- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Making Sense of Advanced Payment Models
The American Society of Clinical Oncology has developed the Patient-Centered Oncology Payment (PCOP) model with the hope that PCOP will be accepted by CMS as an advanced alternative payment model, and become available to medical oncologists as an alternative to the Merit-based Incentive Payment System.
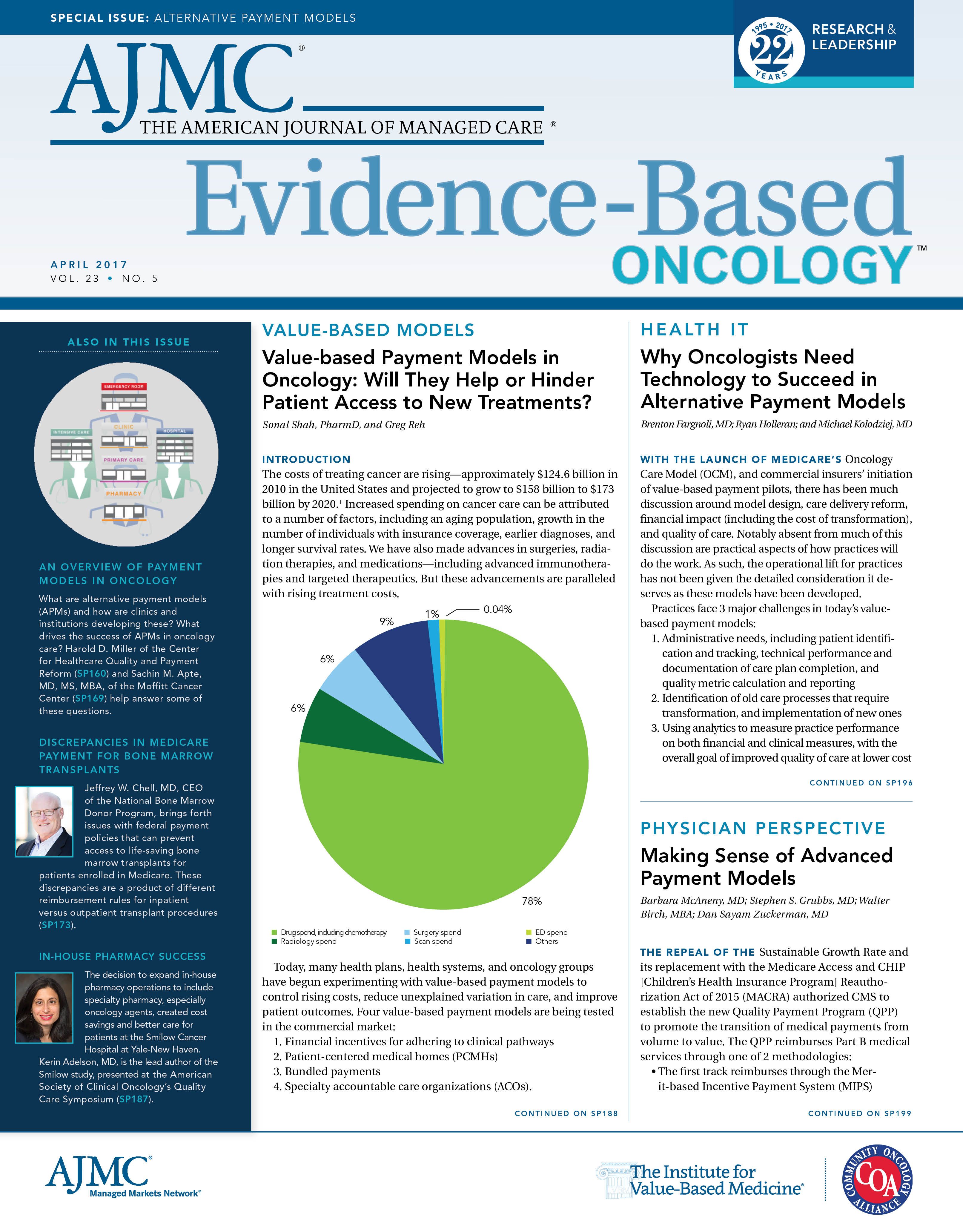
The repeal of the Sustainable Growth Rate and its replacement with the Medicare Access and CHIP [Children’s Health Insurance Program] Reauthorization Act of 2015 (MACRA) authorized CMS to establish the new Quality Payment Program (QPP) to promote the transition of medical payments from volume to value. The QPP reimburses Part B medical services through one of 2 methodologies:
- The first track reimburses through the Merit-based Incentive Payment System (MIPS)
- The second track promotes payment through advanced Alternative Payment Models (APMs).1
Under MIPS, which consolidates 3 separate programs, physicians report on:
- Quality (formerly the Physician Quality Reporting System or PQRS)
- Cost/resource use (formerly the Value-Based Modifier program)
- Advancing care information (formerly Meaningful Use)
- Improvement activities
Physician and practice performance in 2017 will be analyzed in 2018, and adjustments to the physicians’ fee schedules will be released in 2019. Physicians may report individually or as an entire practice, and scores will be based upon reported activities and ranked against all others who report under MIPS. Physicians or practices that rank ahead of their peers will be eligible for a fee schedule increase of up to 4% in 2019, and those ranked behind their peers face a decrease in their fee schedule of up to 4% in 2019. The potential fee schedule gain or loss will witness an annual increase to 9% in 2022.2
The good news is that CMS has deemed 2017 as a preparation and transition year (termed “Pick Your Pace”); a physician can avoid the 4% reduction from MIPS in 2019 by reporting 1 measure for only 1 patient for the entire year.
Advanced Alternative Payment Models
The QPP encourages physicians and practices to participate in APMs, including those designated by CMS as “advanced APMs,” characterized by the Office of the National Coordinator for Health Information Technology—-certified electronic health record (EHR) use, quality reporting, and financial standards that require 2-sided financial risk. Participation in an advanced APM that provides care for a threshold quantity of patients exempts physicians and practices from the MIPS program and provides an annual 5% reimbursement bonus starting in 2019.
