- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
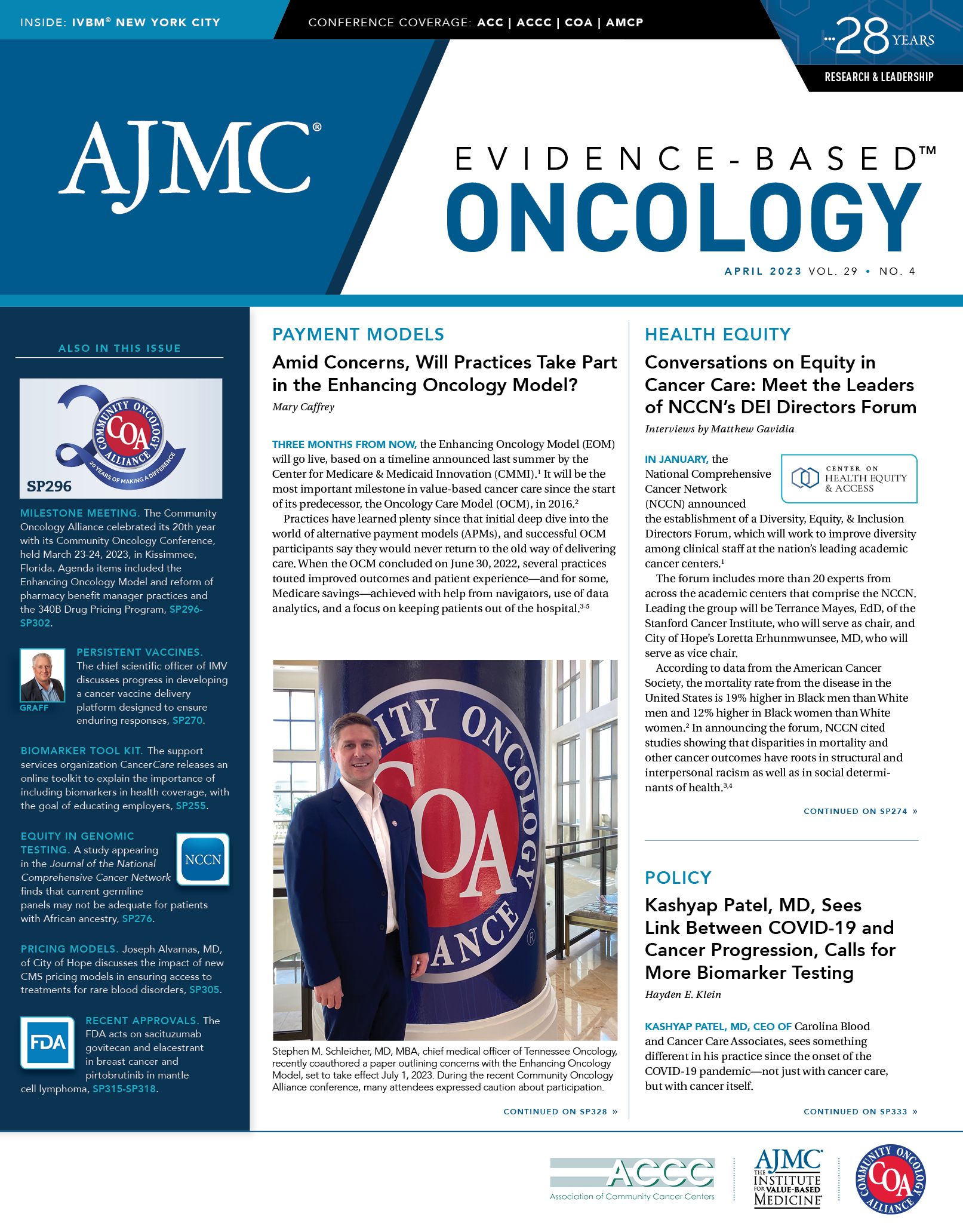
Kashyap Patel, MD, Sees Link Between COVID-19 and Cancer Progression, Calls for More Biomarker Testing
Recent papers highlight possible role of inflammation in connections between COVID-19, cancer markers.
Kashyap Patel, MD, CEO of Carolina Blood and Cancer Care Associates, sees something different in his practice since the onset of the COVID-19 pandemic—not just with cancer care, but with cancer itself.
Since March 2020, the longtime community oncologist has seen multiple patients in his Rock Hill, South Carolina, based-clinic with cholangiocarcinoma, and these patients are developing the rare cancer 20 to 30 years earlier than the typical age at presentation, which is usually 65 years or older.1 In the past year alone, physicians in Patel’s practice saw 7 patients with this cancer, and 3 have died.
