- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Panel Addresses How Payers, Providers Can Optimally Use Real-World Evidence to Advance Cancer Care
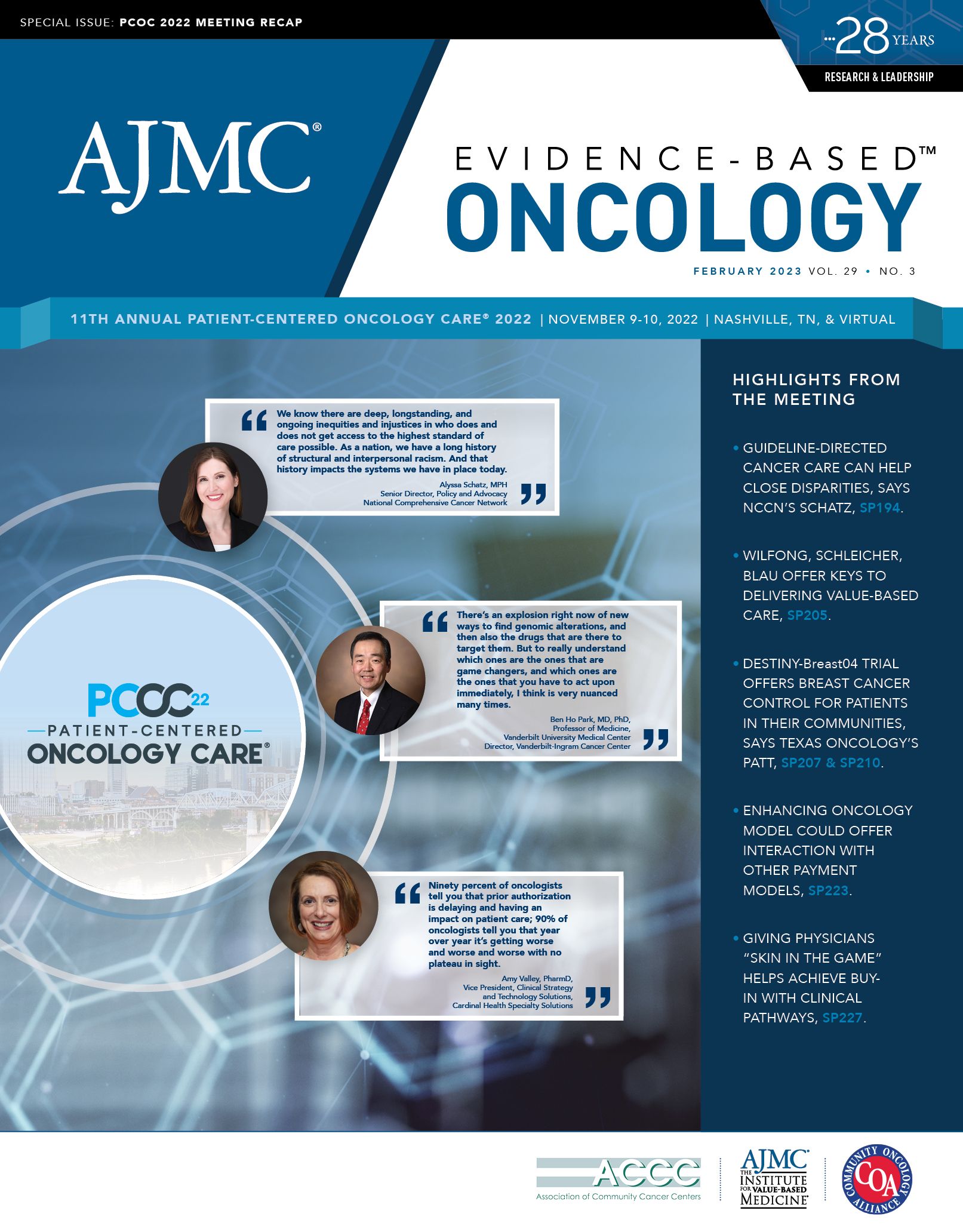
Utilizing real-world evidence that applies to the specific care needs of certain patient populations can promote timely decision-making among payers and providers on the use of effective cancer therapies available on the market, said panelists at the 2022 Patient-Centered Oncology Care® (PCOC) meeting.
Note: A previous version of this article appeared with our meeting coverage.
Novel therapeutics have demonstrated efficacy and safety in clinical oncology trials. However, issues that may impact the generalizability of trial findings, such as diversity of patient enrollment and significant cost implications, warrant more enhanced data from manufacturers. That would help payers and health systems decide which patients would benefit most from these drugs.
Real-world evidence (RWE) from these trials can address gaps in knowledge regarding the use of specialty drugs for specific patient subpopulations, noted an expert panel during the 11th Annual Patient-Centered Oncology Care® meeting in November.
Moderator Ryan Haumschild, PharmD, MS, MBA, director of pharmacy services for Winship Cancer Institute at Emory University in Atlanta, Georgia, said that not only can these data help promote timely decision-making for the use of current and emerging cancer therapies, but they can also inform payers and providers on gaps in care for patients who are not represented and what efforts may be needed to improve treatment.
The types of data involved in RWE were explained by Miruna Sasu, PhD, MBA, president and CEO of COTA Healthcare, Inc, based in New York, New York, who said that her previous experience in biotech pharmaceuticals has helped her understand the impact RWE has on the patient and on drug development and approval.
