- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
David Jackman, MD, on Clinical Pathway Buy-in, Process for Updates
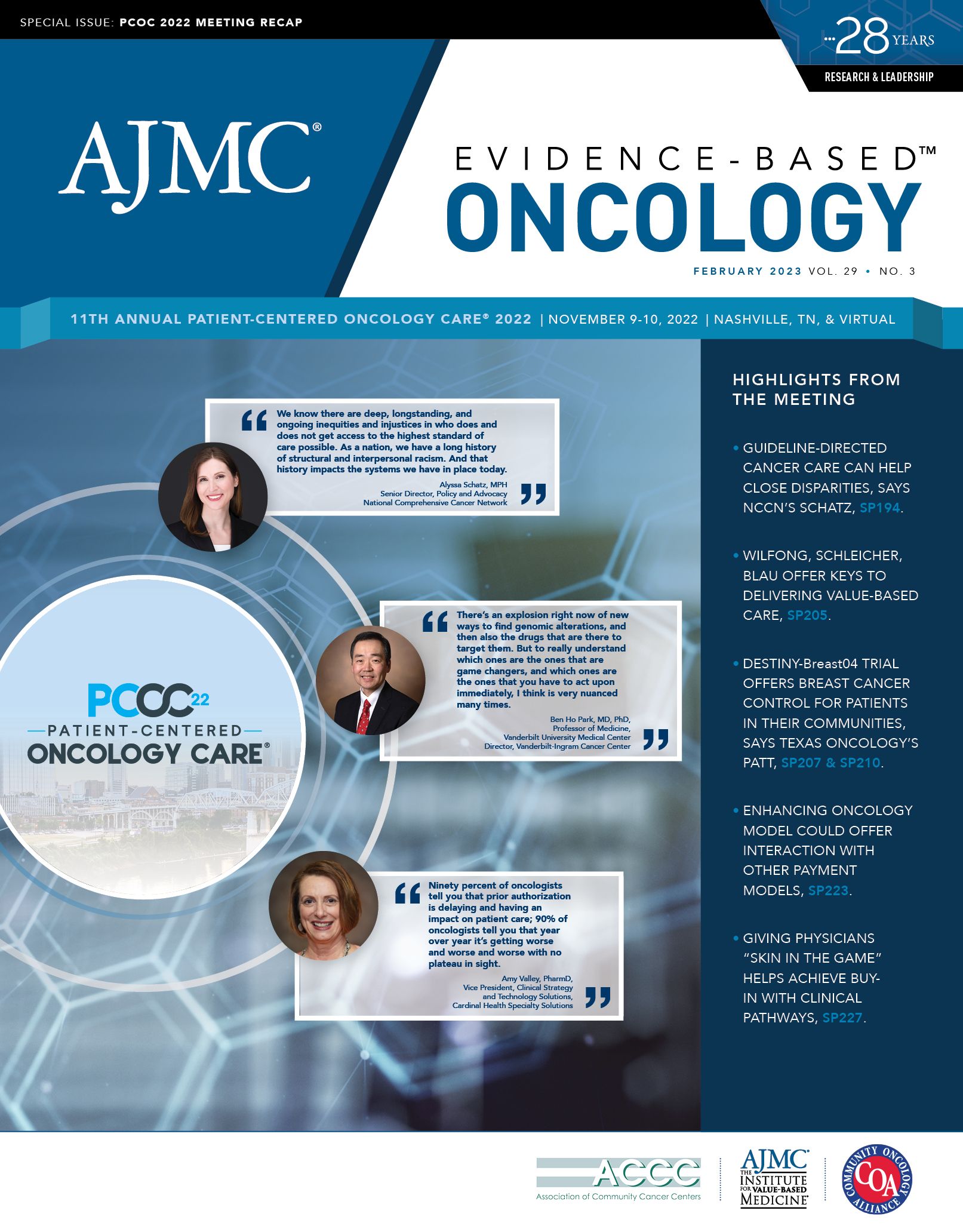
Efficiency, collaboration, and efficacy are key drivers in creating clinical pathway buy-in, with updates also vital to incorporate the latest trends and insights in cancer care, said David Jackman, MD, senior physician and medical director of clinical pathways at Dana-Farber Cancer Institute, Boston, Massachusetts. Jackman spoke with Evidence-Based Oncology™ (EBO) in Nashville, Tennessee, where he took part in a panel discussion on clinical pathways during the 11th Annual Patient-Centered Oncology Care® meeting.
EBO: What are the best strategies for institutions to create clinical pathway buy-in?
Jackman: To create buy-in, I think that it’s never just 1 thing. In terms of thinking about employing any [information technology] tool, one has to consider the spectrum of why people are hesitant. Is it technology, in which case you’ve got to refine the platform where and when you can to make it intuitive and to make it efficient? Is it concerns about content? [Physicians may say], “Dave, this isn’t how we practice,” or, “I’m a world expert. I don’t need a tool to help me do this.”
For us, part of that is bringing those [individuals] into the fold of the conversation of creating that content, so they see not only how it’s done, but also feel like they have a voice in it. And that certainly helps….
Then, in general, taking the data that you get back and showing how much we can learn from this. How have we improved our clinical trial accrual? How have we captured data with context that we can’t get from the [electronic medical record] and then enable it to give that back to departments and to researchers to say, “Wow, here’s what you can do with this.”
I think it’s all 3 of those pieces: making it more efficient, giving people a voice in the content, and making them feel comfortable that it’s expert, and showing the value from the data that one can generate that helps to create buy-in.
EBO: Can you describe the ongoing process for pathway updates?
Jackman: So, our pathway updates are always looking to have a few important qualities. How can it be expert and robust? How can it be transparent, not just about who’s in the room, but what data is being reviewed? And can there be uniformity to the process?
Our updates [involve] our experts from Dana-Farber as well as those from all participating institutions in our pathways—because ours is a platform that is available to outside institutions as well—to make sure that they feel like they have a voice. Before the meeting, we have a prereview where we create a very robust slide set of not just what the agenda items are, but what the data are that we want to discuss. What were the presented or published studies? What are the drug costs involved? What are the side effects? And [we] make sure we always address all 3 of these for every agenda item so that people are reacting to actual data and not just recall, which could be fuzzy or foggy.
Then after that [we] make sure not only that we convey this all into the platform in the way that it should be, but add to that [a] level of transparency [so] that all participants, as well as anybody using the system, has access to not just to the minutes of what happened, but to the actual recordings if they want to go back and listen. Maybe they missed that meeting; they’d love to hear what it is that people said that drove this decision.