- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
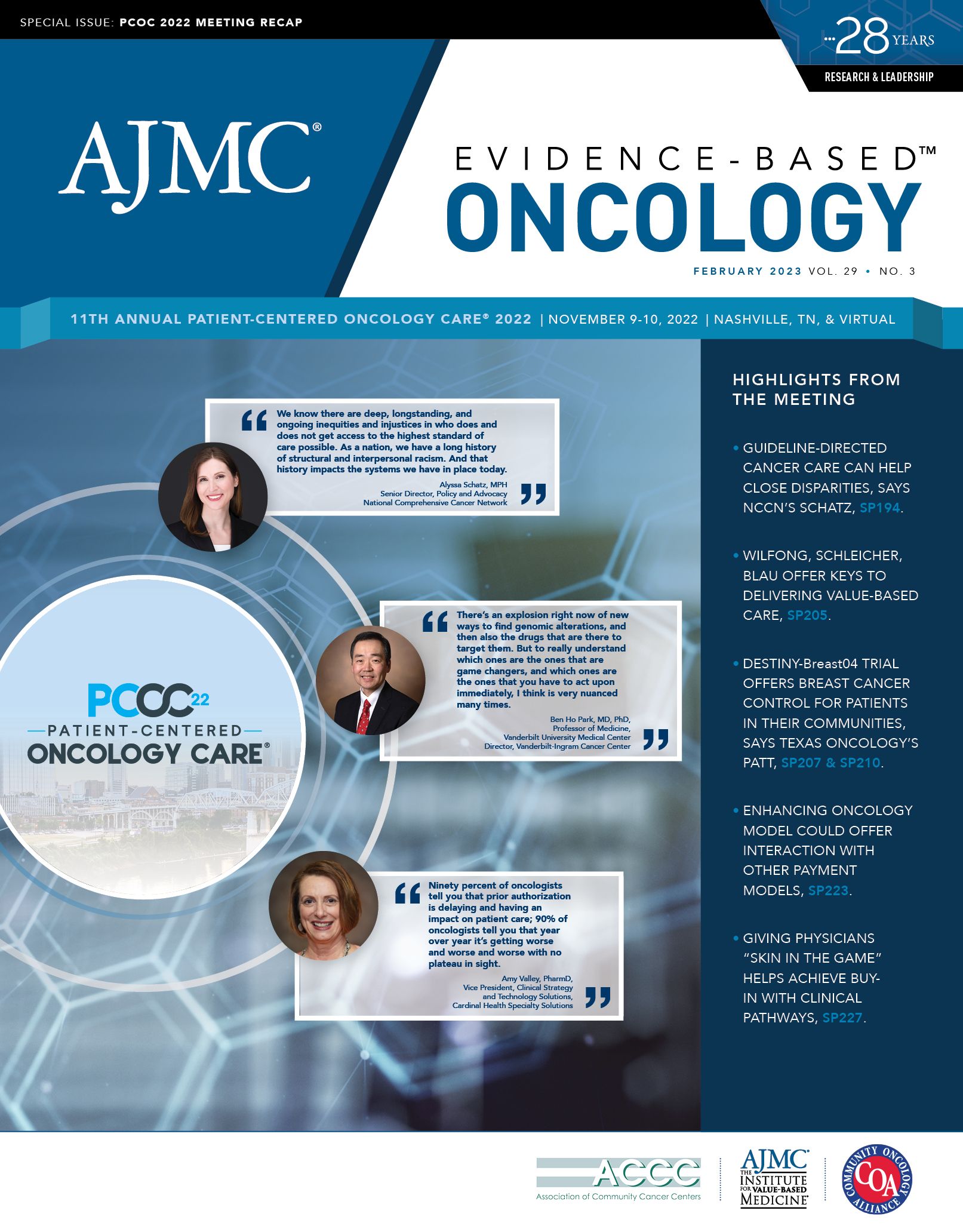
Guideline Adherence “Can Make a Real Difference in Someone’s Life,” Schatz Says
Guidelines from the National Comprehensive Cancer Network (NCCN) offer multiple benefits for providers, payers, and patients, according to Alyssa Schatz, MSW, senior director of policy and advocacy for NCCN. Schatz was also a featured speaker at the Patient-Centered Oncology Care® 2022 meeting held in Nashville, Tennessee. During the conference, she spoke with Evidence-Based Oncology™ (EBO) about the importance of guideline adherence.
