- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Neil Iyengar, MD, Emphasizes Importance of Population Health Lens in Oncology
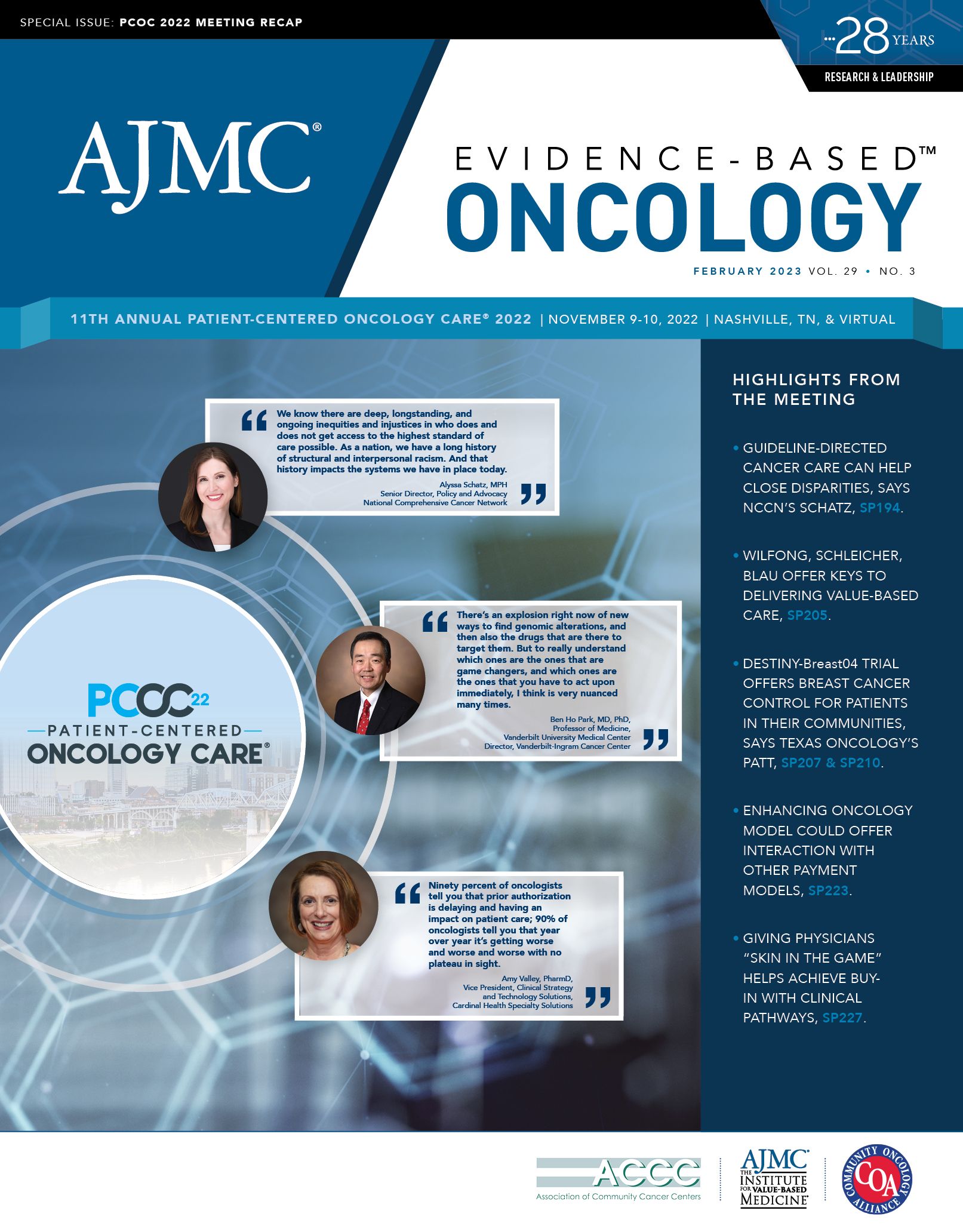
In an interview with Evidence-Based Oncology™ (EBO), Neil Iyengar, MD, associate attending physician, breast medical service, Memorial Sloan Kettering Cancer Center, New York, New York, discussed how population health brings an important lens to both oncology practice and research. Iyengar took part in a panel discussion on the topic at the 11th Annual Patient-Centered Oncology Care® meeting, held November 9-10, 2022, in Nashville, Tennessee.
