- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
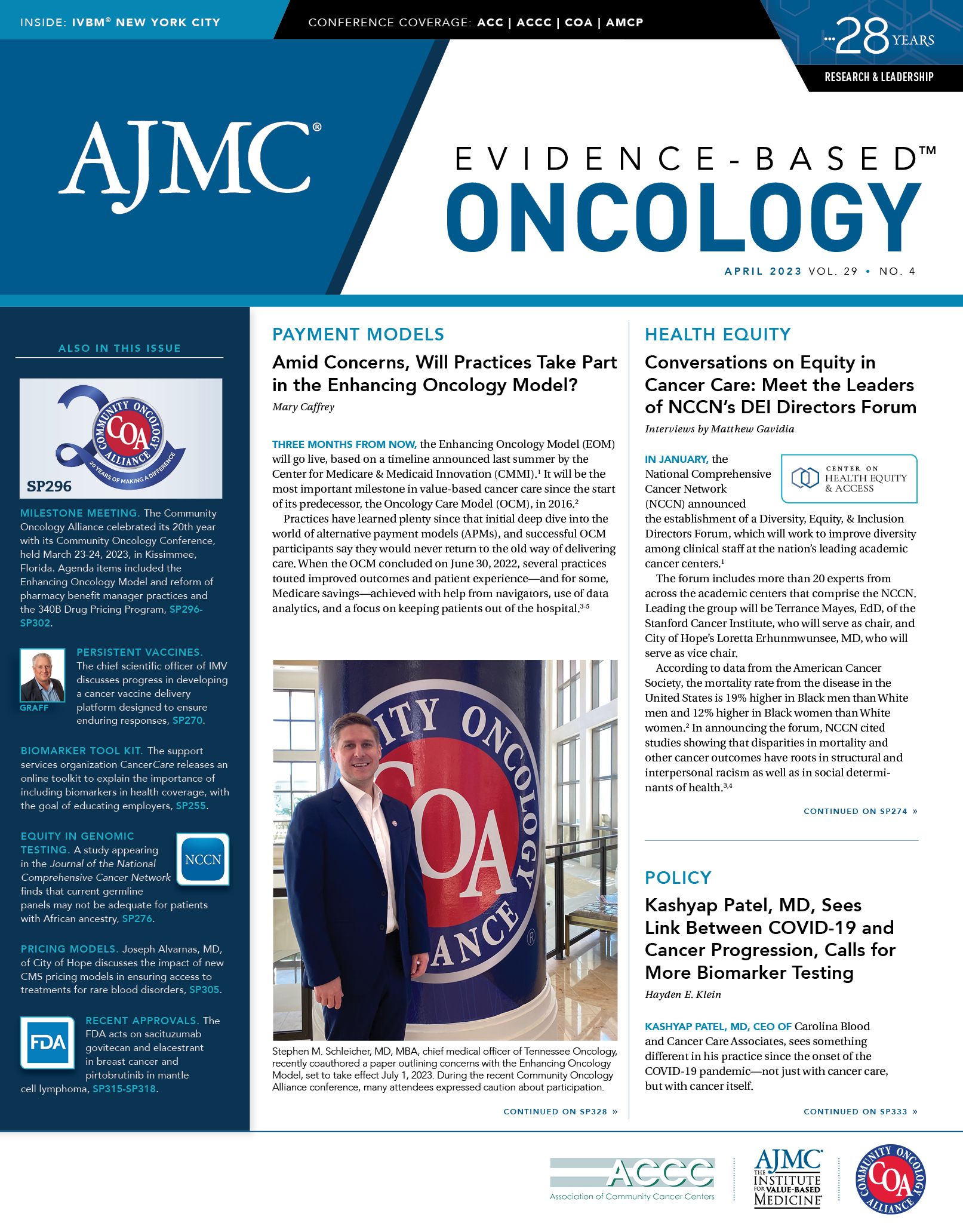
Coverage From the 2023 COA Community Oncology Conference
The Community Oncology Alliance celebrated its 20th year at the Community Oncology Conference held March 23-24, 2023, in Kissimmee, Florida.