This interview has been edited for clarity and length.
EBO: How does guideline adherence reduce patient costs for breast cancer?
Schatz: Guideline adherence has been shown not only to improve outcome measures, including overall survival and quality-of-life measures, but also to reduce cost across a variety of cancer types, including breast cancer. There was a study done by UnitedHealthcare that found [that by] employing a real-time clinical decision support mechanism, they were able to ensure guideline adherence and reduce denials from 7% to 1% among their patient population, which increased access to care. Despite increasing that timely access to care and reducing administrative burden, UnitedHealthcare was able to reduce drug costs to trend by 20%. At that time, drug costs were increasing by 10% nationwide, as well as within that region. And for United Healthcare, for that population, they decreased by 10%. That was a savings of $5.3 million. That was for chemotherapy costs, specifically, across a variety of cancers.1
CVS Health has also looked specifically at [patients with] breast cancer in both the commercial and the Medicare populations, and [they] also found significant cost savings by implementing a clinical decision support mechanism to ensure guideline adherence among that population and the commercial population. [They] saw savings of 25% to 28%. In the Medicare population, they saw a savings of 43%. So, we know this can reduce costs. The great thing is [that] it’s also a win-win, because patients are getting better access to better care.2
This also makes a difference in a patient’s out-of-pocket costs. There’s a study by Williams [et al] that found patients with breast cancer who receive guideline-adherent care saved [approximately] $1800 on average compared with patients who receive guideline-nonadherent care. So, in addition to improving outcomes, improving access, [and] reducing cost to the system, we know it can also reduce cost to the patient. That can make a real difference in someone’s life.3
EBO: Have you found similar results in lung cancer?
Schatz: Guideline adherence has been shown to reduce costs and improve outcomes across a variety of cancer types, [and] it’s no different in non–small cell lung cancer. In a study done by CVS Health through their CVS transformed oncology model, which used a NovoLogix decision support mechanism, they were able to increase guideline adherence from 60% at the beginning of the project to 81%, which is fantastic. By doing that, they were able to reduce costs and non–small cell lung cancer among [patients with] Medicare Advantage by 27%. That represents a huge cost savings, as well as an improvement in care and quality of care.4
EBO: Can you discuss how adherence to NCCN guidelines can address health equity?
Schatz: In addition to improving quality of care and reducing costs, we’re increasingly seeing some studies coming out that show controlling for guideline adherence may also be a promising tool to improve equity in cancer care. It’s just 1 tool in what needs to be a much larger toolbox, and we recognize that, but we are excited by some of the studies we’re seeing.
One study was conducted in the [Veterans Affairs] Medical Center setting, and as a result, they were able to very closely control for guideline adherence that was looking at laryngeal cancer specifically. They had [more than] 200 patients that were monitored for guideline adherence. Within that study, there were no differences across race in terms of who did not receive guideline-adherent care. There also were no differences in terms of outcomes, including overall survival, across race. So we know that when we do this, it can be [a] factor that improves equity. There was another study done across non–small cell lung cancer, prostate cancer, and breast cancer that found that there were differences across race in terms of guideline adherence, using Medicare C data. When they were able to control for guideline adherence, they found that those elevated hazard ratios for all-cause mortality were reduced, essentially, to eliminate the disparities that had existed. When they controlled for who did not receive guideline-adherent care across race, they were able to essentially eliminate disparities.