The Center for Medicare & Medicaid Innovation (CMMI)’s Oncology Care Model (OCM) qualifies as an advanced APM if a practice elects the 2-sided financial risk option. This advanced APM option is limited to the nearly 200 oncology practices that were accepted into the OCM program and, subsequently, chose to participate.
Because the MACRA legislation specifies that CMS should review physician-sponsored APM models for Medicare reimbursement, Medicare has established the Physician-Focused Payment Model Technical Advisory Committee (PTAC). PTAC will evaluate the proposed models based upon their attributes of value-based care and reimbursement that will qualify as an advanced APM. One such APM is the Patient-Centered Oncology Payment Model (PCOP) developed by the American Society of Clinical Oncology (ASCO).
Patient-Centered Oncology Payment Model
Several years before MACRA, ASCO volunteers foresaw the need for a payment model that compensated oncologists for providing oncology care in a high-quality, patient-centered fashion, rather than in the current volume-based manner. The concept includes reimbursing oncology professionals for performing high-value care improving activities that had not been compensated previously.
ASCO mobilized a task force of oncologists, staff, and consultants to develop the model. The volunteer oncologists were geographically diverse and represented a variety of practice settings, including independent practice, academic institutions, and health system employed practice. This task force identified services that promote lower costs and higher quality care performed during an episode of chemotherapy or immunotherapy that are currently uncompensated or undercompensated, including:
- Detailed treatment planning
- Patient education
- Case management
Analyses of the cost of a course of chemotherapy/immunotherapy were performed to identify costs that could be eliminated or reduced. The task force then developed a payment mechanism for oncology care providers that would allow them to pay for the practice transformation needed to provide the enhanced valued care.
These efforts led to the creation of the PCOP model, published in May 2015.3 The model encompasses a chemotherapy or immunotherapy episode of care with 3 levels of reimbursement, leading from basic fee-for-service care to monthly payments to overall care bundles.
