- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
CancerCare Tool Kit Aims to Guide Employers in Biomarker Coverage Decisions
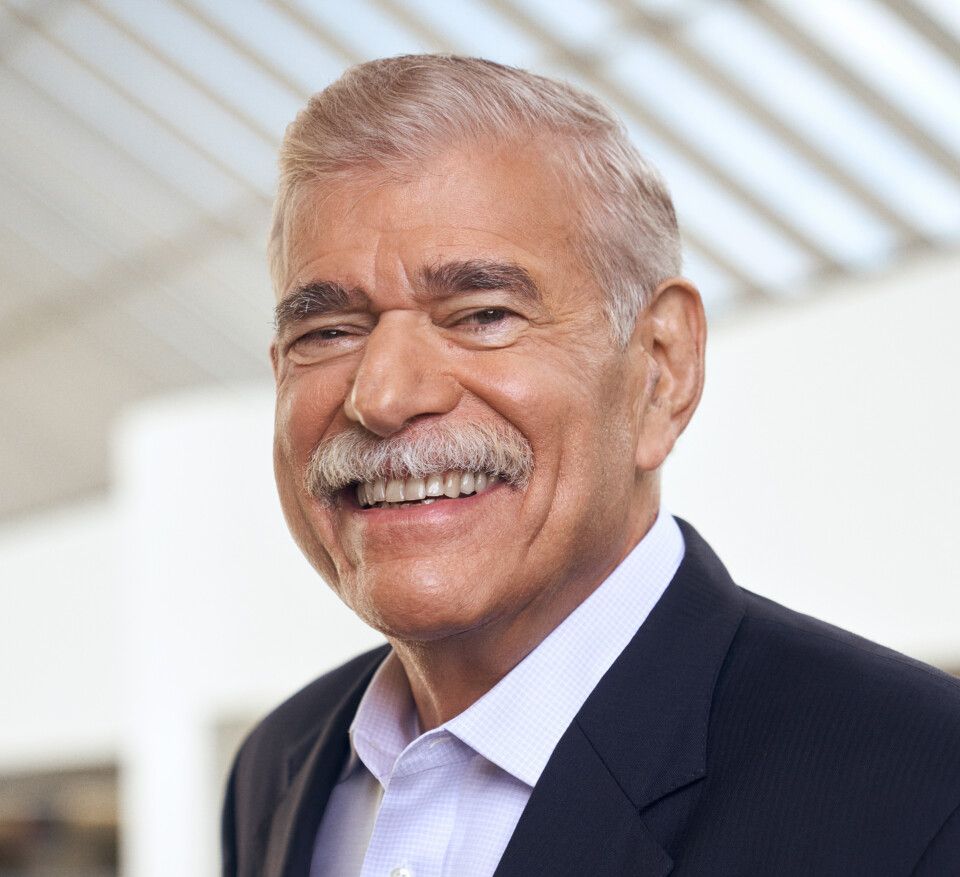
Evidence-Based Oncology (EBO) spoke with Len Lichtenfeld, MD, the chief medical officer for Jasper Health and a board member with CancerCare.
In the era of precision medicine in oncology, giving the right therapy to the right patient at the right time involves biomarker testing, which has been required or recommended for most new cancer drugs for the past 5 years.1 A 2018 study found that clinical pathways can optimize use of biomarkers and promote selection of the correct target therapy in lung cancer, for example.2
However, providers report that coverage for biomarker testing is inconsistent, leading to the use of older, more toxic treatments that are less effective than newer therapies. This occurs despite evidence that use of testing per National Comprehensive Cancer Network guidelines improves overall survival, especially in disease types with rapidly advancing treatment, such as lung cancer.3
To create a more equitable care environment, in February 2023 the support services organization CancerCare released the Employers’ Prescription for Employee Protection: Biomarker Toolkit (biomarker tool kit), an online document designed to educate human resources professionals so they can ask the right questions of benefits consultants and insurance providers.4 The goal, according to leaders at CancerCare, is to give employers or their designees enough knowledge to make prudent coverage decisions.
