- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Joseph Alvarnas, MD, Discusses New CMS Drug Pricing Models, Impact for Blood Diseases
CMS in February 2023 announced 3 new models for testing by the Center for Medicare & Medicaid Innovation—all of which “aim to lower the cost of drugs, promote accessibility to life-changing drug therapies, and improve quality of care.”
Since the arrival in 2015 of direct-acting antivirals (DAAs) to cure hepatitis C virus (HCV),1 Medicare and Medicaid officials have grappled with the question: What should they do when a game-changing therapy arrives to cure a devastating disease, yet the costs exceed anything budget officials envisioned?
At the time, the cost of a full treatment course to cure HCV was $84,000, which seems quaint compared with the prices that would follow for chimeric antigen receptor (CAR) T-cell therapy, which launched at $475,000 to treat certain blood cancers.2 Opinions differed on how Medicare and Medicaid could respond, but the consensus was that the frameworks developed over many decades were not built with these drugs in mind. New concepts, such as bigger risk pools or payments over time for therapies that, in theory, should work the first time have been evaluated in recent years.3
With regulatory filings complete for the first cure for sickle cell disease, based on CRISPR technology,3 and the knowledge that the platform would be expanding to other areas including immuno-oncology, CMS in February 2023 announced 3 new models for testing by the Center for Medicare & Medicaid Innovation—all of which “aim to lower the cost of drugs, promote accessibility to life-changing drug therapies, and improve quality of care.”4 They are:
The Medicare $2 Drug List for chronic conditions, which encourages Part D plans to offer a low, fixed co-payment for a standardized list of generic drugs that treat high blood pressure or high cholesterol.
The Cell and Gene Therapy Access Model, which allows CMS to coordinate and administer multistate outcomes-based agreements with manufacturers for certain cell- and gene-based therapies that cost more than $1 million. Although it is believed that pending approval of the sickle cell treatment is the impetus for this model, it could have a significant impact in oncology and hematology.
The Accelerating Clinical Evidence Model, which calls for CMS to develop payment methods requiring evidence collection for drugs that are approved under FDA’s accelerated pathway. The model will encourage timely completion of confirmatory phase 3 studies and is designed to halt Medicare spending if drugs have no benefit.
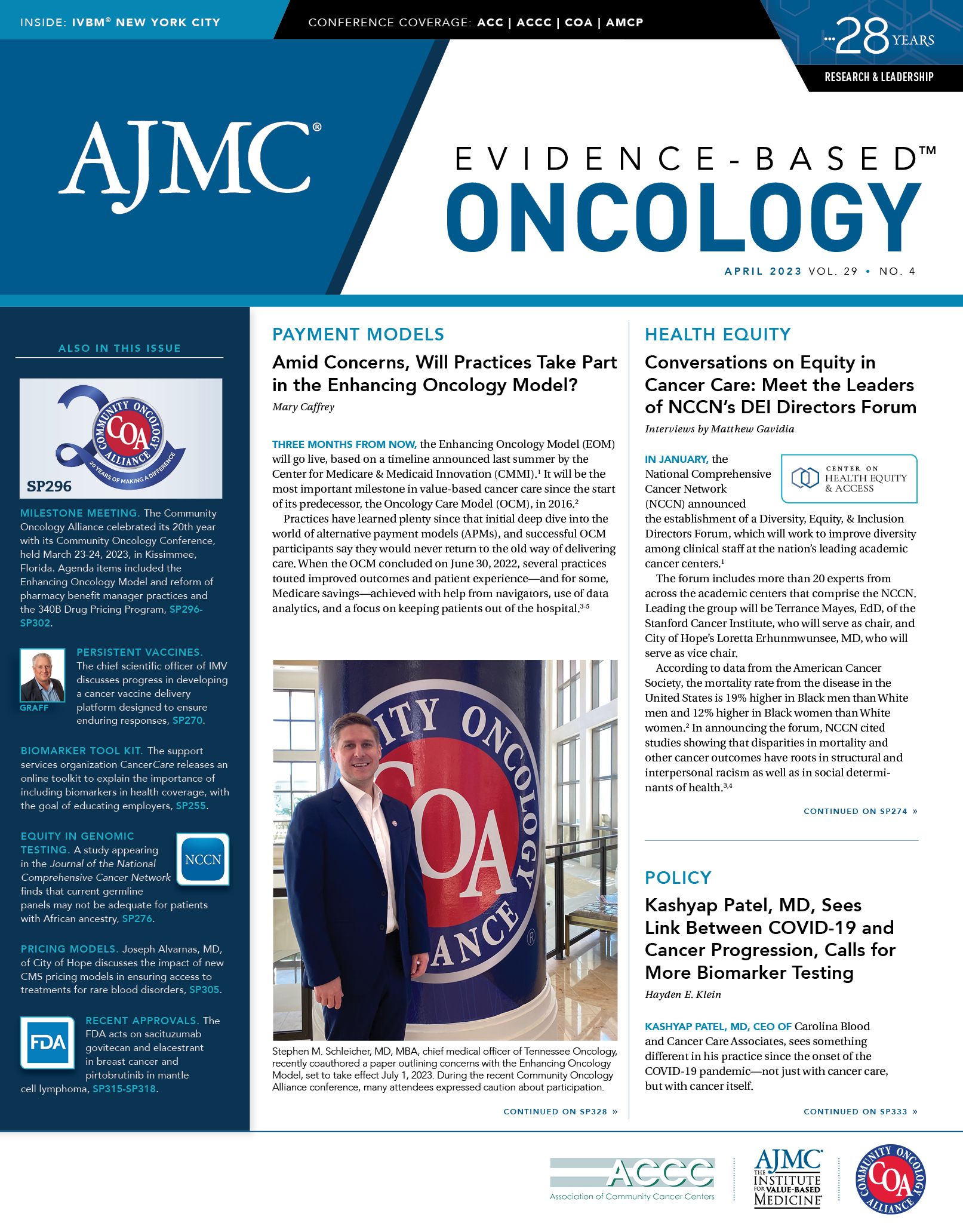
Alvarnas

Evidence-Based Oncology (EBO) spoke with Editor-in-Chief Joseph Alvarnas, MD, a hematologist and specialist in bone marrow and stem cell transplantation who is vice president of government affairs for City of Hope and chief clinical advisor for AccessHope, a National Cancer Institute–designated center in Duarte, California, about the potential impact of these models. This interview has been edited for length and clarity.
EBO: What are your thoughts on the CMS Cell and Gene Therapy Access Model?
Alvarnas: I think that this model might have the potential to be broadly applicable across a number of treatment types, including CAR T cells, emerging cellular therapeutics, and gene-based treatments for a growing number of clinical conditions. While CAR T cells have become an important part of our suite of anticancer treatments, the emergence of gene therapy–based therapeutics is another key area for clinical innovation with new treatments coming for the care of patients with sickle cell disease, β-thalassemia, and treatments for unmet clinical needs for the treatment of a number of heritable and acquired conditions.