It is not just a single cancer type, either. Patel and his colleagues, both in the United States and those he knows overseas, have seen patients with rapidly progressing cancers of several types, such as breast cancer and renal cell carcinoma. During an interview with Evidence-Based Oncology™(EBO), Patel said several did not even have time to receive treatment and died within weeks of diagnosis.
Among these was a patient aged 26 years with rapidly progressing triple-negative breast cancer. Another patient developed systemic inflammatory response syndrome, which can be caused by an infection, inflammation, or pancreatitis, and is often seen in patients with lung cancer.2 The patient was 51 when he died 4 weeks after receiving a diagnosis, making him 15 years younger than the typical patient with this condition.3
Patel said one his colleagues told him that he cannot keep up with the volume of new patients presenting with prostate cancer at his practice in India.
“The trend is getting more and more alarming,” Patel emphasized. “We are noticing trends in hematological malignancies, breast cancer, colorectal carcinoma, and pancreatic cancer.”
Several cancer types Patel cites were causing alarm among oncologists even before the pandemic. In 2019, the American Cancer Society (ACS) published an epidemiological study in The Lancet Public Health based on data collected among adults aged 25 to 49 years from 1995 to 2014; investigators found that despite the overall drop in cancer mortality, incidence of several obesity-related cancers were rising sharply among younger adults.4
With COVID-19 added to the mix, Patel now fears a “perfect storm” of factors will trigger inflammatory responses in some patients, causing cancer to arrive years earlier than normal and making it deadlier once it is diagnosed.
“If you go back and look at the post–COVID[-19] recovery phase—we are coming out of almost like a hibernation—a lot of people don’t know how to deal with the stress,” Patel said. “Combined with the obesity pandemic, people didn’t exercise a lot with the fear of going out in the pandemic, and the alcohol intake has increased. All of this descends down on inflammation, and I think it’s creating a perfect storm between [these] risk factors, and we need to learn how to deal with that.”
The most recent ACS annual report on cancer statistics, which typically offers breakdowns by cancer type, does not reflect data from years of the pandemic.5 However, a December 2022report from the Centers for Disease Control and Prevention (CDC) finds that from 2018 to 2021, the annual number of cancer deaths increased 4.7%, after a long period of declining cancer mortality.6 Although some increase in cancer deaths had been anticipated due to a drop in screening, CDC investigators found disproportionate increases in cancer deaths with COVID-19 as an underlying cause, with higher rates among males; members of ethnic or racial minority groups; and those with lymphoma, leukemia, or myeloma.
Patel is now on a mission to put concrete numbers to what he acknowledges are clinic-level observations, and to find a way to help patients most at risk. There is evidence to support Patel’s observation that SARS-CoV-2 can set off inflammatory responses in tumors, causing cancer to progress much sooner and more aggressively, and even reawaken dormant cancer cells.
The mission now is to develop the data, which will require tests, research, and funding to pay for it all.
Patel is undeterred by the challenge. He is meeting with payers, colleagues, the news media, and anyone else who will listen in hopes of launching a study among community oncologists that would lead to a prospective registry that would help physicians “understand more about who experiences post–COVID[-19] conditions and why, including whether groups disproportionately impacted by COVID-19 are at higher risk” for developing cancer or having more aggressive cancer.
Other Post–COVID-19 Trends
Post–COVID-19 conditions can include a wide range of ongoing health problems, which vary in severity and can last weeks, months, or longer, as demonstrated by long COVID symptoms. Individuals not vaccinated against COVID-19 who contract the virus may also be at increased risk of developing a post–COVID-19 condition compared with those who are vaccinated and had a breakthrough infection. Additionally, some persons experiencing post–COVID-19 conditions may not have tested positive for the virus or known they had it.
According to Patel, more research needs to be done to better understand who experiences these post–COVID-19 conditions and why, whether populations disproportionately impacted by COVID-19 are at higher risk of these conditions, and whether cancer is one of these post–COVID-19 conditions.
There is support for this idea in existing research. Saini and Aneja hypothesized that cancer should be considered another sequela of long COVID, with other COVID-19 sequelae including cardiovascular, pulmonary, and neurological conditions.7
“It is becoming increasingly evident that [patients with cancer] are more susceptible to SARS‐CoV‐2 infection and are at a higher risk of severe COVID‐19 than the general population,” the authors said. “Nevertheless, whether long COVID‐19 increases the risk of cancer in those with no prior malignancies remains unclear.”
