- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Spotlights From Our Cochairs: Kashyap Patel, MD, Talks Value-Based Care, Effects of COVID-19 on Cancer Care Delivery
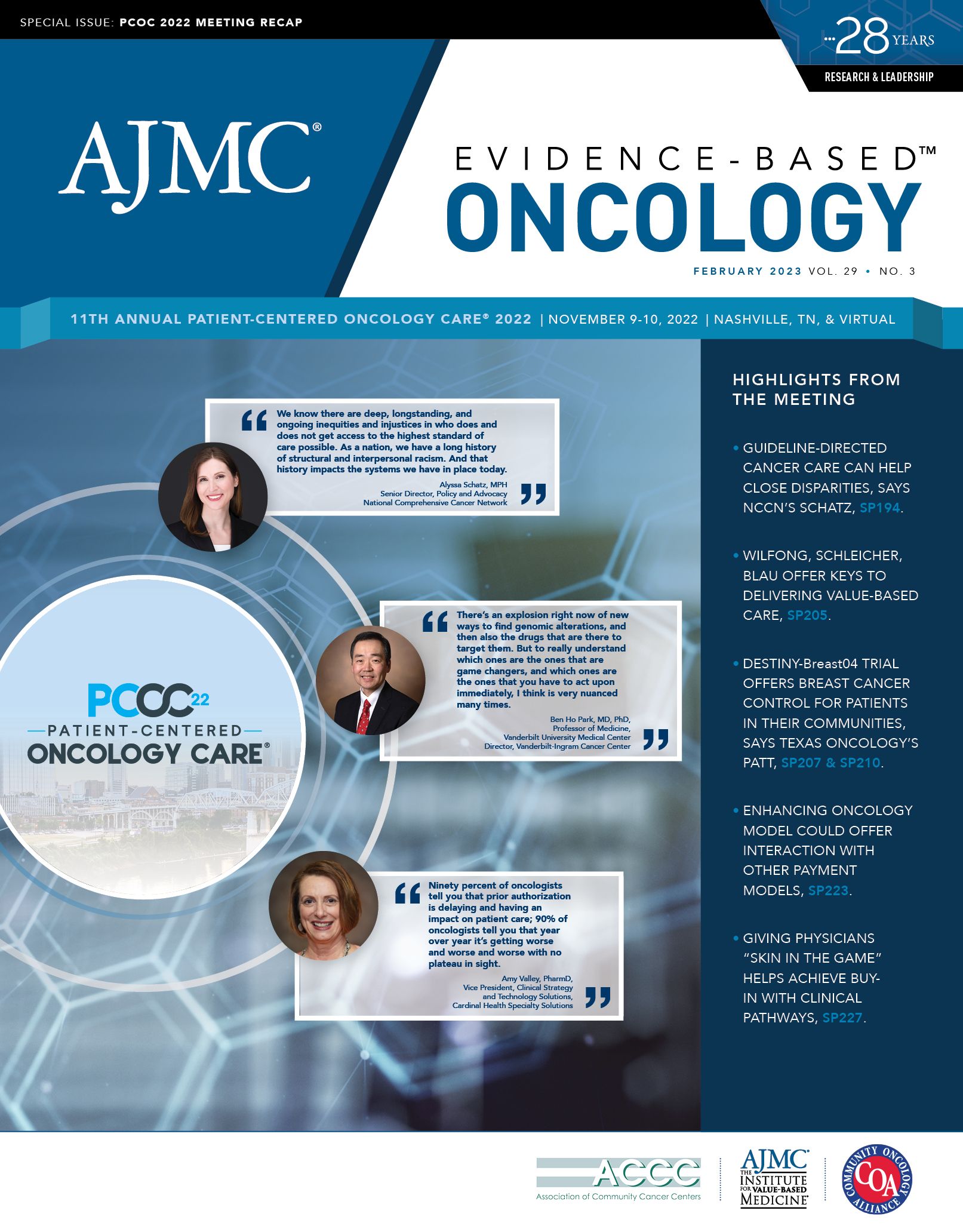
Kashyap Patel, MD, immediate past president of Community Oncology Alliance (COA) and CEO of Carolina Blood and Cancer Care Associates, based in South Carolina, served as a cochair of the 11th Annual Patient-Centered Oncology Care® (PCOC), held November 9-10, 2022, in Nashville, Tennessee. He spoke with Evidence-Based Oncology™ (EBO) about the PCOC theme, “Equity Equals Access for All,” which aligned with Patel’s initiatives as president of COA during 2020-2021, when he highlighted disparities in cancer care delivery and implemented a program to deliver novel therapies to patients with limited financial means.