COA: An Advocacy Group Born in Crisis Looks Back on 20 Years
The Medicare Prescription Drug, Improvement and Modernization Act (MMA) of 2003 might be best known for creating the prescription drug benefit known as Part D.1 But for community oncologists, the law felt like a wrecking ball—it drastically altered how practices were reimbursed when prescribing chemotherapy, in ways that threatened the financial health of some practices.
In this moment of crisis, a group of oncologists formed the Community Oncology Alliance (COA), which marked its 20th year at the annual Community Oncology Conference, which took place March 23 and 24, 2023, in Kissimmee, Florida. Nearly 2000 attendees overflowed the Gaylord Palms Convention Center as the 2023 cochairs kicked off the meeting.
Atkins

During the opening session, COA welcomed back most of its former presidents and featured a video with photos from early days of action on Capitol Hill, when no one knew what the group was or understood its mission. But as COA President Miriam Atkins, MD, FACP, of AO Multispecialty Clinic in Augusta, Georgia, later explained, lawmakers would learn quickly about the lives of patients who had to drive 75 miles one way for appointments or could not afford chemotherapy.
Beyond the laughs at old footage of Executive Director Ted Okon, MBA, leading a group of “dancing doctors,” a gimmick designed to grab attention, came a serious message: the MMA blindsided oncologists because members of Congress and Medicare administrators had little grasp of how community practices served patients. As Mary Kruczynski, COA director of development and strategic initiatives, put it during the video, “These guys have no idea what we do.”
And so, engagement began in earnest. Today, COA is well known in Washington, DC, and has been a resource for the Federal Trade Commission in its investigation of unfair practices by pharmacy benefit managers (PBMs).2 When a Senate committee recently held a hearing on prior authorization and PBMs, COA Vice President Debra Patt, MD, PhD, MBA, a breast cancer specialist who is an executive vice president of Texas Oncology in Austin, testified about her recent experience of waiting 4 weeks for a peer-to-peer consult. Patt had to use chemotherapy instead of a preferred innovative regimen, and the patient later died.
In many ways, its leaders say, COA retains the spirit of an upstart advocacy group while working to look ahead at innovative technologies, care delivery trends, and other events that threaten independent practices.
“New government policies, many of which we’ll hear about at this conference, including the Inflation Reduction Act [of 2022] or the Enhancing Oncology Model, are poised to change many parts of the health care system with which we operate,” said meeting cochair Stephen M. Schleicher, MD, MBA, chief medical officer of Tennessee Oncology, practicing in Lebanon. “Throughout all this, constantly, the control variable as independent community oncologists is the willingness to transform, adapt, and evolve to meet the challenges of the day.”
Next came a panel discussion, “20 Years of COA: The Value of Community Oncology,” featuring Okon; Atkins; Lucio Gordan, MD, president, Florida Cancer Specialists & Research Institute; Barbara McAneny, MD, CEO of New Mexico Cancer Center; and Jeffrey F. Patton, MD, CEO of OneOncology and chairman of the board, Tennessee Oncology.
The panelists agreed on several points:
- Community oncology provides care closer to patients and more efficiently, with data to prove it.
- The recent focus on health equity is old news for community oncology—practices have been helping underserved patients and those with limited resources for decades.
- Community practices are offering patients access to clinical trials and can get a trial up and running faster than counterparts in academic medicine.
“We deliver equity. We have offices everywhere,” Gordan said. “We take care of patients with all types of insurance and uninsured patients.”
