- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
PA Is Part of an “Antiquated System” With Patient Safety, Workforce Burnout Implications
As the number of oncology drugs given as oral therapies increases, so too have challenges with prior authorization (PA) and utilization management from pharmacy benefit managers (PBMs), said Kashyap Patel, MD, associate editor of Evidence-Based Oncology™ and CEO of Carolina Blood and Cancer Care Associates, who moderated a panel discussion around these strategies at the 11th Annual Patient-Centered Oncology Care® meeting.
Although PBMs may have had good intentions when they were created to save money for the benefit of patients, they have morphed into something else, said Jeffrey Patton, MD, CEO of OneOncology and executive chairman of the board for Tennessee Oncology, in Nashville.
Amy Valley, PharmD, vice president of clinical strategy and technology solutions at Cardinal Health Specialty Solutions, echoed the sentiment. She added that significant research has come from multiple sources, including the American Society of Clinical Oncology and the American Medical Association, documenting the burden on providers and the delays in care as a result of PBMs and their tactics.
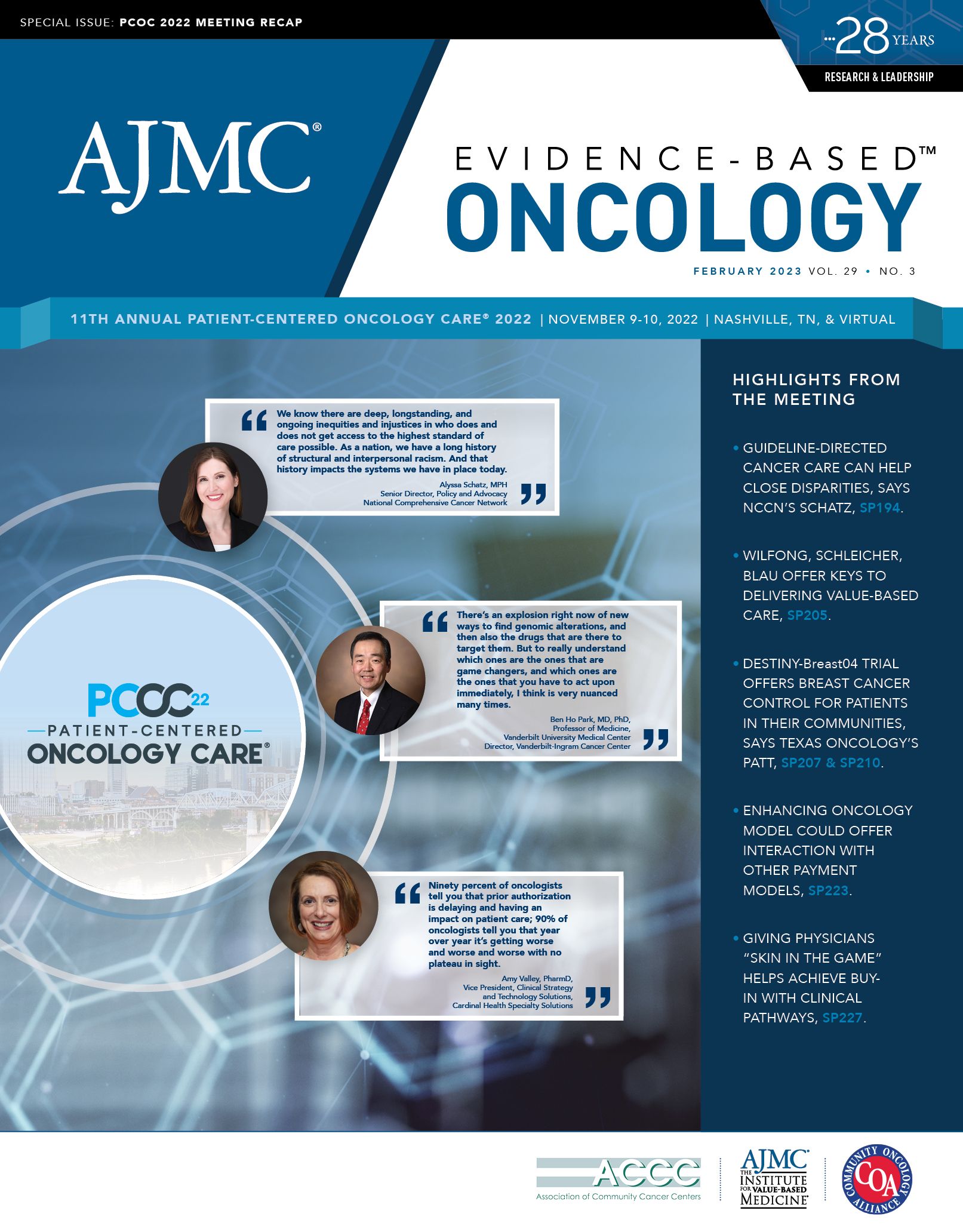
Valley referenced findings from a Cardinal Health report that showed that nearly 90% of oncologists said PA is a barrier to starting new patients on medication.1 “Ninety percent of oncologists tell you that [PA] is delaying and having an impact on patient care,” she said. “90% of oncologists tell you that year over year it’s getting worse and worse and worse with no plateau in sight.”