EBO: What common themes emerged during the discussions at PCOC 2022?
Patel: For the [past] 10 years since the Affordable Care Act was enacted, [creating] CMMI [Center for Medicare and Medicaid Innovation], we started learning about shift from the fee-for-service to the value-based care. That was a whole theme about the evolution of patient-centered care. But we still are in the learning process for understanding what patient-centered care should look like, and there are parts of that which are access to care, equity, diversity, and value—value, which is, it just the cost, or is it the value to the patient as well?
So, we are learning how to define, what is the value to the patient? What is the value to the system? What is value to the doctors? The whole theme of patient-centered oncology care has multiple facets to that, beginning from stakeholders, which is like the pharma industry, the physicians delivering the care, the patients receiving the care, and the payer paying for the care. And it’s nothing that can be learned overnight. It’s almost like doing a phase 1 trial in population health. And we are slowly and steadily learning about, how do you define what is most important part? For example, looking at the alternate payment model, that is one way that stakeholders like the physicians, CMS, as well as manufacturers can come together on one common theme of defining what that kind of part looks like.
EBO: Why is it important to include diverse perspectives from payers and providers in the conversation around patient-centered care?
Patel: About 15 years [ago], we barely had 1 or 2 drugs that were in oral [therapy] space. But now, about maybe 4 out of 10 drugs in oncology the space are in oral drugs, and they’re under the control of the pharmacy benefit managers [PBMs]. What we’re learning now is that the frequent issues that arise out of the PBM step edit, preferred drug list, all of that, can really interfere and really cause issuesS in a very, very serious way for access to care. So, if I’m defining the patient-centered care, but if I cannot have access to a drug that patient wants, it doesn’t make any sense.
Physicians are in the position to take control, and then we are looking at the legislation at state level because federal level may be too hard—there are too many lobbying groups, there are too many special interest groups—but, at state level, definitely. For example, Texas, [South Carolina], Tennessee, all the states are taking action to ensure that there is kind of unfettered, unhindered access to oral drugs, which is [approximately] 4 out of 10 patients now for cancer care. It’s very important to include that part in the light of where the oncology care is moving.1
EBO: How has COVID-19 impacted patient-centered oncology care initiatives?
Patel: Two and a half years of pausing delivery of care really helps us understand how we can sustain the delivery of care, telehealth, and all of that. But what worries me now—and we’ve not factored this into, which I probably will bring up in discussion—is that we don’t know the impact of COVID-19, the chronic COVID-19 on ongoing delivery of care.
Cancer patients in particular are very vulnerable to get COVID-19, and they’re also vulnerable to complication, and COVID-19 increases the cost of care because of the multiple comorbidities [such as] brain fog, lung complications, [and] neuropathy. There are some studies about vulnerability of cancer patients or much worse prognosis as well. So, in the next 5 to 10 years of ongoing discussion about the value-based care, quality of care, and health care quality, it’s important to factor in unexpected circumstances like COVID-19’s impact on the delivery of care.
Reference
Russell C, Nubla J. The increased approval of oral oncolytics: 1995-2018. Presented at: National Community Oncology Dispensing Association. Spring Forum, April 28-30, 2021. https://www.ncoda.org/wp-content/uploads/2021/05/Russell-The-increased-approval-of-oral-oncolytics.pdf
Blister Packs May Help Solve Medication Adherence Challenges and Lower Health Care Costs
June 10th 2025Julia Lucaci, PharmD, MS, of Becton, Dickinson and Company, discusses the benefits of blister packaging for chronic medications, advocating for payer incentives to boost medication adherence and improve health outcomes.
Listen