He pointed to research he coauthored that shows community practices spend thousands less per month per patient compared with hospitals on cancer treatment, both for chemotherapy and total cost of care.3
McAneny said that when she arrived in New Mexico as a young oncologist, she soon observed the same problems with the health care delivery system across many patients. In 2003, she joined an American Medical Association physicians’ committee that was supposed to advise an HHS secretary—who did not necessarily want their advice. McAneny said she learned that some physicians had to take a leadership role not just in treating patients but also in being their advocates.
“People don’t hand you power,” she said. “You actually have to stand up and say, ‘I’m speaking for people who cannot speak for themselves.’”
She said her mantra became “follow the money,” and this has remained so. McAneny has spoken out against abusive behavior by PBMs as well as data-gathering requirements from the Center for Medicare & Medicaid Innovation that she worries will alarm the Native American patients she serves; McAneny has said in many forums that this patient group sees sharing information with the government as a signal that they might lose property or benefits.
“If a patient comes in and says, ‘I have to decide between chemotherapy and putting food on the table for my kids or my rent,’ we are the ones who find the money to pay the rent,” McAneny said. Hospitals, she said, typically do not offer such assistance.
Atkins agreed. She described the behavior by hospitals that have taken advantage of the 340B Drug Pricing Program, intended to help safety net hospitals acquire drugs at discount prices so they could afford to care for the uninsured and other underserved patients. In her area, a hospital took over another area clinic and let all referring primary care physicians know to send patients to her competitor.
If it came down to it, Atkins said, “We will shut the door before we sell to the hospital.”
Patton said the role of COA is to give community oncology physicians a voice they lacked in other organizations. The American Society of Clinical Oncology (ASCO) is a giant organization with many constituencies, some in direct conflict with the community practice.
“In 2003 and 2004, we didn’t have a voice,” Patton said. ASCO, he said, has certain conflicts. Without COA, he said, the situation for community oncologists would be even more dire. The percentage of chemotherapy administered in physician-owned practices has been cut in half over the past 20 years, he said, even though costs are lower for payers and for patients. The financial strain on practices is enormous and constantly shifting, he said.
“We have past presidents [of COA] who, not by choice but by necessity, have joined hospital systems,” Patton said.
The amount of money involved in cancer care makes it attractive to those who do not deliver care to find a way into the revenue stream, he said. “It’s a huge business, so the middlemen come in to get a slice of the pie.”
Gordan highlighted the positive contributions community oncology has made to the advancement of treatments, noting that his practice has participated in trials for 87% of the new cancer drugs approved by the FDA in the past 10 years. Plus, the community practices can do this at a lower cost.
McAneny said the call for health equity—and more diversity in trials—could mean that is an important path forward for practices. The nimbleness of community practices in setting up trials should be attractive to pharmaceutical sponsors now that the FDA is requiring proof of diversity in trial enrollment.
“The community is an untapped resource.,” she said. As practices look for new revenue streams, trials offer opportunities for business stability along with better patient care. “As COA evolves, we will remain an advocacy organization because we have to have that voice. But we also are going to need to figure out how to teach more and more oncologists how to manage practices and how to remain independent.”
References
1. Medicare Prescription Drug, Improvement, and Modernization Act of 2003, HR 1, 108th Cong (2003). Accessed March 23, 2023. https://www.congress.gov/bill/108th-congress/house-bill/1
2. FTC launches inquiry into prescription drug middlemen industry. News release. Federal Trade Commission. June 7, 2022. Accessed March 23, 2023. https://bit.ly/3uDbHle
3. Gordan L, Blazer M, Saundankar V, Kazzaz D, Weidner S, Eaddy M. Cost differences associated with oncology care delivered in a community setting versus a hospital setting: a matched-claims analysis of patients with breast, colorectal, and lung cancers. J Oncol Pract. Published online October 31, 2018. doi:10.1200/JOP.17.00040
As Decision Time on EOM Nears, COA Panel Has Many Questions
To open the discussion on payment reform at the recent Community Oncology Alliance (COA) 2023 Community Oncology Conference, moderator Judith Alberto, MHA, RPh, BCOP, the director of clinical initiatives for COA, asked several times for a show of hands.