COTA’s process for aggregating data from electronic medical records to integrate into a real-world database and subsequently generate RWE involves a spectrum of very-deep-use cases on certain types of data, Sasu noted, such as figuring out a particular patient’s needs and how they might potentially react to a therapy.
“We’re predicting types of outcomes, and that requires really deep data. And [those] deep data need to come from a database that has been abstracted, cleaned, and is typically regulatory grade,” Sasu said. “Whereas there are other questions that may be a little bit later in nature. How many patients has this particular health care provider seen who have these characteristics? How much was the payment for a particular medicine? Those are sort of in varying depths of data, and you can use claims data for things like that.”
As Sasu mentioned, addressing specific research questions requires data that apply to each specific task. And as such, real-world data and RWE do not comprise a one-size-fits-all approach.
Emphasizing the key theme of “fit for purpose,” Sonia T. Oskouei, PharmD, BCMAS, DPLA, previously with Cardinal Health, said that discussions about real-world data depend on what is being studied. “You might not need the most robust, well-rounded data set to have a strong RWE study. You need a strong analysis. So you could have strong real-world data and poor RWE associated with it if you don’t have strong analysis. You can’t have strong RWE without strong fit-for-purpose, real-world data,” said Oskouei, now vice president for biosimilars and specialty at Sandoz.
Afsaneh Barzi, MD, PhD, vice president of value and quality for AccessHope, a subsidiary of City of Hope, in Duarte, California, added that quality real-world data can also be collected from case reports and case series beyond what is available in data sets from RWE providers (eg, Flatiron Health, Optum) and collecting it depends on how the data applies to the questions asked.
“We have to be careful what outcome we are looking at. We can’t take COTA’s data and look at response rate because there is no way that it’s accurately reflected in the way we measure it in clinical trials,” Barzi said. “But we can see traces of that. We can look at different things—the data have been used as long as there has been medical literature. We just gave [real-world data] a fancy name, but we have to be careful how we use it, what we expect out of it, and what we are looking for. The source would definitely be different depending on the question.”
The patient perspective and the patient voice are not extensively reflected in RWE, said Bobby Green, MD, MSCE, president and chief medical officer at Nashville, Tennessee-based Thyme Care.
In driving essential outcomes within oncology, such as overall survival and quality of life, he said improvements are necessary to better integrate these metrics, as well as data related to death that will be required by the Enhancing Oncology Model (EOM) (eg, chemotherapy given within days of death).
“The thing that universally impacts the efficacy of a drug is whether the patient actually takes the drug. And financial toxicity often gets overlooked, at least from the patient’s perspective. So making sure and understanding when drugs are going to be affordable or not for patients impacts [adherence]—drugs don’t work if you don’t take them,” Green said.
The panelists highlighted the benefits that RWE provides in working with payers on pathway development and adding or removing medications from formulary.
Biosimilars have particularly benefited from RWE, Oskouei said, as clinical research has helped to drive utilization and early adoption in oncology. Moreover, it has demonstrated applicability in regulatory decision-making for biosimilars coming to market.
Regarding pathway development, Barzi described how olaparib (Lynparza) and pembrolizumab (Keytruda) have shown clinical efficacy in pancreatic cancer for patients with germline BRCA1 or BRCA2 mutations. However, because less than 40% of patients undergo germline testing, including those who are covered for testing (eg, those with private, employer-based insurance), insights on who would benefit from these drugs were lacking.
The National Comprehensive Cancer Network subsequently issued guidelines recommending the use of germline testing for every patient with pancreatic cancer after the positive findings shown previously with these drugs. But there remains an unmet need to make care comprehensive and complete for these patients, Barzi said.
Because questions are often asked by payers about why they should cover certain drugs or care services that may not be aligned with sponsor requests, having these data can assist providers during these discussions, Sasu noted, and even spark ideas for potential clinical trials that can ultimately translate RWE outcomes for a value-based environment.
Oskouei added that this will be particularly useful amid the rollout of the Inflation Reduction Act (HR 5376) because it will increase demand for a strong clinical package associated with emerging therapeutics that will likely become Medicare-negotiated products.
“Taking these [oncology] databases and performing these questions on a regular basis as your drug gets to market is a really important aspect of being able to measure [toxicities and treatment duration]. But measuring exactly what is required can be really challenging to do from electronic medical records and curating doctor’s notes. If we could capture them at the point of care, and really be able to get to the questions that we need to answer from there, I think that would be really meaningful,“ said Oskouei.
“Thinking about how to collect that data appropriately and in an async manner from the patient is also, I think, going to be critically important,” Green added. “And then I think the biggest barrier in the EOM space has been around the health equity assessments and collecting and reporting that data. It’s something that we’ve spent a lot of time thinking about: How do we make the tools and the workflows for that to actually happen? But I think that’s going to be one of the biggest operational things that we’re going to see in the EOM.”
Specialty and Operator Status Influence Electronic Health Record Use Variation
January 22nd 2026Operators demonstrated specialty-specific differences in electronic health record efficiency, timeliness, and after-hours use, highlighting how workflow and training shape documentation behaviors across medical disciplines.
Read More