EBO: Can you elaborate on what it means to bring a population health lens to cancer care?
Iyengar: As an oncologist, when I think about population health,
I think it brings an important lens to how I practice oncology but also the type of research that we do. As an oncologist, we’re very much focused on tumor-directed therapy, so oftentimes [that means] matching very specific treatments to specific lesions, say genetic lesions within the tumor. But it is helpful to zoom out and think about how host metabolism and other biological processes, as well as lifestyle and environment, may also influence both cancer risk and response to cancer treatment.
Because there are so many variables in those sorts of aspects of cancer care, population health is very helpful because we can focus on large populations and pull out observations that we may not get from anecdotal, individual experiences. So, when I say that population health helps inform both my practice and the research from a practice lens, population health can be helpful for implementing cancer care models. And from a research lens, population health can be very helpful for asking or understanding what are the right questions to ask. A lot of the questions with regard to lifestyle modification and cancer risk and outcomes were derived from observations of large study cohorts, and we wouldn’t have a lot of the lifestyle modification interventions that we have nowadays without the initial observations that were derived from population scientists.
EBO: What obesity-related cancers are on the rise, and which populations are most at risk?
Iyengar: There are at least 13 cancers that are related to obesity, and I think that this list is growing as we understand and study more cancers that may be linked to metabolic health. Currently, we define obesity by body mass index [BMI], which is derived from population studies where we use BMI as a tool to understand the general metabolic health of large populations. This is, of course, the weight in kilograms, normalized by the height in meters squared, and this has identified, as I said, at least 13 cancers that are associated with obesity.
We also know that 1 out of 6 male cancer-related deaths and 1 out of 7 female cancer-related deaths are related to obesity, so this is a major public health problem. Another issue is that the rates of obesity are on the rise in younger populations, and the American Cancer Society put out a report a few years ago showing that the incidence of cancer in younger cohorts, and specifically obesity-related cancers, is on the rise.1 So, we anticipate that the burden of obesity-related cancers worldwide is likely to increase in the coming years.
On top of that, we and others are identifying that BMI is not the best tool on the individual level to identify cancers that are related to metabolic health. For example, we’ve published a report showing that, in women with a normal body mass index, if the body fat levels are above 33%, this is associated with a doubling or more of the risk of developing invasive breast cancer. This is alarming to me because, normally, we think about people who have a healthy body mass index as not being at risk for obesity-related diseases, including obesity-related cancers.
There’s now a growing literature demonstrating that metabolic obesity in normal weight individuals is linked to multiple cardiometabolic disorders, as well as a growing list of cancers. This is a major issue, and our interventions need to be matched to identify those individuals [who] are at risk either because of their body mass index or their underlying metabolic health. And the subsequent intervention—be it a lifestyle modification— should also match, whether it is weight loss or body recomposition, by increasing muscle mass and decreasing fat mass. These are the kinds of things that we’re currently studying in clinical trials.
Reference
Sung H, Siegel RL, Rosenberg PS, Jemal A. Emerging cancer trends among young adults in the USA: analysis of a population-based cancer registry. Lancet Public Health. 2019;4(3):e137-e147. doi:10.1016/S2468-2667(18)30267-6
Quality of Life: The Pending Outcome in Idiopathic Pulmonary Fibrosis
February 6th 2026Because evidence gaps in idiopathic pulmonary fibrosis research hinder demonstration of antifibrotic therapies’ impact on patient quality of life (QOL), integrating validated health-related QOL measures into trials is urgently needed.
Read More