How many in the room had taken part in the Oncology Care Model (OCM)?
Hands went up around the room.
How many had applied to take part in the Enhancing Oncology Model (EOM)?
A few more hands joined them.
Finally, how many were planning to join the EOM if they received a participation agreement from the Center for Medicare & Medicaid Innovation (CMMI)?
Hands fell everywhere.
Alberto

That summed up sentiment about the EOM among oncologists and practice administrators attending the COA meeting March 23 and 24. When the EOM was presented in late June 2022, many practices had hoped by this point they would be saying yes to the model.1 This was especially true among those who spent years fine-tuning their performance in the OCM, which for 6 years was Medicare’s chief way for oncologists to take part in an alternative payment model under the 2015 Medicare Access and CHIP Reauthorization Act.2
But as the July 1, 2023, EOM implementation date nears, questions remain, and Alberto and her fellow panelists explored many of them. Joining her were T.R. Strickland, a value-based care consultant whose company is called StrictlyHealth Consulting; Anne Marie Rainey, MSN, RN, CHC, director of quality and value-based care for Clearview Cancer Institute, based in Anniston, Alabama; and Matthew R. Skelton, MD, an oncologist with Blue Ridge Cancer Care, based in Roanoke, Virginia.
Rainey and others at the COA meeting say participation agreements that were anticipated weeks ago from CMMI have yet to materialize, making it hard for practices to know what they are agreeing to do if they want to proceed.
Those on hand have many concerns, but chief among them is the EOM requirement to take on downside risk from the outset—something that the OCM did not do. However, as the panelists explained, not joining the EOM carries its own risk, as many believe that CMS will someday make risk-based reimbursement mandatory; thus, time spent in the EOM will be a worthwhile investment.
The cultural change achieved over 6 years in the OCM was hard won, and no practice wants to backslide, the panelists agreed. A major consideration for taking part in the EOM, Skelton said, is “if you don’t do it, you’re going to be left behind.”
Retaining the patient-centered approach that the OCM promoted is key, Rainey said. “If we focus more on the patient and keeping the patient in the center and doing what’s right from the start, then that puts us on the best trajectory to solve some of the problems that we have,” she said.
EOM Alongside Other Concerns
Deciding whether to join the EOM would be monumental enough if it were the only major action coming from CMS, but it is not. As Strickland noted, practices are also figuring out the near-term impact of the Inflation Reduction Act of 2022, as many practices still have most of their revenue tied to fee-for-service models.
CMS and health plans are also aggressively marketing Medicare Advantage plans to retirees, and oncologists continue to report issues with step edit requirements in these plans that prevent them from giving patients the best therapy available. Oncologists may be required to use older, less effective drugs before trying newly approved therapies, regardless of the available evidence, in what some call a “fail first” strategy.
The panelists expressed frustration that the OCM ended just as practices had finally mastered its nuances. Skelton cited updated figures from The US Oncology Network, of which Blue Ridge is a part, that showed these practices saved Medicare more than $300 million, of which the member practices retained one-third of this amount. (An earlier estimate based on fewer performance periods, which appeared in Evidence-Based Oncology™, put the savings at $240 million.3)
“And on top of that, patients are doing better. That should be first and foremost,” Skelton said. Data show that patients spent less time in the hospital and pursued hospice earlier. “That turned some skeptics around,” he said.
Practices have many concerns about the EOM, Rainey said. Although critics say the model asks practices to do more and be paid less, Rainey was less harsh. But she did outline some of the challenges.
Practices will receive less in monthly per-patient stipends to cover services such as patient navigation or 24/7 access to health records; however, they will face a host of new reporting requirements on social determinants of health.
Rainey said the data gathering requirements, including the call for collecting electronic patient-reported outcomes data, cannot be performed by an entry-level employee. “That’s an expensive staff member,” she said.