They echoed that more research is needed but, given the disproportionate impact of COVID-19 on Black patients and the community more broadly, another unanswered question is whether racial disparities are to be expected in COVID‐19 sequelae, including cancer.
COVID-19 and Tumor Cell Inflammation
Despite the current lack of concrete, real-world data linking COVID-19 infection to cancer progression, the science supports the association in theory.
An early paper by Francescangeli et al appearing in Frontiers in Oncology in October 2020 discussed the possibility that COVID-19 could reawaken dormant cancer cells and cause a relapse, but that the precise mechanism of inflammation in cancer cells had “yet to be elucidated.” Examining how SARS-CoV-2 interacted with cancer cells and the immune system would require complex mouse models, and this research would not be easy—but that was no reason to avoid the questions, the authors wrote.8
A subsequent 2022 review in Frontiers in Molecular Biosciences by Rahimmanesh et al supports Patel’s points. It suggests a potential link between COVID-19, inflammation, and immune-mediated tumor reawakening, particularly the reawakening of dormant cancer cells and metastatic relapse.9
Referencing past research, these authors noted that immune responses in patients with COVID-19 are orchestrated by proinflammatory cytokines—IL-1, IL-6, IL-8, and tumor necrosis factor alpha (TNF-α)—which are also known to drive tumorigenesis. COVID-19 infection has also been linked to T-cell depletion and activation of oncogenic pathways—including JAK/STAT, MAPK, and NF-κB—which may potentially increase the risk of cancer development.
Several other factors related to COVID-19 infection may be related to cancer progression.
“Besides impaired T-cell response, elevated levels of cytokines, growth factors and also chemokines in the plasma of patients in the acute phase of COVID-19 as well as tissue damage and chronic low‐grade inflammation in ‘long COVID‐19’ syndrome may facilitate cancer progression and recurrence,” the authors said.
Collectively, these investigators say, if these observations are confirmed by further studies, they may have important implications for the treatment and long-term management of patients with cancer who have had COVID-19.
Inflammation and the Need for Biomarker Testing
After the pandemic began, a 2021 paper funded by the National Cancer Institute/National Institutes of Health explored the links among stress, inflammation, and cancer. It reviewed data that found inflammatory markers “specific to both cancer and depression,” as well as the mechanisms by which inflammation can affect both tumors and neurotransmitters and neurocircuits in the brain.10 The authors discussed interventions to reduce inflammation and depression in patients with cancer, pointing to the same risk elements of obesity, stress, and inflammation that Patel believes are causing the patterns he sees in his clinic.
Some studies have looked at potential biomarkers of this link between COVID-19 infection and worsening cancer progression, even if it was not a primary end point.
Research at Mount Sinai Health System in New York, New York, published in Nature Medicine, looked at whether inflammatory cytokine levels could serve as a biomarker to predict disease course and outcomes in patients hospitalized with COVID-19, with 147 participants with COVID-19 having cancer, among other comorbidities included in the study.11
After following a total of 1484 patients, researchers found that elevated IL-6 and TNF-α serum levels at COVID-19 presentation were strong predictors of disease severity and survival. However, when looking at associations with a range of comorbidities like diabetes and heart failure, they found no association between cytokine levels and active cancer. According to the researchers, these results suggest multiplex cytokine profiling could help stratify patients as well as guide resource allocation and prospective interventional studies.
Understanding the relationship between COVID-19 and cancer could inform treatment decisions. A systematic review of 16 studies published within the first year of the COVID-19 national emergency even demonstrated that chemotherapy can increase the mortality risk of COVID-19 among patients with cancer. Specifically, chemotherapy within the last 30 days before COVID-19 diagnosis increased the risk of death for these individuals after adjusting for confounding variables (OR, 1.85; 95% CI, 1.26-2.71). There were no safety concerns surrounding immunotherapy, targeted therapies, surgery, and radiotherapy (however, the authors and Zou et al exchanged letters clarifying which surgical patients were included in the study).12-14
The common denominator among these studies is the investigators’ call for additional research. Realistically, they write, it may take years to establish a clear association between COVID-19 and cancer progression, but that makes it even more important to focus on research now. It is also important to note that, even if the existing research cannot find a clear association between the two, they do support the need for biomarker testing to help understand this association.
Patel told EBO his talks with payers have centered on the need for broader biomarker testing to gain a better understanding of the relationship between prior COVID-19 and cancer and, more importantly, to better understand risk factors of future patients. In documentation provided to EBO supporting the need for a study, Patel asserts that these trends, if widespread, could have important cost implications for payers and employers.
