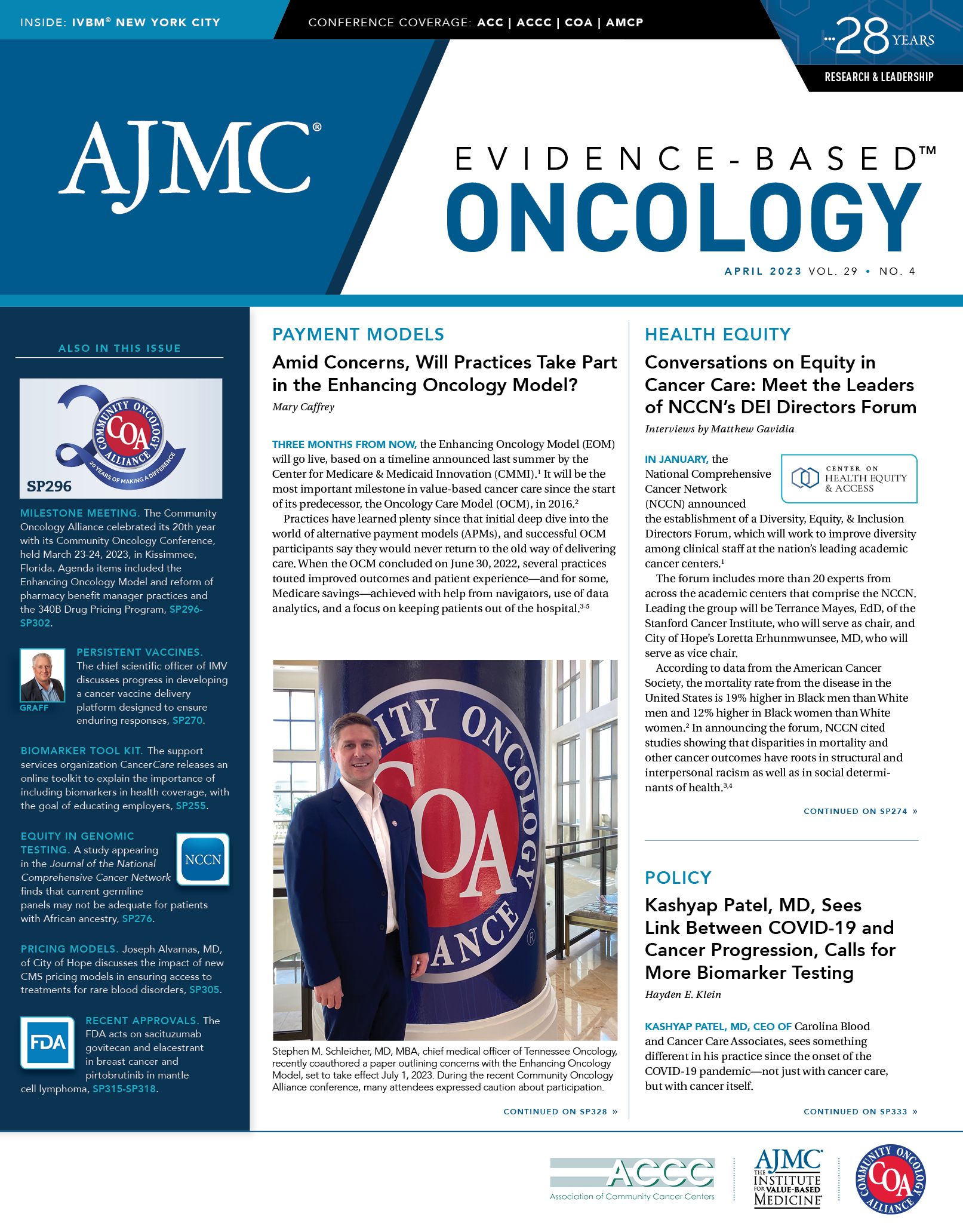
Loretta Erhunmwunsee, MD, FACS
Erhunmwunsee

Erhunmwunsee will be vice-chair of the NCCN’s DEI Directors Forum. She is a thoracic surgeon and assistant professor in City of Hope’s Division of Thoracic Surgery and Division of Health Inequities.
EBO: Can you speak about your goals and priorities as vice-chair of the NCCN DEI Directors Forum?
Erhunmwunsee: To achieve health equity, it is imperative that we attain true DEI within our workforce. And thus, we must move away from informative measures that simply discuss the benefits of DEI without any real change—instead, start making the cancer centers and institutions truly diverse, inclusive, and equitable.
Right now, there are just too few [minorities] represented in medicine, in the workforce, and certainly in leadership. Even if they are there, they frequently experience isolation. The truth is this has to change. So we at the new DEI Directors Forum hope to provide a venue for DEI leaders to show best practices and challenges regarding advancing DEI initiatives at the respective centers and to develop recommendations of new policies and practices to actually support DEI efforts so that we can get to a point where our workforce is truly diverse, inclusive, and equitable, and our patients therefore benefit and we can really walk towards health equity.