“Precision medicine in oncology has dramatically changed the way cancer is diagnosed and treated,” Patricia J. Goldsmith, CEO of CancerCare, said in a statement released with the new tool kit.4
“Employers that don’t adequately cover biomarker testing in their insurance plans create a real risk that their employees will not receive the most effective therapy, and instead receive suboptimal treatment or even treatment that could cause them harm.”
CancerCare officials cited lung cancer as an area where coverage for biomarker testing can make a difference: use of testing can help identify targeted therapies that have increased survival rates, and American Cancer Society data from 2021 show 89% of oncologists said biomarker testing improved their ability to prescribe the right drug.5 Despite this, research presented last year at the American Society of Clinical Oncology Annual Meeting shows that up to one-third of patients may not receive the right therapy due to inadequate coverage for biomarker testing, leading to disparities in clinical trial enrollment.6
To learn more about the biomarker tool kit, its role in ensuring that patients receive the right therapy, and the current precision oncology landscape, Evidence-Based Oncology (EBO) spoke with Len Lichtenfeld, MD, who spent 19 years with the American Cancer Society, mostly in the role of deputy chief medical officer. Today, Lichtenfeld is the chief medical officer for Jasper Health and a board member with CancerCare. This interview has been lightly edited for length and clarity.
Lichtenfeld
EBO: We continue to hear from physicians that while coverage for biomarker testing has improved in some areas, there are still gaps—that patients with Medicaid or lower-priced coverage still have a hard time gaining access. What is CancerCare’s perspective on the current state of access to biomarker testing?
LICHTENFELD: CancerCare is obviously very concerned about people, patients, families, caregivers, and loved ones having access to appropriate biomarker testing in their time of need. The problem is not just limited to those who don’t have insurance, or those who have Medicaid or less expensive insurance policies. Unfortunately, it seems to be a pretty universal phenomenon—and for a lot of different reasons. It’s just fascinating, and sad—having watched this develop over the course of time—that CancerCare and the folks that we represent still have this problem. We’ve made such incredible advances in the treatment of cancer, and yet access to those advances [is] not uniform…it’s not equitable, but it can impact everyone. Of course, CancerCare emphasizes in its biomarkers report that as a patient, you need to understand what the current state of the art is. You have to be your own advocate for getting the appropriate treatment that’s best for your cancer under your particular circumstances.
EBO: How does the landscape break down? Are there certain types of employers that do a better job than others at offering coverage for biomarker testing? Are there certain population groups that are at a particular disadvantage?
LICHTENFELD: It’s hard to know the all the intricacies and all the people who might be affected in different groups. Clearly, people who are uninsured have a major problem, and people who have Medicaid can have difficulty. But even people who have employer-based insurance—depending on how that insurance is structured—can have difficulty. And people with more traditional commercial plans can have problems because of what we call prior authorization, which [causes] delays, and leave[s] open the question of who will make sure you get the test you need in the time you need it.
Let’s remember, when we talk about biomarkers, we’re talking about not only a cancer that is treated at a particular time—we’re also talking about the ability to do circulating blood tests to look at tumor markers, to see how cancer can be best treated; you’re looking at familial genetic testing, to make sure you have access to that kind of treatment as well. So, it’s a pretty broad landscape. Recently, there was a piece—it’s hard to believe that it’s such a substantial number—that said up to a third of the people who should have a biomarker test to help treat their cancer aren’t getting one.7 And this is something we’ve known. I mean this story [of biomarkers] has evolved since the 1990s, but believe it or not, and we’re still having difficulty 30 years later in making sure people get access to the care that they need. And that’s what [is] of such great concern to me—and it’s also of concern to CancerCare, among many others.
EBO: Both the biomarker tool kit and the earlier document, the CancerCare Employer Toolkit, do a great job of explaining the problems with prior authorization in accessible language. What these documents describe is consistent with what we’ve heard from providers over the past 2 years. The problem seems to be getting worse, and now there is a significant gap between what clinical guidelines and pathways recommend and what practices can get through prior authorization in the real world. Is this what providers tell you?