Level 1 is based on the concept of adding 3 additional reimbursement codes to cover the enhanced practice services:
- An upfront new patient treatment planning code applied at the start of a new episode of chemotherapy
- A monthly case management code during the course of chemotherapy
- A monthly posttherapy case management code for up to 6 months of monitoring following chemotherapy
A proposed fourth code would support clinical trial management. These codes augment the current evaluation and management codes, and this additional compensation will allow the physician to plan the full course of therapy, educate the patient and family, and fund practice services to efficiently manage treatment and post-treatment complications and toxicities. Examples of enhanced services include staff nurse triage lines, standardized triage protocols, extended office hours, and practitioner and infusion center capacity for same-day service to avoid emergency department (ED) and hospital admission. The model also requires adherence to care quality measures and appropriate care and resource use such as ASCO’s Choosing Wisely measures.4
The PCOP model achieves 2-sided financial risk by adjusting reimbursement to quality and performance targets. ASCO financial modeling has demonstrated both an increase in practice revenue and an overall cost saving to payers while enhancing care quality. Modeling of a typical episode of chemotherapy on a Medicare fee schedule increases Part B non-drug revenue to the practice by nearly 50% (4.3% of total cost) while simultaneously decreasing the overall cost of care by 4%.
Levels 2 and 3 of PCOP are for the more advanced practices that have shown they can successfully manage the cost of care for their patients. In level 2, monthly payments are made in lieu of all physician billings, including the 3 new codes described above and the optional clinical trials management code. Payments would have to be negotiated by disease state and risk adjusted. Finally, in level 3, bundled payments would be paid for the entire course of therapy, but they would have to be negotiated by disease state and risk adjusted. Bundling of payments that include chemotherapy and other drugs are complex and would have to be continually updated to account for new therapies.
PCOP is designed to benefit patients and their families with accurate diagnosis and appropriate treatment, education and support services, less ED and hospital care, and financial benefit by reduction of expensive ED and hospital care and unnecessary drugs and tests. Oncology practices will benefit from increased revenue from the new codes, which will reimburse the practice for current nonbillable or undercompensated services that promote effective care management and fund practice transformation—this will allow all members of the oncology care team to perform at the highest level of their license and skill set. Payers will benefit from not just lower costs, but enhanced quality of care and member satisfaction.5
Oncology Medical Home Model Shows Promise
Physician practices that move from “volume-based” to “value-based” payment models require adjustments of their practice to be successful. Published evidence suggests that physician practice transformation to an oncology patient-centered medical home model will achieve the goals of better care and cost required by an APM.1 A CMMI grant—funded COME HOME project, which incorporated oncology medical home systems within 7 oncology practices and measured oncology practice outcomes, demonstrated high quality care at reduced costs and high patient satisfaction. Over the 3-year period, ED use at the 7 practices decreased by 11.7%, hospital admissions declined by 6.6%, and hospital readmissions reduced by 12.5%. These cost-saving results were achieved with a high patient satisfaction of 98.1%.6 The tools that were developed and the knowledge that was acquired from this project reside in Innovative Oncology Business Solutions (IOBS).
ASCO has licensed the IOBS tools to assist practices in the transformation required to be successful in this new era of practice. This initiative, named the ASCO COME HOME program, will assist practices in implementing the programs necessary to acquire and develop medical oncology home characteristics that will promote success in APMs.
The PCOP model, which can be adapted by commercial payers and by Medicare, is currently operational with an independent oncology practice and a regional commercial insurer. Several other practices and commercial insurers are evaluating the model for implementation. The PCOP model is also being revised to be presented to the PTAC and then CMS for designation as an advanced APM. The following revisions are planned:
- Quality metrics to ensure cost savings while delivering appropriate care, and an efficient reporting of quality metrics that will not be an onerous requirement on physicians.
- Incorporating nationally accepted pathways into the model to ensure that patients receive evidence-based treatment.
- A 2-sided financial risk model that rewards outstanding care and penalizes less than optimal care, with a level of downside risk that will not lead to the insolvency of physician practices.
- EHR utilization and reporting.
- Oncology medical home infrastructure requirements.