EBO: What lessons have you learned from your experience and research in thoracic cancer, as a surgeon and professor, as they pertain to health disparities and inequities? How will they influence your work in your new role?
Erhunmwunsee: My thoracic surgery and health equity research expertise is the foundation for my desire to promote DEI. Historically excluded patients have the worst outcomes in every lane, and we won’t achieve health equity if we don’t have diverse perspectives. We cannot keep doing the same things and expecting different outcomes. So, we truly need different voices and points of view, and we need members from the most burdened communities to be at the table making decisions which will increase diversity. We need those people to be welcomed and truly supported, thus increasing inclusion, and we need to treat these important members fairly, thus increasing equity.
The truth is DEI is not the natural course. It isn’t what happens naturally in a system that was created to advantage certain groups while disadvantaging others. We have to be intentional about these DEI efforts and we must prioritize them, or the status quo will continue. And the problem is that the status quo means increased death of Black and Brown groups—we’ve got to make these changes. My experience as a thoracic surgeon and a researcher that thinks about health equity is the reason why I’m such a proponent of true nonperformative DEI efforts.
EBO: The capabilities of precision medicine have grown substantially in recent years, particularly in lung cancer, but logistical challenges remain for underserved communities. What opportunities do you see regarding access to precision medicine across NCCN’s cancer centers?
Erhunmwunsee: I agree that precision medicine is gaining ever-increasing importance in health care. There are many concerns, though, that there is limited access in historically excluded communities, which might make disparities worse. There are also concerns that many of the trials that are the basis for the precision medicine movement lack true racial and ethnic representation from those who have the highest burden of disease.
So, there’s certainly a need for great attention to assure that those who are typically excluded are intentionally sought out to partner and join these efforts. And we believe that having a cancer center workforce that is actually diverse and is truly inclusive would positively impact efforts in this vein.
Having a diverse, inclusive, and equitable workforce allows for us to truly impact communities that have been marginalized and excluded. It allows for us to come up with more novel ideas about how to get precision medicine and other novel treatment modalities, screening, or anything to these groups, and so again, DEI efforts should impact this greatly.
EBO: What practice- and policy-level issues are foremost in your mind in terms of DEI in clinical staff representation and care delivery?
Erhunmwunsee: One of the priorities is the understanding that our institutions must prioritize this work. The institutions should support the DEI leader with funding, resources, personnel, to show that they understand the importance of this very challenging work. For institutions to assume that the one DEI leader can fix the whole DEI problem alone suggests that the institutional leadership doesn’t fully grasp the depth of the issues.
One very important focus is revealing or reflecting the value of this work to institutions so that they can give the appropriate resources, funding, and priority to this work. No change will happen if there isn’t a focus and funding towards it, and so in this time where some funding might be scarcer, or there might be a tighter hold on funding, we’ve got to make sacrifices. For too long, DEI hasn’t been a priority and now it really needs to be and that needs to be shown.
Also, I think there should be metrics that can hold leadership accountable. Every institution should know the percentages of their demographics for their workforce, they need to know their retention and attrition data, they need to understand who’s being recruited and who’s making it to interviews. All of these data need to be clear, metrics need to be set, and leadership needs to be held accountable for these results.
EBO: What advice or recommendations on equitable care delivery would you give to residents or other medical professionals just entering the health system?
Erhunmwunsee: Great question—I would say first, welcome. For those who might be new to the health care system, our resident doctors, medical students, those who have an interest in potentially health equity or DEI efforts, or for doctors who want to make sure that they can give their patients the best care, I think I would say that providing equitable care means providing high-quality care to everyone. You can’t have equitable care without high quality, you can’t have high quality without making sure that everyone can get it.
We must make sure that all groups have access to high-quality care and that the barriers to this care are minimized. And, therefore, we’ve got to be cognizant of what the barriers might be for individual patients and for communities. It’s important to understand that we must include patients and their families in the discussion and in the decision-making so we have this idea of what quality care, equitable care might be, but the patient in the end has to contribute to that definition.
As a thoracic surgeon, I might think that the right answer for a patient with early-stage lung cancer is to undergo surgery, period, right? But the patient has to be included. I give them my knowledge and my expertise, and I give them the data, but in the end, it is a discussion. And so equitable care is care that is high-quality and is for everyone, it’s patient-centric.
We must also consider the whole patient, and that means understanding their social and environmental context or, as we all call it, their social determinants of health. In essence, I do believe that equitable care delivery means patient-centric, high-quality care that focuses on the whole patient and incorporates them into decision-making.
Terrance Mayes, EdD
Mayes

Mayes, who will chair the NCCN DEI Directors Forum, is the inaugural associate dean and executive director for Strategy, Equity, and Inclusion for the Stanford Medicine Enterprise Strategy Team, executive director of the Commission on Justice and Equity at Stanford Medicine, and associate director for DEI at the Stanford Cancer Institute.