However, the panelists had doubts that the requirement to take on downside risk was responsible or fair to practices that had no experience with value-based care, if CMS plans to make this type of payment system mandatory.
Alberto asked the panelists what they might change about the EOM as currently designed. Rainey was specific: Give practices the first performance period without downside risk. “This is a chance to get some data to see how it performs,” she said.
Although former OCM practices have some knowledge, they will have far fewer patients in the model—due to the EOM’s limit to 7 cancer types. “We just don’t know exactly what that’s going to look like with a smaller patient population,” she added.
At this stage, Rainey said, CMMI may want to reconsider the timeline for the EOM.
For example, Rainey’s practice is “very on the fence” about the EOM because it has acquired 3 locations that were not part of the OCM. Giving those locations an initial period to collect data before taking on risk would increase the practice’s comfort.
Skelton agreed. “Two-sided risk right out of the gate is a disincentive,” he said, if the goal of CMMI is “a solution for the country and not just super high-performing practices.” He noted that even the most successful OCM practices took 3 to 4 performance periods—which were 6 months each—to learn to work the model.
Strickland noted that after the early performance periods, CMMI changed methodology based on feedback, and then practices were finally able to see their data—and performance improved. “Value-based care is usually built in a progressive manner,” he said.
Both Strickland and Rainey said practices are considering tapping into the chronic care management model, which could replace revenue being lost due to reduced monthly payments under the EOM.
To conclude the session, Alberto asked the panelists what is preventing the health care system from putting oncology care where it wants to be.
Rainey said technology to help with decision-making is still not optimal, and Strickland agreed that more must be done to make collaboration seamless.
Skelton said physicians feel “resentment” when third-party payers dictate what therapies they can use, and so much time is wasted doing battle to work through prior authorization just to give patients guideline-directed care. As frustrating as it is, he said, physicians must advocate for their patients, because “who else is going to do it?”
References
1. Enhancing Oncology Model. Centers for Medicare & Medicaid Services. Updated March 6, 2023. Accessed March 24, 2023. https://innovation.cms.gov/innovation-models/enhancing-oncology-model
2. MACRA. Centers for Medicare & Medicaid Services. Updated April 1, 2022. Accessed March 24, 2023. http://bit.ly/3LP2Fv6
3. Staggs S. New Enhancing Oncology Model builds on knowledge from the OCM. Am J Manag Care. 2022;28(Spec No 6):SP405.
Could This Be the Year for PBM Reform? COA Panel Weighs In
Leaders of the Community Oncology Alliance (COA) have spent years sounding the alarm about unfair practices by pharmacy benefit managers (PBMs), only to see vertical integration of these entities with payers make prior authorization even more challenging for oncologists.
But Capitol Hill experts taking part in COA’s Community Oncology Conference on March 24, 2023, said that bipartisan awareness of PBM practices has reached a point where they believe the US Congress may finally act, if only to require greater transparency.
Okon

Moderated by COA Executive Director Ted Okon, MBA, the legislative update is a highlight of the annual conference, and this year’s session featured the following panelists:
- Christian G. Downs, JD, MHA, executive director, Association of Community Cancer Centers
- Ben Jones, vice president, government relations and public policy, The US Oncology Network
- Jerrica Mathis, director, government relations, Cardinal Health
- Kristine Rufener, director, congressional affairs, American Society of Clinical Oncology
- Tony Lee, director of public policy, AmerisourceBergen
The group agreed that no one should expect a piece of legislation on par with the Inflation Reduction Act (IRA) of 2022, which community practices are still sifting through as they work to understand how providers will be affected. But longtime COA priorities such as PBM and 340B reform are gaining traction, they said. Despite the divided Congress, with Republicans controlling the US House of Representatives and Democrats running the US Senate, there is interest in bipartisan work when the parties can find common ground.