However, despite the use of PA, 90% of the time the therapies prescribed ultimately get approved, she said.
For Ryan Haumschild, PharmD, MS, MBA, director of pharmacy services at Winship Cancer Institute of Emory University, PA is part of an antiquated system that was initially set up to provide some utilization management before the era of consensus around guidelines and evidence-based care that exists today. However, the PA system persists, possibly more out of comfort than a real need.
“I do think having the right indication and driving the right therapeutic selection is always a great thing, but I’m not sure that prior authorizations are doing that anymore,” Haumschild said. “How do we start reform around it?”
There was a perception at one time that oncologists were not following guidelines, but that is not really the case anymore, noted Lalan Wilfong, MD, vice president of payer relations and practice transformation at The US Oncology Network (The Network). The intent when tactics like PA were implemented was to gain control over oncologists and other physicians who were just prescribing all the drugs.
There has been a change, though. Today, more than 95% of the time, oncologists in The Network are following national guidelines and managing patients appropriately, he noted.
PA, Wilfong said, “has changed into a utilization management technique not around what’s best for the patient but what’s best for the PBM.”
The Network has value-based payment contracts in place with payers where its practices and clinicians are being assessed for total cost of care, and they are incentivized to use the most cost-effective therapies for patients.
However, now Wilfong is sitting in meetings with payers who want to use more expensive therapies than The Network wants to use because there are rebates, which shows the incentives are misaligned.
Another example of where profits are misaligned, pointed out Patel, is when more expensive reference products are used because less expensive generics or biosimilars are denied by the insurance company.
“You don’t have that many levers to lower cost of care in oncology,” but choosing less expensive generics or biosimilars is one area, Valley said. However, sometimes oncologists are unable to take advantage of this because the reference product is the preferred drug on the formulary and they have to use it. Those patients don’t end up realizing the benefit of the lower cost of care.
These misaligned incentives have serious consequences for patients, noted Haumschild, because they result in delays in care, and some patients need to get treatment as quickly as possible. “The thing that worries me a lot is when you have delay, you have [disease] progression,” he said. “That’s absolutely a patient safety issue.”
The challenges around PA and utilization management are also a health equity issue, Patel noted. These require patients to navigate a system they might not understand and if they are unable to do so, their care will be on the line or more expensive.
Although the providers do a lot of work, a lot of burden remains on patients to get through the system, Wilfong said. “How will patients who don’t have equitable access to care [be] able to navigate the system to get the drugs they need? They [w]on’t. It increases our inequities significantly.”
The panelists also discussed the additional workforce burdens that PAs create. Haumschild pointed out that staff in the clinic is being pulled away from clinical activities to run through PAs, creating patient safety issues. Patel added that when practices are already understaffed, as they have been since the pandemic, making nurses and doctors spend time on hold with the insurance company instead of providing care puts an extra burden on the remaining staff. “Are we going to be able to keep our staff engaged and motivated to do what they want to do, which is take care of patients?” he asked.
Although the burden of PA and utilization management cannot be eliminated, there are opportunities for technological assistance, Valley said. On the pharmacy benefit side, there is a standard transaction for PAs and benefits verification, but the same is not true for the medical benefit for Medicare Part B. Without that standardization, there is no opportunity for electronic PA; faxing is used instead, which typically takes 5 days to 2 weeks but can take even longer.
However, on the pharmacy side, it can take a matter of hours because of standardization, she explained.
“…Companies can build technology to that standard that tries to deliver the efficiency and so we can get the work done with fewer people and eliminate some of this administrative burden,” Valley said.
States can help make changes, Wilfong said. Through the efforts of the Texas Medical Association and Debra Patt, MD, PhD, MBA, executive vice president of Texas Oncology, the state of Texas passed a “gold card bill” where physicians who adhere to guidelines more than 90% of the time over a 6-month period are “gold carded” and exempt from PA requirements for those services.2 Payers are now mandated to comply when physicians are doing well. Tennessee is also working on gold card legislation.
In Louisiana, Kathy W. Oubre, MS, CEO of Pontchartrain Cancer Center, helped push through legislation to prevent white bagging and ensure that health insurers pay for physician-administered drugs and related services.3 And in Pennsylvania, a new bill ensures timely approvals, timely appeals, and a peer review by a physician in the specialty.4
“I think there is a significant opportunity there to work with our states and get states to start passing legislation to fix the problem,” Wilfong said.
References
1. Oncology Insights: December 2022. Cardinal Health. Accessed January 23, 2023. https://www.cardinalhealth.com/en/services/specialty-physician-practice/resources/whitepapers-and-downloads/oncology-insights.html
2. Robeznieks A. New physician “gold card” law will cut prior authorization delays. American Medical Association. September 15, 2021. Accessed January 23, 2023. http://bit.ly/3YbmRdF
3. Devino M. New Louisiana law bans white bagging. ACCCBuzz blog. June 17, 2021. Accessed January 23, 2023. http://bit.ly/3Xz7s6V
4. Cass A. Pennsylvania prior authorization reform bill signed into law. Becker’s Payer. November 7, 2022. Accessed January 23, 2023. https://www.beckerspayer.com/payer/pennsylvania-prior-authorization-reform-bill-signed-into-law.html