EBO: What are your goals and priorities as chair of the DEI Forum?
Mayes: I was honored to be appointed inaugural chair of the NCCN DEI Forum. NCCN is an alliance of 32 leading cancer centers, all of which are devoted to patient care, research, and education. And Stanford is a proud founding member of this network; we joined in the 1990s.
The NCCN has long advocated for policies and practices to achieve equitable and accessible cancer care. But in recent years, and especially after the violence against Black Americans in the summer of 2020, the NCCN, like many organizations around the world, began to place a much greater and much needed focus on identifying and dismantling those deeply rooted historical, social, and structural barriers—barriers that have hampered progress, including barriers such as racism and other forms of discrimination.
So, I’m really proud to be a part of this group. The NCCN is established as a community of subject-matter experts, working together to address many of the issues I just mentioned and doing so through shared best practices, through policy, advocacy at all levels, and through education, and that’s what I am hoping we will do together as a community.
EBO: One of the forum’s primary aims is to improve diversity among clinical staff across NCCN’s cancer centers. What potential changes do you see in how diversity is promoted and measured across those centers?
Mayes: Yes, a major aim of the DEI Directors Forum is to increase diversity across the cancer workforce, including clinical staff and researchers, but I think we enter this work with a more nuanced understanding of what diversity actually means and how it benefits organizations—a greater understanding and depth of knowledge than we had decades ago. We have a much better appreciation of intersectionality and a clearer understanding of which data we should be tracking and how to use these data to advance a more diverse and inclusive organization.
I call my office at the Stanford Cancer Institute the JEDI office—justice, equity, diversity, and inclusion—and when I think about the opportunity ahead of us, about how this work is promoted, measured, and sustained, I’m interested in our leaning into the J in JEDI because where diversity asks the really important question of who’s in the room, justice asks who’s presence in the room is under constant threat.
Justice will ask what structures and systems are operating in our organizations that have allowed these inequities, whether they’re related to health, education, income, you name it. What are the historical structures that have allowed these inequities to not just persist but to thrive? So, that is the work that I’m interested in doing, not just with the Stanford Cancer Institute but also as part of the NCCN DEI Directors Forum.
EBO: What role can the forum play in raising awareness and interest in the medical field, particularly oncology, among racial and ethnic minorities?
Mayes: We are still in the early stages of setting up the NCCN DEI Directors Forum, and therefore, our goals and initiatives are somewhat to be determined right now. But what I’ll say broadly is that we have an opportunity to join forces in our campaign to broaden participation of underrepresented minorities in oncology research and in STEM (science, technology, engineering, and math) careers. Much of this work historically has been done within the silos of our individual institutions, and we now have this unique opportunity for collective impact, something that I’m very excited about.
EBO: You also serve as a director of DEI at Stanford Cancer Institute. What has been your experience managing equity-related issues in California and how will it influence your approach nationwide?
Mayes: I’ve had the honor of participating in or leading several DEI efforts at the state level, at the national level as well. I recall my time as a member of the team that authored Disrupting the Status Quo, a report from the University of California Health Sciences’ DEI Task Force and a document that has served as a strategic guide for all health centers across the University of California.
I also spent time on the Association of American Medical Colleges graduate research, education, and training steering committee. And what I’ve learned from these and other experiences is that we have to start by listening—we need to listen and listen some more. Listening to each other, certainly, but more importantly, listening to the communities that we are all working to uplift. And my job as the chair of the NCCN DEI Directors Forum is to help us align around a shared purpose and strategy, one that is informed by our community. Then I think I can just sort of get out of the way and let the magic happen because we have an incredible group of very thoughtful and experienced leaders on the Directors Forum.
EBO: The Forum will meet several times a year to formulate recommendations to support DEI efforts. What practice- and policy-level issues do you expect to be at the forefront of conversations, and what are some long-term goals here?
Mayes: As I mentioned, the Forum is just getting started, and so we’ve not fully built out a policy agenda yet, but I can guarantee you that we will have one. We intend to advocate for change across our individual institutions, across the NCCN itself, and also across state and federal governments. This work is too important.
We know that over the past few decades, we’ve seen incredible and hopefully lasting progress in cancer research, cancer care, cancer prevention. We’ve seen a 30-plus percent decline in cancer mortality in the United States since 1991, I believe. But this progress hasn’t been universally enjoyed by everyone. We know that there are differences based on a person’s race, gender, socioeconomic status, or where they live in the country—all of these things determine one’s chances of surviving cancer. That is simply not acceptable, and that is the work that the DEI Directors Forum will be committed to doing something about.
This work is going to require all of us. The DEI Directors Forum is here to help to catalyze change, but we can’t do it alone. We’re going to need our colleagues across the health care workforce, our colleagues across academia, our colleagues across government, if we are really going to move the needle this time, and I think we can do it.