One of the great challenges associated with the future of cell and gene therapies is that the costs associated with these emerging therapeutics will grow in unprecedented and potentially unsustainable ways. If we look carefully at the paradigm of sickle cell disease treatments, the lifetime costs of sickle cell disease treatment in the United States are roughly $1.8 million.5 While the price for gene treatments for sickle cell disease comes to the market at a purported $2.7 million,6 we need to carefully consider clinical context in how we judge drug costs. This requires a more systematic process than what the agency currently uses. The proposed CMS Cell and Gene Therapy Access Model could provide a potentially useful mechanism for ensuring that these treatments get to the patients who need them while attempting to manage the costs associated with these treatments.
EBO: One of the models is based on a principle CMS has used in the past, called coverage with evidence development. Can you discuss how this works?
Alvarnas: The challenge with new and emerging technologies is that we sometimes do not know how effective they will prove to be over time. The Coverage under Evidence Development (CED) model provides a path for coverage and payment by CMS when the effectiveness or long-term outcomes for a particular technology [are] uncertain. CMS has applied this to myeloproliferative diseases in older patients, allogeneic stem cell transplantation for multiple myeloma, and allogeneic transplantation for older adults with myelodysplastic syndromes. CMS’ intent is to use the data acquired through this process to make a final coverage decision. This model, which provides for reimbursement for technologies with potentially uncertain outcomes, creates transparency to the agency about these outcomes in a way that can make for better future coverage decisions. The goal here is to try to avoid paying for high-cost treatments if they prove to be ineffective. While this creates a significant and uncompensated administrative burden for centers offering these treatments, it also creates a model in which better quality decisions will be made around the availability and coverage of high-cost treatments. This model is extraordinarily valuable from the data-gathering point of view. Far too often in oncology, we lack high-quality data around long-term patient outcomes; the CED model is one way in which a massively important payer has created a model for getting that deeper understanding.
EBO: When you discuss the comparison of the cost of a therapy vs the cost of lifetime care, as you said, many of these therapies have been used in older patients. But in the case of sickle cell disease, the patients are often quite young. Would part of the equation be the ability of a patient to hold down a job, or return to work?
Alvarnas: The lifetime cost of care for someone with sickle cell disease averages around $1.8 million. This does not factor in the human suffering and social costs experienced by those with this condition. I suspect that these sort[s] of cost models are likely used to set benchmarks for therapeutic pricing. My personal belief is that a $2 million treatment that could cure sickle cell disease and avert both the health costs and human suffering associated with this condition represents high-value care.
As we begin to talk about therapeutics that range in cost between $2 million and $3 million, however, we do have to carefully consider how we can deliver these treatments in a sustainable way without denying necessary care for patients who may suffer potentially avertable lifelong disability and pain.