LICHTENFELD: What strikes me about the CancerCare biomarker tool kit is that it’s targeted primarily to employers and benefit managers, but it’s really written in plain English—maybe not everybody can understand it, but a lot of patients and caregivers can understand what’s written in the document. It really lays it out in straightforward, understandable language: What are biomarkers? Why are they important? What do you need to know? In the case of human resources departments, what you should be looking for in the contracts you sign? A lot of people aren’t aware that if you’re employed by [a] large employer, your insurance may be what we call a self-insured plan. The commercial plans that cover people on the health exchanges are the ones where there are rules covering what you have access to. But if you’re in an employer-sponsored plan, the plan sets the rules of what they’re going to cover, how they’re going to cover it, and what they’re going to do. I’ve had situations in my own family with serious illness, and when you deal with the complexities of a serious disease like cancer, if you’ve lived that experience, it is like nothing else you’ve ever gone through. There are so many nooks and crannies, and so many places where “the system” can fall apart and not work on your behalf as a patient. It sets barriers in place—and some of those barriers, unfortunately, I think are intentional. Some are not intentional; you can have a great policy that covers everything in the world, but the test doesn’t get ordered. And if it’s not timely, and if the preauthorization is not submitted, and by the way, who’s going to submit the preauthorization? Is it going to be the primary doctor who’s trying to make the diagnosis? Is it going to be the pathologist who does the test and the diagnostic? Well, no, they don’t want to be bothered. Is it going to be the surgeon? Is it going to be the interventional radiologist, so you can get the benefit from these tests? Who are the people affected? We’re all affected. But particularly, it’s folks who were disadvantaged, who don’t know how to speak up. They [might] not be aware of what their options are; perhaps a person lives in a rural area….I know of a case [in a rural area] where getting the right test for the person took a tremendous amount of effort. It took literally 4 bites at the apple to get the right test. And then the right test showed that they had a mutation, a biomarker that would work for their cancer. If a person doesn’t have insurance, they may not be able to understand what the options are, they may not get access to high-quality care. Some states have actually enacted laws trying to improve access to biomarker testing, to make sure people get the right care.8 This results from a lot of politicking from a lot of people—some of whom don’t have necessarily the patients’ interests in mind. You would think that with something as remarkable as a biomarker test and a treatment that would work for your cancer that everybody would say yes, but that’s where we have a long way to go.
EBO: What does all this mean for health equity? Can you discuss the issue of disparities in who is getting biomarker testing?
LICHTENFELD: This is a huge, huge issue. Let me emphasize something: when we think about health equity, we often think about urban populations who don’t have health insurance, or who have problems with access to care. But let’s remember, there are many different types of health equity, and not only in cities, but also in rural communities, because systems of care aren’t in place in some of these communities, or they may not have the financial resources. Those are very real issues.
Part of it has to do with access. Are you insured, are you uninsured? Do you even have Medicaid? States that expanded Medicaid have gone a lot further down a path of making sure people can get appropriate care, such as biomarker testing and appropriate cancer care, whereas other states, including the state I’m in, the State of Georgia, has not seen fit to provide access to care through expansion of Medicaid. So that affects people in the cities and affects people in the rural areas. It affects people by educational status. How much are you able to actually interact with the system? Do you have a doctor and a care team that you know? Do you have a reasonable chance of going to a hospital? In rural communities, it’s not because the doctors don’t understand [biomarkers], but the system isn’t set up that way. So, this is a real issue.
We really do have a push for health equity to improve the quality of care that we give folks. But we, again, have those barriers, as though maybe the prior authorization may be part of the system, but the system is sometimes set up against you. And we need to have systems that are going to work for us and not against us.
EBO: What should an employer do if they’re not sure they’re offering the right coverage, or if they’re getting appeals or hearing from their staff that they’re not getting the coverage? Where’s a good place for them to begin?