“Who had on their bingo card that banning TikTok would be bipartisan?” Mathis said. On a serious note, she added that there is interest in extending the flexibilities offered during the COVID-19 public health emergency—such as telehealth in Medicare—and in greater transparency across health care. Mathis sees issues of pricing and access gaining bipartisan attention.
Downs agreed that the health care items settled this year will be those “on the margins,” but PBM reform could make the list. “I think there’s space there right now,” he said. With some issues, he added, “It doesn’t matter if you’re an R or a D; you hear about it from your constituents.”
On the eve of the conference, the Senate Commerce Committee voted 18 to 9 on March 22, 2023, to advance the PBM Transparency Act of 2023, sending the bill to the full Senate.1 It would address lack of transparency, including such practices as direct and indirect remuneration fees and clawback fees, which have been burdensome for oncologists.
A key dynamic of the current session of Congress, Jones said, is that the partisan makeup of the House and Senate—and the slim margins in each—were not anticipated going into the November 2022 election. “No one expected us to be here,” he said, and there is nothing typical about the current environment.
However, that can work for an issue such as PBM reform, which finds supporters as politically diverse as Sen Ron Wyden (D-Oregon) and Rep Earl L. “Buddy” Carter (R-Georgia). Jones noted that the IRA had only just been settled when Wyden said PBM reform would be his next priority.
Okon said legislators are gaining awareness of the effects of vertical integration, and the resulting behavior by PBMs in areas such as prior authorization. He recapped COA’s recent visit to a Senate hearing at which Debra Patt, MD, PhD, MBA, vice president of COA and executive vice president of Texas Oncology, recounted her experience of being unable to give a young patient with aggressive breast cancer an innovative regimen she thought would offer the best chance of survival. Told she would have to wait up to 6 weeks for a peer-to-peer consult, Patt started the patient on chemotherapy instead. After the hearing, Patt learned the patient died.
“You get robbed of hope,” Okon said.
Implementation of the IRA
This law is designed to bring patients relief through several measures, including Medicare price negotiations and other steps to put downward pressure on drug prices. Not only does this fail to appreciate that oncology providers are still reimbursed based on average sales price (ASP) of therapies plus 6%, but it calls for payment of Part B drugs with negotiated drug prices to be compensated at average fair price plus 6%.2
“It’s particularly not good when providers are caught in the middle, because it’s going to artificially drag down to ASP in the Medicare market,” Jones said, reducing the add-on fee “without any costs going down on your end,” he said.
At the same time, Medicare is imposing cuts in physician payments, due to the 2015 Medicare Access and CHIP Reauthorization Act, which Jones said simply does not speak to the higher costs and staffing challenges of the post–COVID-19 era. “It’s not as though because of the IRA, it just magically became cheaper to deliver care,” he said.
Rufener agreed with Okon’s suggestion that the IRA’s good intentions add up to “unintended consequences” in the potential effects on oncology providers. “We all want to see drug prices come down; we want to see patients having access to the treatments that they need. And obviously we support that,” she said. “But where it gets tricky is…when the provider [feels like] they’re getting caught in the middle.”
Lee said one of the puzzling aspects of the IRA is that is it highly proscriptive in some areas and much less so in others. AmerisourceBergen is closely watching implementation of elements related to Part B pricing, he said, noting that some provisions “might go counter to the Cancer Moonshot Initiative.”
“So, that reflects the tension within the [Biden] administration,” he said.
340B reform
The panelists agreed that the atmosphere surrounding this issue has shifted markedly since articles in The New York Times and The Wall Street Journal explained to a wider audience how use of a provision to support safety net hospitals has become a profit center for some hospitals.3,4 Okon emphasized that COA does not oppose the idea behind the 340B Drug Pricing Program—it just wants to see the discounts follow the underserved patients.