ASCO is hopeful that PCOP will be accepted by CMS as an advanced APM and become available to medical oncologists as an alternative to the MIPS program.
Conclusion
FUNDING SOURCE:
None.
AUTHOR INFORMATION
Barbara McAneny, MD, is chief executive officer and chief medical officer, Innovative Oncology Business Solutions.
Stephen S. Grubbs, MD, is vice president, Clinical Affairs Department, American Society of Clinical Oncology.
Walter Birch, MBA, is division director, Practice Management, Resources, Performance Improvement, and Quality Certification Division, American Society of Clinical Oncology.
Dan Sayam Zuckerman, MD, is medical director, St. Luke’s Mountain States Tumor Institute, and immediate past chair of the American Society of Clinical Oncology’s Clinical Practice Committee.
ADDRESS FOR CORRESPONDENCE
Stephen S. Grubbs, MD
2318 Mill Road, Suite 800
Alexandria, VA 22314
E-mail: Stephen.Grubbs@asco.org.
Value-based healthcare is an evolving practice reality accelerated by the QPP, And APMs seem the likely predominant payment model of the future in this new system. ASCO’s PCOP model will offer oncology practices an APM that will provide improved patient care and satisfaction, reward physicians for providing excellent care, and reduce costs for patients and payers. The ASCO COME HOME program will assist oncologists and practices in this transformation of care, and with PCOP, will attempt to achieve the healthcare Quadruple Aim (enhanced patient experience, improved population health, cost reduction, and improved provider work life).REFERENCES
1. Physician payment reform. American Society of Clinical Oncology website. www.asco.org/paymentreform. Accessed February 24, 2017.
2. Payment for Part B Medical and other health services, 42 C.F.R. pt. 4 (2016). Government Publishing Office website. https://www.gpo.gov/fdsys/pkg/FR-2016-11-04/pdf/2016-25240.pdf#page=541. Published November 4, 2016. Accessed February 23, 2017.
3. Ward et al. (May 2015). Payment Reform to Support Higher Quality, More Affordable Cancer Care. Patient-Centered Oncology Payment. http://www.asco.org/sites/new-www.asco.org/files/ content-files/advocacy-and-policy/documents/asco-patient-centered-oncology-payment.pdf. Accessed 23, Feb 2017.
4. Five things physicians and patients should question. Choosing Wisely website. http://www. choosingwisely.org/wp-content/uploads/2015/02/ASCO-Choosing-Wisely-List.pdf. Updated October 29, 2013. Accessed 23, Feb 2017.
5. Sprandio JD, Flounders BP, Lowry M, Tofani S. Data-driven transformation to an oncology patient-medical home. J Oncol Pract. 2013;9(3):130-132. doi: 10.1200/JOP.2013.001019.
6. Personal correspondence.
NAACOS Continues Pushing Forward on the Transition to Value-Based Care
September 21st 2020Allison Brennan, MPP, discusses legislation that would affect accountable care organizations (ACOs), the impact coronavirus disease 2019 had on ACOs, and the fall National Association of ACOs meeting.
Listen
Ambient AI Tool Adoption in US Hospitals and Associated Factors
January 27th 2026Nearly two-thirds of hospitals using Epic have adopted ambient artificial intelligence (AI), with higher uptake among larger, not-for-profit hospitals and those with higher workload and stronger financial performance.
Read More
Examining Physician-Initiated Alternative Payment Models, a New Wave of Payment Reform
September 12th 2019To date, most alternative payment models (APMs) that have emerged in the shift toward value-based care have been initiated by payers and focused on primary care providers. However, there has recently been a new wave of payment reform in which providers, mostly specialists, are designing and implementing their own APMs in their practices. A study published in the September issue of The American Journal of Managed Care® analyzed some of these new payment models to gain insight into what providers are prioritizing in their APMs.
Listen
Specialty and Operator Status Influence Electronic Health Record Use Variation
January 22nd 2026Operators demonstrated specialty-specific differences in electronic health record efficiency, timeliness, and after-hours use, highlighting how workflow and training shape documentation behaviors across medical disciplines.
Read More

