- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
EOM Payments Are Not Sufficient to Achieve Health Equity Goals
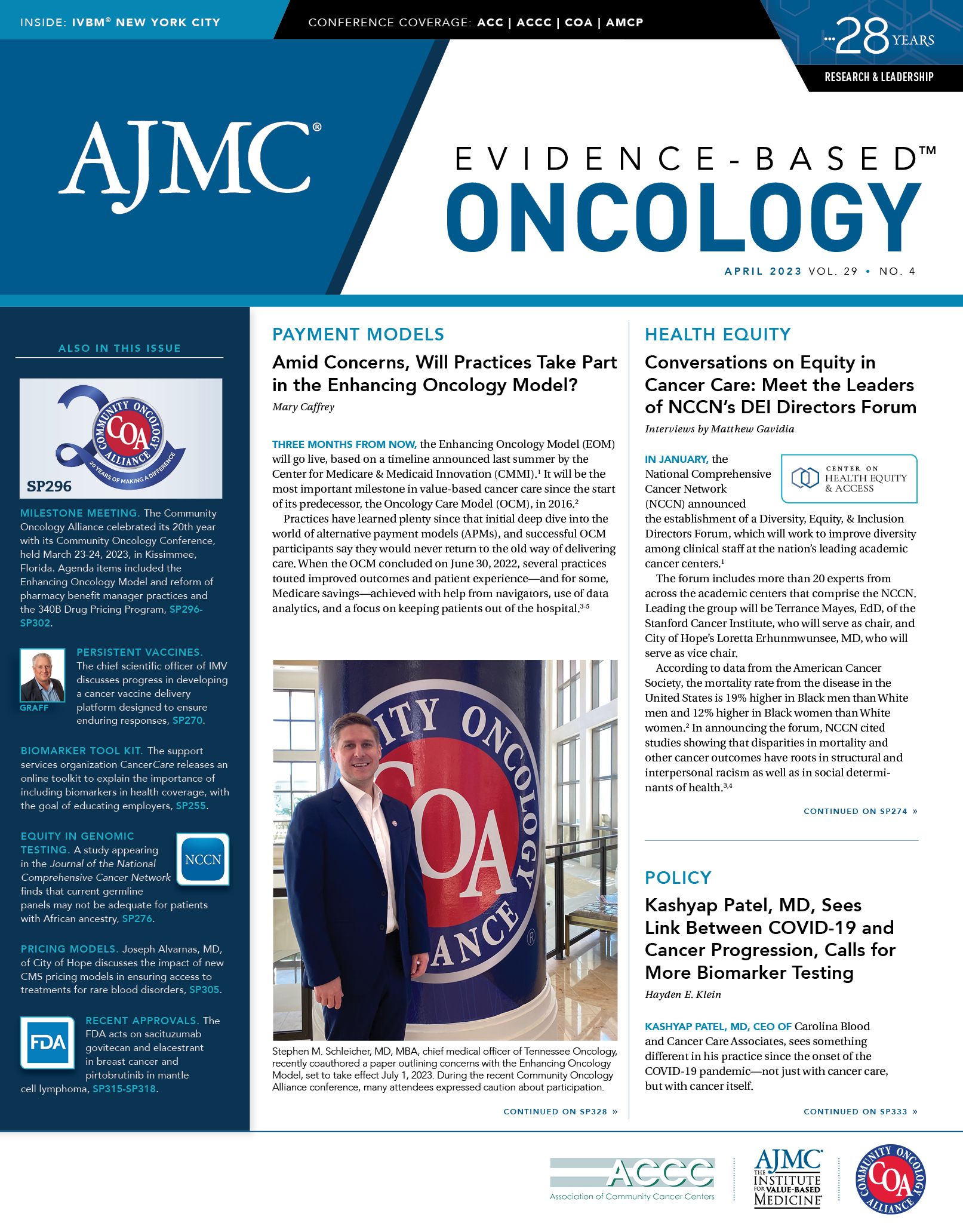
The CEO of Carolina Blood and Cancer Care Associates discusses challenges with the proposed Enhancing Oncology Model.
In 2016, my practice, Carolina Blood and Cancer Care Associates, embraced the Oncology Care Model (OCM) in both letter and spirit. For the patients we serve in the counties around Rock Hill, South Carolina, the OCM offered an opportunity to care for the whole person—by rewarding practices that provided advanced care planning, survivorship care, and extended-day options to keep patients out of the hospital.
Kashyap Patel, MD

Our practice partnered with urgent care providers, increased our use of biosimilars, and trained staff to multitask to provide the required services. As the OCM wound down, we took the additional step of creating a program, No One Left Alone, that addresses financial toxicity by dedicating staff to help patients qualify for financial assistance or free drug programs offered by pharmaceutical companies.1 We have formed research partnerships to help our patients gain access to genomic testing.2 With all 5 counties in our primary catchment area reporting median incomes well below the US median income level,1 our efforts have helped address cancer care disparities for patients we serve.