Drug companies that had to offer therapies at discount to qualifying entities have pushed back as well, and the US Court of Appeals for the Third Circuit recently ruled in favor of drugmakers that they can restrict health systems’ use of contract pharmacies.5
Downs predicted that this issue would see movement, but that the action will come first outside the legislative arena. “I think you are going to see some business things happen,” he said. Downs and Jones discussed that it remains unsettled who enforces 340B once an entity qualifies, and the courts seem poised to settle the question.
Mathis predicted that despite the recent momentum, a final solution on PBM reform will await a report from the Federal Trade Commission, which opened an investigation into PBM practices in June 2022.6
Jones said he is optimistic about resolution on the long-term COA priorities of PBM and 340B reform. He and Downs credited Okon for bringing these topics into “mainstream conversation.” When he meets with members of Congress to discuss 340B, Jones said, he no longer spends 20 minutes explaining what the program is. “We’ve eclipsed that first hurdle to having a serious conversation.”
The issues that COA has championed are ones that only Congress can fully resolve, but that message is breaking through. “I am a little more glass half full for the potential for reform,” he said.
References
1. King R. Senate panel advances bill to reform PBMs and bring more FTC scrutiny on industry. Fierce Healthcare. March 22, 2023. Accessed March 24, 2023. https://bit.ly/3Zhv4Na
2. Cubanski J, Neuman T, Freed M. Explaining the prescription drug provisions in the Inflation Reduction Act. Kaiser Family Foundation. January 24, 2023. Accessed March 24, 2023. http://bit.ly/3LRihhr
3. Thomas K, Silver-Greenberg J. How a hospital chain used a poor neighborhood to turn huge profits. The New York Times. September 24, 2022. Accessed March 12, 2023. https://bit.ly/3DdPiiS
4. Mathews AW, Overberg P, Walker J, McGinty T. Many hospitals get big drug discounts. That doesn’t mean markdowns for patients. The Wall Street Journal. December 20, 2022. Accessed March 24, 2023. https://on.wsj.com/3lJpc1y
5. Pifer R. Court rules for drugmakers over HHS in 340B fight over contract pharmacies. Healthcare Dive. January 31, 2023. Accessed March 24, 2023. http://bit.ly/3lPfdI2
6. FTC launches inquiry into prescription drug middlemen industry. News release. Federal Trade Commission. June 7, 2022. Accessed March 24, 2023. https://bit.ly/3uDbHle
Community Oncology Offers Nimbleness for Pivot to Value-Based Care
When the University of Washington released its first set of core health data among the state’s oncology providers several years ago, the top performers were not the well-known academic centers certified by the National Cancer Institute.
Instead, the practice that stood apart was Northwest Medical Specialties, and soon the big institutions were calling on its medical director, Sibel Blau, MD, to learn how to deliver high-quality care with her level of cost-effectiveness.
“Our medical home initiative started in 2013. By 2015, we had the first commercial payer initiative,” Blau said. That led to more recognition; today, her practice has pursued a joint venture with a hospital that helps that larger entity improve its contracting processes.
Payers benefit from this collaboration, she said, because no matter who is providing the care, it saves money if providers have value-based contracts and follow pathways. “It’s my practice that’s going to get the shared benefits,” Blau said.
Her story offered just one example of how community oncology practices can be laboratories for innovation in care delivery, during a March 23 session at the 2023 Community Oncology Alliance (COA) Community Oncology Conference, held in Kissimmee, Florida. The session, “Thinking Outside the Box: Going Beyond the Traditional Model of the Community Oncology Practice,” allowed Blau and 3 other practice leaders to share how they continue to work on ways to deliver better care by offering just the right drugs or procedures, not the most.
Moderated by Stephen “Fred” Divers, MD, of Genesis Cancer and Blood Institute in Hot Springs, Arkansas, and the chief medical officer for the American Oncology Network, the panel also featured Alti Rahman, MBA, MHA, CSSBB, practice administrator for Oncology Consultants of Houston, Texas; and Brad Hively, CEO of The Oncology Institute of Hope and Innovation, which has practices in 5 states.