EBO: Are any incentives emerging to encourage providers to adhere to guidelines, or at least to eliminate barriers to using them?
Schatz: There have been a number of payers who have moved toward clinical decision support mechanisms, recognizing that this is a model that can improve care and timely access to care without harming access, [as well as reduce] costs. That’s one excellent strategy in lieu of traditional prior authorization, which can sometimes be harmful and lead to delays in care.
Using real-time clinical decision support is a great strategy. A piece of legislation that’s out right now on Capitol Hill is the Improving Seniors’ Timely Access to Care Act.5 That would require Medicare Advantage plans to use these real-time prior authorization tools. If that legislation passes, it may be one shift and trend to help us get closer to real-time clinical decision support. That also introduces greater transparency into prior authorization, to be friendly to patients, as well.
In addition to clinical decision support mechanisms, we’re also seeing some trends within value-based models of care. The [Oncology Care Model] included a requirement for guideline attestation, [and] the Enhancing Oncology Model requires that as well. [However], for providers who are participating in those value-based models of care, it’s going to be really important to not [only] test but [to] also look at the systems you have in place to make sure you are adhering to guidelines. It’s a way to make sure you’re reducing your costs while also improving your quality of care and your care outcomes. It’s a win-win for anyone who’s in a value-based model.
EBO: How does guideline adherence help with focusing on putting the patient first?
Schatz: I’m so glad you mentioned that. From a patient-centered perspective, we need to do a better job of getting these tools into patient’s hands so they’re empowered to ask their provider, “What’s the evidence for my care? How does this fit into guidelines?” We can promote those shared decision-making conversations. At NCCN, we have patient versions of our guidelines, so it’s all the same content as what is outlined in our guidelines but in a patient-friendly format for nonclinicians to be able to use. That’s something we’re trying to do a better job [at], making sure we’re getting those into as many patients’ hands as possible, so they’re empowered to have those conversations.
Editor’s Note: The Improving Seniors’ Timely Access to Care Act passed the House of Representatives but was not taken up by the Senate before the end of the 117th Congress.
References
1. Newcomer LN, Weininger R, Carlson RW. Transforming prior authorization to decision support. J Oncol Pract. 2017;13(1):e17-e61. doi:10.1200/JOP.2016.015198
2. Sapkota U, Cavers W, Reddy S, Avalos-Reyes E, Johnson KA. Total cost of care differences in National Comprehensive Cancer Center (NCCN) concordant and non-concordant breast cancer patients. J Clin Oncol. 2022;40(suppl 16):e18833. doi:10.1200/JCO.2022.40.16_suppl.e18833
3. Williams CP, Azuero A, Kenzik KM, et al. Guideline discordance and patient cost responsibility in Medicare beneficiaries with metastatic breast cancer. J Natl Compr Canc Netw. 2019;17(10):1221-1228. doi:10.6004/jnccn.2019.7316
4. Yeon H, Brito RA, Kong W, et al. Impact of a regimen-level prior authorization tool on provider adherence to clinical guidelines’ and cost savings in a Medicare advantage population. J Clin Oncol. 2021;39(suppl 15):1522. doi:10.1200/JCO.2021.39.15_suppl.1522
5. Improving Seniors’ Access to Care Act of 2021, HR 3173, 117th Cong (2021-2022). Accessed January 26, 2023. https://www.congress.gov/bill/117th-congress/house-bill/3173
Telehealth Intervention by Pharmacists Collaboratively Enhances Hypertension Management and Outcomes
January 7th 2026Patient interaction and enhanced support with clinical pharmacists significantly improved pass rates for a measure of controlling blood pressure compared with usual care.
Read More
Exploring Racial, Ethnic Disparities in Cancer Care Prior Authorization Decisions
October 24th 2024On this episode of Managed Care Cast, we're talking with the author of a study published in the October 2024 issue of The American Journal of Managed Care® that explored prior authorization decisions in cancer care by race and ethnicity for commercially insured patients.
Listen