Today, however, our practice is at a crossroads. The Enhancing Oncology Model (EOM), set to start July 1, 2023, has a goal of improving health equity, a mission that was not part of the OCM.3 For physicians dedicated to reducing disparities, this is a welcome change. But the financial pieces of the EOM do not give practices like mine the resources to achieve this goal. Like other smaller practices, we face a choice of pursuing the EOM—and taking on risk that could be challenging to manage—or pursuing our goal of addressing health equity outside of the major oncology alternative payment model (APM) offered by Medicare.
As detailed in the Table, changes to the formula for Monthly Enhanced Oncology Services would cause our annual payments to fall from the $307,200 a year seen in OCM to an estimated $50,400. (These data are based on average patient totals, which vary from month to month.) With these reduced funds, our practice would be asked to provide all the enhanced services we now provide, along with new requirements. Notably, our practice would be asked to collect electronic patient-reported outcomes in a service area where many patients lack a phone with texting capability.
TABLE.
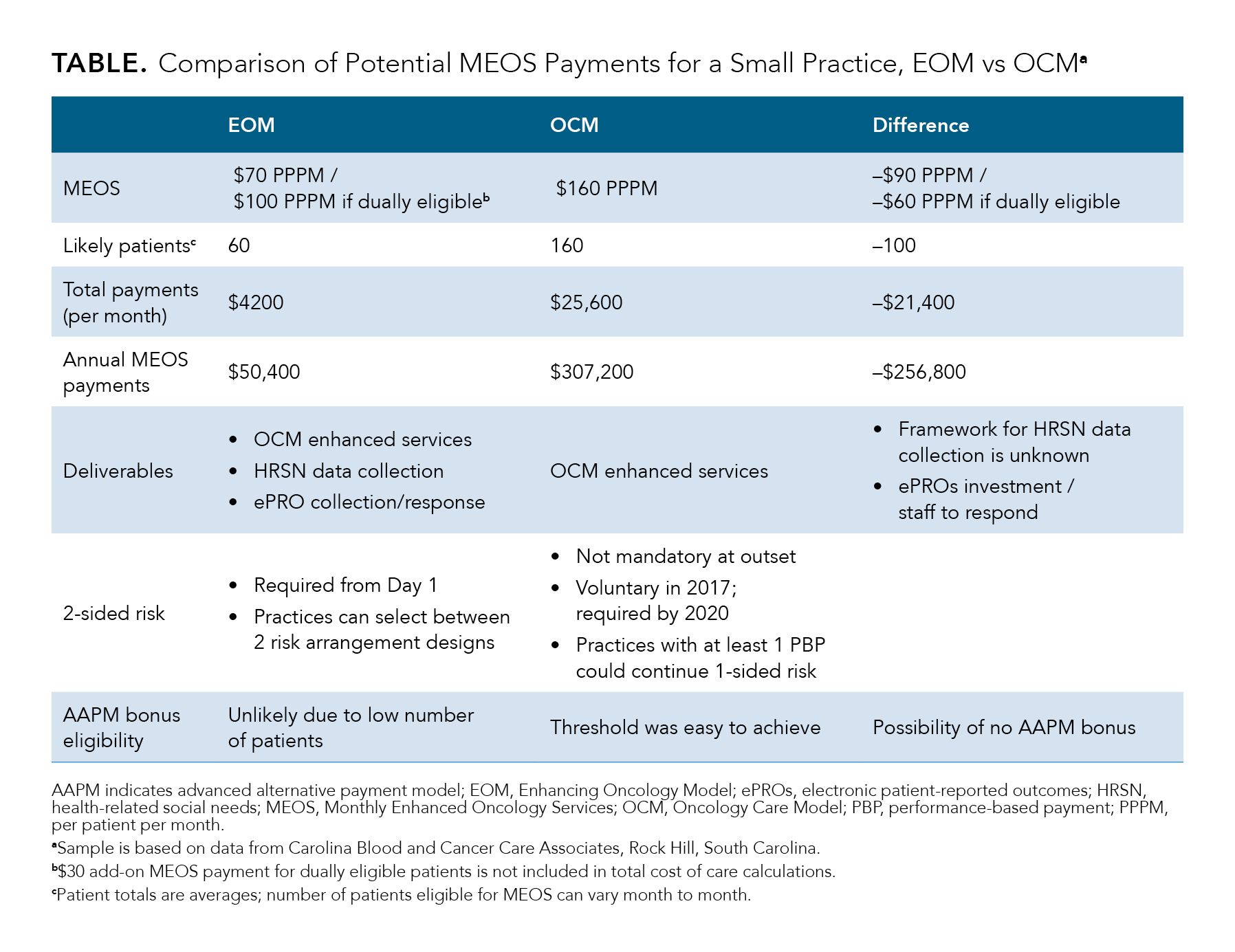
The reduced per-patient amount—from $160 to $70, with an extra $30 for patients who are dually eligible for Medicare and Medicaid—is not the biggest challenge. The Center for Medicare & Medicaid Innovation (CMMI) decision to provide payments only for Medicare beneficiaries with 7 common cancer types creates the perception that not all cancers are equal. Yet we physicians know that the burden of cancer does not discriminate between those with the cancer types included in the EOM, such as early-stage breast and prostate cancer, and rare, deadly conditions such as cholangiocarcinoma, which are excluded. With a pricing difference of up to 10% to 15% between males and females, with newer therapies, that gap may change.