The Oncology Institute offers physicians a national network to participate in value-based models, including those at full risk. Hively said making the shift to value-based reimbursement requires extreme care in contracting, because otherwise the practice is doing all the work to save money and the payer gets all the benefit.
“The average oncologist in this country writes between $8 million and $10 million in [chemotherapy] per year. Our average oncologist writes between $4 million and $5 million per year,” he said. “If you shift from volume to value without the appropriate reimbursement methodology, you crush your profitability. So, it’s a delicate balance.”
“Oncology risk is scary,” Hively said. The therapies are expensive, new ones are approved all the time, and it can be hard to predict which ones will dominate. A group such as the Oncology Institute helps physicians by managing the risk and spreading it across a wider pool of patients. “We’re up to 1.8 million lives under capitation, and so we’re very well positioned to take that risk.”
“For smaller oncology groups that are thinking about taking on risk, volume is really important in terms of number of patients,” he continued. “So, we have to think about ways to come together and work together. That’s the name of the game in taking risk; you’ve got to be able to spread it over a large population.”
For Rahman, understanding the local market is key. “What does the overall health ecosystem look like?” he asked. Houston, where his practice operates, is the fourth-largest US city, very diverse, and home to multiple payers—none of which control more than 14% of the market. Managing multiple value-based contracts for various payers is difficult, but Rahman said it is necessary. “If we’re going to work with payers, no one payer commands the population,” he said.
The proliferation of Medicare Advantage is a key development. Many academic centers refuse to accept this coverage, and community oncology can fill a void for these patients by learning to work with these plans, Rahman said.
“We’re one of the very few practices in our county that takes the majority of those plans—that’s a barrier to access right there,” he said. “We don’t have the marketing dollars that some of our very, very large institutions have, but at the end of the day, no amount of marketing dollars [is] going to matter if you walk when you call that institution and they say, ‘Well, you don’t qualify to come here.’”
Beyond the contracts with different payers, Divers said, “It’s going to become more and more important in community oncology to champion that value proposition.” He asked fellow panelists to discuss the different components of making value-based care work, such as technology, data analytics, and staff buy-in.
Rahman’s journey with data analysis at Oncology Consultants began when his practice got bad news. In 2008, the director of contracting asked him to help find solutions after the practice had been deselected by Blue Cross Blue Shield. “At that time, there was no risk stratification, there was no kind of this emphasis on [hierarchical condition category] coding, or how do you look at staging—none of that was there,” he said. The insurer “simply deselected our practice, because our cost per cancer was too high, just per cancer.”
The more he worked with the numbers, the more Rahman realized that value-based care requires people like him—who love getting into the weeds to find areas for improvement—alongside physician and nursing leaders who can translate the numbers into what they mean for the lives of patients.
When Rahman joined his practice as an intern, he fully embraced the focus on data, but he acknowledged, “There’s no way that you can look at the complex methodologies around oncology actuarial studies and [say], ‘You know what, this is exciting. This is something I’m going to talk about at parties.’ ”
t takes physicians and nurses to carry the message of what the data mean in terms of improving quality. Rahman said, “You have to pair it with ‘what’s the experience of the patient?’ And that’s really where the magic happens.”
Blau agreed. She also pointed to the value of being part of COA and the Quality Cancer Care Alliance (QCCA), a clinically integrated network of independent practices for which she serves as president and CEO. The QCCA came together in 2018, after the Oncology Care Model (OCM) took flight.
Since then, Blau and other practices have also formed a research collaborative to help patients enroll in clinical trials.
“During the OCM we used artificial intelligence tools, we used different data analytic tools, but also our experience and experience from other groups.
And this is one of the benefits of working within a network when we shared some data analytic tools. Those practices opened up their data—I didn’t care if they saw that I did something wrong, because of what we learned from other practices and what they learned from us,” she said.
“This is an ongoing process,” Blau said. “It’s not going to stay where we are today.”