This quandary reminds me of another similar situation that arose when effective hepatitis C treatments hit the market. Remember what happened to the states when [the DAAs] Sovaldi [sofosbuvir] and Harvoni [ledipasvir/sofosbuvir] came [on] the market? A lot of state Medicaid officials said, “How are we going to pay for this?” There’s a lot of money, largely because there were a lot of people with HCV, and…it makes long-term sense financially. But boy, it’s a lot of money to put out all at once. I think Medicaid systems are kind of having that same experience, again, with sickle cell disease drugs, which will be expensive to use. As I read the instructions from HHS Secretary [Xavier] Becerra, I saw that 2 potentially impactful strategies were being laid out. One was that of federalizing the risk pool as a way of spreading risk. By federalizing the risk pool, I think you create a better way of sustainably paying for the much-needed, high-cost drugs.
The other thing that you achieve by federalizing the risk pool is that it creates immense leverage for negotiating the drug acquisition price. So, if you have a big payer who controls payment for the majority of beneficiaries, it may individually have immense leverage to acquire that drug for less, especially in the case after statutory authority to negotiate pricing has been established.
As CMS creates an ecosystem around the delivery of these kinds of therapeutics, I think that such a system may enhance care access and greater transparency around the delivery of very high-cost but potentially lifesaving therapeutics. These treatments should not be withheld from patients based solely upon their costs, but they should be delivered in a systematic way that avoids the delivering of these therapeutics to patients who will not benefit from them. These are products that I think are too expensive to use indiscriminately. I think it would be tragic to use these drugs in these patients if they’re not going to work. It’s wasted money and it’s toxicity to the patient who shouldn’t ever have to incur any toxicity. That doesn’t make sense.
EBO: Will the process of the institution or the provider knowing they must show their work, so to speak, discipline them into not providing expensive therapies to inappropriate candidates?
Alvarnas: Some institutions have invested heavily in creating robust systems for ensuring that we prospectively identify these patients carefully and make the best, evidence-based decisions on how and when to use these therapeutics.
EBO: So, could this process lead to patients getting more scrutiny and higher quality care?
Alvarnas: It could, and that’s an upside to these kinds of models. Beyond better stewardship of these technologies, expanding the base of clinical evidence for how best to use these technologies provides a huge value-add to patients, clinicians, and payers. The one complaint that I would have about the CED is that the government provides no resources for what is actually a very expensive series of activities. This is my 1 reservation with this kind of model, which is as we work, and it takes professionalized individuals to get patients’ consent, to follow their data to submit their data regularly, because these aren’t trivial data sets—they are substantial data sets—and to be able to make sure that those data [meet quality control standards] before they’re sent out. That costs money. Yes, with a model like this, you’re not getting paid for all the extra work that you’re doing.
I think there must be a way to acknowledge or defray some of the costs of infrastructure. I can tell you on CAR T cells, at City of Hope every patient gets run through a CAR T-cell committee to make sure that they meet candidacy, and that they’re getting the right product for what’s going on with them. And this system performs postadministration tracking of toxicities. And that all goes through a process of iterative feedback, into a process of iterative improvement. That represents an investment in systems of delivering better care for products, where right now…reimbursement does not always cover the cost of product acquisition.
The challenge with the CED model and even with the proposed Cell and Gene Therapy Model is that the role of the clinician and the clinical care system is undervalued; there are infrastructure and data investments that go uncompensated, and there is no reimbursement adjustment based upon delivering more effective care with better patient outcomes. This is a huge missed opportunity for the model.
References
1. Rosenthal ES, Graham CS. Price and affordability of direct-acting antiviral regimens for hepatitis C virus in the United States. Infect Agent Cancer. 2016;11:24 doi:10.1186/s13027-016-0071-z
2. Borgert R. Improving outcomes and mitigating costs associated with CAR T-cell therapy. Am J Manag Care. 2021;27(suppl 13):S253-S261. doi:10.37765/ajmc.2021.88737
3. Caffrey M. MIT group brings together stakeholders to brainstorm how to pay for curative therapies over time. Am J Manag Care. 2019;25(6):SP214-SP215.
4. HHS secretary responds to the president’s executive order on drug prices. News release. Centers for Medicare & Medicaid Services. February 14, 2023. Accessed March 14, 2023. https://www.cms.gov/newsroom/press-releases/hhs-secretary-responds-presidents-executive-order-drug-prices
5. Researchers identify high costs of living with sickle cell disease. News release. National Institutes of Health. May 16, 2022. Accessed May 14, 2023. https://www.nih.gov/news-events/news-releases/researchers-identify-high-costs-living-sickle-cell-disease
6. Lapid N. Sickle cell cure will be cost-effective if health disparities considered, study finds. Reuters. December 15, 2022. Accessed March 14, 2023. http://bit.ly/3TdEHeB