Requiring practices to collect data on health-related social needs without a precise plan for what to do with these data puts the physician in a bind. Once I ask patients whether they lack food or housing, I carry the moral burden of addressing this issue—asking these questions creates the expectation that something will be done. But as designed, the EOM provides fewer resources to address the social challenges many of our patients face.
There is a path forward, and it can be achieved largely within existing frameworks of CMMI. Adoption of these ideas could make the EOM more attractive, especially to small, rural practices lacking the economies of scale or resources seen in large networks. CMMI should do the following:
- Allow providers to be reimbursed by using codes for the chronic care management (CCM) model that address health-related social needs. This is permitted if the patient in question is not eligible for EOM, but it should be permitted for all patients. This step alone could cover 30% to 50% of patients, and it would be an essential element in reducing cancer care disparities. As with the proposed add-on payment for EOM patients who are dually eligible, use of CCM codes has already produced better outcomes and reduced monthly spending for Medicare beneficiaries.4,5
- Reward practices that take extra steps to reduce disparities and promote health equity, which will provide resources to take on this challenge.
- Have the EOM cover patients with all types of cancer. This sends a message that the model is truly inclusive and promotes better care, and not just a way of saving money.
Have both proposed risk arrangements start on the day a practice joins the model. However, for smaller practices, the anticipated reduction in eligible patients would make it unlikely that the practice could qualify for an advanced APM bonus. To encourage practices to enroll in Risk Arrangement 2, which has greater potential rewards and greater stop loss, CMMI should eliminate thresholds to qualify for the APM bonus under this risk design.
Eliminating cancer care disparities is my passion. I will not stand by when I see statistics such as those reported by the American Association for Cancer Research (AACR) that show the impact social factors have on patient outcomes. AACR’s report tells us that 34% of cancer deaths could be prevented if socioeconomic disparities were eliminated.6 Both the Community Oncology Alliance and the American Society of Clinical Oncology have made health equity a priority. CMMI should join us and give practices on the front lines the resources to achieve this worthy goal.
Author Information
Kashyap Patel, MD, is the CEO of Carolina Blood and Cancer Care Associates in Rock Hill, South Carolina, and the immediate past president of the Community Oncology Alliance. Patel is the associate editor of Evidence-Based Oncology.
References
1. Patel K, Mukhi H, Patel A, et al. Addressing cancer health disparities in a multilateral collaboration in an independent community cancer clinic: translating words into action. Am J Manag Care. 2022;28(6 Spec No.):SP398-SP401. doi:10.37765/ajmc.2022.88856
2. Patel K, Mukhi H, Mehta D, Patel A, Oh W, Reddy P. Incorporating biomarker testing in community cancer clinics: a real-world pilot study. Targeted Therapies in Oncology™. 2022;11(7):16.
3. Enhancing Oncology Model. Center for Medicare & Medicaid Services. Updated March 6, 2023. Accessed March 28, 2023. https://innovation.cms.gov/innovation-models/enhancing-oncology-model
4. O’Malley AS, Sarwar R, Keith R, Balke P, Ma S, McCall N. Provider experiences with chronic care management (CCM) services and fees: a qualitative research study. J Gen Intern Med. 2017;32(12):1294-1300. doi:10.1007/s11606-017-4134-7
5. Schurrer J, O’Malley A, Wilson C, McCall N, Jain N. Evaluation of the diffusion and impact of the Chronic Care Management (CCM) services: final report. Mathematica Policy Research Report. November 2, 2017. Accessed March 29, 2023. http://bit.ly/2AlFovc.
6. Sengupta R, Honey K. AACR Cancer Disparities Progress Report 2020: achieving the bold vision of health equity for racial and ethnic minorities and other underserved populations. Cancer Epidemiol Biomarkers Prev. 2020;29(10):1843. doi:10.1158/1055-9965.EPI-20-0269