LICHTENFELD: I think a good place for an employer to begin when it comes to biomarkers and genetic testing is with the CancerCare Biomarker Toolkit. That explains things in plain, simple language; it’s not a long document. It says these are the important things that you need to know about what your policies should contain. Some of us have seen the way this works. An employer buys a policy that’s off the shelf, so to speak, and they can ask what’s in the policy. Or, they can help structure the policy, which means they need to know about these elements.
Health insurance is not just “give me a check,” and particularly with large, self-insured plans there is a negotiation on what services will be covered and how much it’s going to cost. Human resources staff must speak up for their employees and say, “We think this is important. We want to make sure that our folks are covered.” Hopefully, we don’t see employers asking to not exceed a certain amount; we want adequate insurance….
The other piece is: employers must listen to their employees. And if they feel someone’s getting the runaround, then maybe the employer or benefit manager needs to step in and do the right thing.
If you thought service was included in your coverage, and your employee should have it, then you act as a backstop and help them through the process. Because there’s nothing like a phone call from the employer—who is the actual customer purchasing the contract, to help move things along. And ultimately, if people think that they’re not getting what they need, they may need to contact the state insurance commissioner if this is a commercial policy. State insurance commissioners in many states are very concerned that people get care….
This is about what we can do to help save lives. I’ve been a cancer care physician for decades, and to be in the place where we are today—years ago, it would have been a dream to think we’d have the tools to look at the cancer, the genes and the cancer cells, to be able to tell what the targets are, to be able to have treatments to help address those targets, and that we would have drugs like immunotherapy. I did research in immunology and immunotherapy—I hate to tell you, but it’s about 50 years ago. And here we are today, and it’s a reality. Think about where we were 10 or 12 years ago, and where we are today is a world of difference. But if people don’t have access to that care, if they don’t have access to the testing—it doesn’t work in the bottle—it works in people.
And getting the drugs to people is the first step. What we need is the biopsy and the testing of that biopsy to see what the biomarkers are. Or a blood test for that matter, sometimes. It helps us understand what the best treatment is for that person.
References
1. Employers’ prescription for employee protection toolkit: best practices for biomarker testing coverage. CancerCare. Accessed March 14, 2023. https://www.cancercare.org/biomarkertoolkit
2. Mason C, Ellis PG, Lokay K, et al. Patterns of biomarker testing rates and appropriate use of targeted therapy in the first-line, metastatic nonsmall
cell lung cancer treatment setting. J Clin Pathw. 2018;4(1):49-54. doi:10.25270/jcp.2018.02.00001
3. Wu N, Ge W, Quek RG, et al. Trends in real-world biomarker testing and overall survival in US patients with advanced non-small-cell lung cancer. Future Oncol. Published online January 19, 2023. doi:10.2217/fon-2022-0540
4. CancerCare releases biomarker testing toolkit for employers. News release. CancerCare. February 15, 2023. Accessed March 1, 2023.
http://bit.ly/42mXc4y
5. Understanding provider utilization of cancer biomarker testing. American Cancer Society. December 7, 2021. Accessed March 14, 2023. http://bit.ly/3JfVl8S
6. Bruno DS, Hess LM, Li X, Su EW, Patel M. Disparities in biomarker testing and clinical trial enrollment among patients with lung, breast, or colorectal cancers in the United States. JCO Precis Oncol.2022;6:e2100427. doi:10.1200/PO.21.00427
7. Hess LM, Krein PM, Haldane D, Han Y, Sireci AN. Biomarker testing for
patients with advanced/metastatic nonsquamous NSCLC in the United
States of America, 2015 to 2021. JTO Clin Res Rep. 2022;3(6):100336.
doi:10.1016/j.jtocrr.2022.100336
8. Schreiner B. Kentucky passes cancer testing mandate for insurers. Associated Press. March 14, 2023. Accessed March 16, 2023. http://bit.ly/40bf947
Insufficient Data, Disparities Plague Lung Cancer Risk Factor Documentation
September 24th 2023On this episode of Managed Care Cast, we speak with the senior author of a study published in the September 2023 issue of The American Journal of Managed Care® on the importance of adequate and effective lung cancer risk factor documentation to determine a patient's eligibility for screening.
Listen