Specifically, he is calling for a multisite prospective observational study of postacute sequelae SARS-CoV-2 infection (PASC) in patients who are diagnosed with cancer. An outline of a study protocol calls for following up to 10,000 patients over 5 years; patients would be enrolled in community oncology clinics. The primary end point would measure PASC symptoms over time and the natural course of cancer, correlation to stress, biomarkers of inflammation, family history, social determinants of health, and outcomes. (The study protocol document was provided to EBO in an email).
“One of the biggest things that we see with cancer and COVID-19 is that cancer is a chronic disease,” Patel said. “If we try to establish the link, it may take years, but what worries me is that if indeed there’s a link between COVID-19 and cancer, then the whole world had COVID-19, practically.”
That widespread nature of COVID-19 means insurers should pay for the common biomarker tests outlined by the investigators in the Nature Medicine study, he said. “We have to start covering these tests to ensure that if we’re studying the link between COVID-19, inflammation, and cancer, these tests are covered.”
Mary Caffrey contributed to this report.
References
- Key statistics. Cholangiocarcinoma Foundation. Accessed March 19, 2023. https://cholangiocarcinoma.org/key-statistics/
- Systematic inflammatory response syndrome. National Cancer Institute. Accessed March 19, 2023. https://bit.ly/3JrkDRn
- Kuo AS, Dusan H, Aldrich JM. Critical care anesthesiology. In: Gropper MA, Eriksson L, Fleisher L, Wiener-Kronish J, Cohen N, Leslie K, eds. Miller’s Anesthesia. Elsevier; 2020:2654-2670.e5.
- Sung H, Siegel RL, Rosenberg PS, Jemal A. Emerging cancer trends among young adults in the USA: analysis of a population-based cancer registry. Lancet Public Health. 2019;4(3):e137-e147. doi:10.1016/S2468-2667(18)30267-6
- Siegel RL, Miller KD, Wagle NS, Jemal A. Cancer statistics, 2023. CA Cancer J Clin. 2023;73(1):17-48. doi:10.3322/caac.21763
- Henley SJ, Dowling NF, Ahmad FB, Ellington TD, Wu M, Richardson LC. COVID-19 and other underlying causes of cancer deaths—United States, January 2018-July 2022. MMWR Morb Mortal Wkly Rep. 2022;71(50):1583-1588.
- Saini G, Aneja R. Cancer as a prospective sequela of long COVID-19. Bioessays. 2021;43(6):e2000331. doi:10.1002/bies.202000331
- Francescangeli F, De Angelis ML, Baiocchi M, Rossi R, Biffoni M, Zeuner A. COVID-19–induced modifications in the tumor microenvironment: do they affect cancer reawakening and metastatic relapse? Front Oncol. 2020;10:592891. doi:10.3389/fonc.2020.592891
- Rahimmanesh I, Shariati L, Dana N, Esmaeili Y, Vaseghi G, Haghjooy Javanmard S. Cancer occurrence as the upcoming complications of COVID-19. Front Mol Biosci. 2022;8:813175. doi:10.3389/fmolb.2021.813175
- McFarland DC, Riba M, Grassi L. Clinical implications of cancer related inflammation and depression: a critical review. Clin Pract Epidemiol Ment Health. 2021;17(1):287-294. doi:10.2174/1745017902117010287
- Del Valle DM, Kim-Schulze S, Huang HH, et al. An inflammatory cytokine signature predicts COVID-19 severity and survival. Nat Med. 2020;26(10):1636-1643. doi:10.1038/s41591-020-1051-9
- Yekedüz E, Utkan G, Ürün Y. A systematic review and meta-analysis: the effect of active cancer treatment on severity of COVID-19. Eur J Cancer. 2020;141:92-104. doi:10.1016/j.ejca.2020.09.028
- Zou C, Huang Y, Ma Y, Yang F, Fu D. Re: a systematic review and meta-analysis: the effect of active cancer treatment on severity of COVID-19: clinical outcomes of SARS-CoV-2–infected cancer patients undergoing surgery. Eur J Cancer. 2021;152:245-247. doi:10.1016/j.ejca.2021.04.011
- Yekedüz E, Utkan G, Ürün Y. Response to letter entitled: re: a systematic review and meta-analysis: the effect of active cancer treatment on severity of COVID-19. Eur J Cancer. 2021;152:248-249. doi:10.1016/j.ejca.2021.04.010