- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
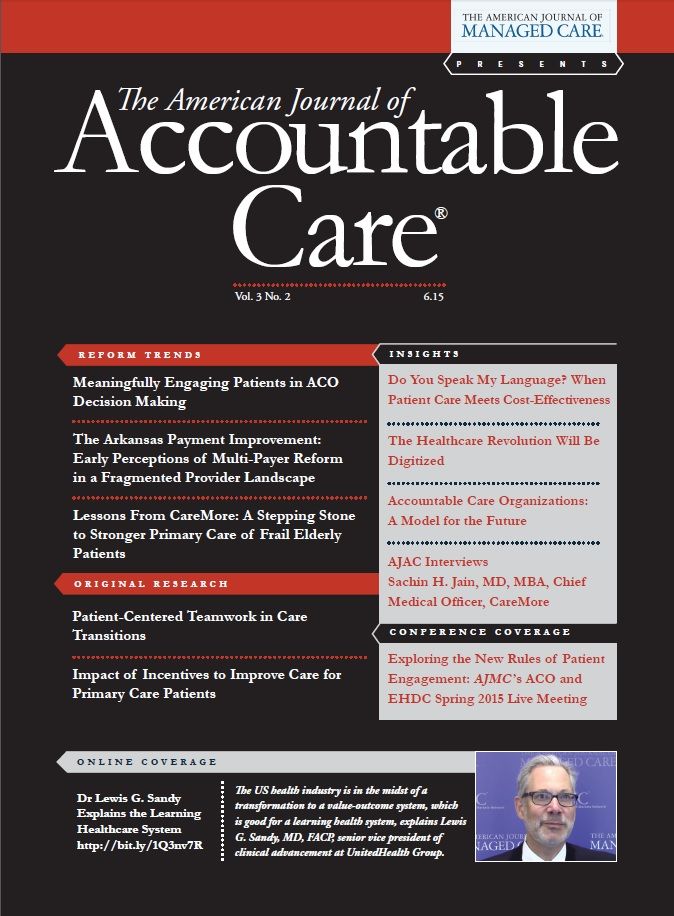
Lessons From CareMore: A Stepping Stone to Stronger Primary Care of Frail Elderly Patients
CareMore, an insurance plan based in southern California, has reduced costs and improved outcomes by providing direct care for its frailest elderly patients.
ABSTRACT
CareMore, a Medicare Advantage insurance plan originating in southern California, provides direct care for its frailest elderly patients and has developed an integrated patient care delivery system designed to surround patients with care. The system is based on extensivists, hospital-based physicians who also see patients for 1 or more follow-up outpatient visits; a cadre of nurse practitioners who manage specific chronic conditions by protocol; and a corps of nurse care managers who manage banks of remote home monitoring data and develop trusting relationships with patients. Early data from this system suggest better outcomes at lower costs: patients experience 42% fewer hospital admissions than the national average, an amputation rate among diabetic patients that is 60% lower than the national average, and a 4% pressure ulcer rate in institutionalized patients compared with a 13% rate for the entire state of California. Per member per month spending is less than expected under a CMS model for similar risk patients. For patients in the intermediate risk category, the actual cost is $1000 versus an expected cost of $1500. For the highrisk group, the actual cost is $2250 versus an expected $3500.Twenty percent of the elderly population consumes 80% of Medicare resources.1 The majority of these patients are chronically ill and living at home or in a nursing home. In many communities, the care this sickest segment receives is fragmented and disorganized, with patients moving from one doctor to the next without communication or coordination, often resulting in frequent, potentially avoidable hospitalizations. By focusing on this high cost, high-need population, CareMore has increased independent living for frail elderly, reduced rates of hospitalization and total costs of care, and improved care for elderly patients with diabetes, heart failure, and other chronic illnesses.
History
CareMore began as a medical group in southern California that aimed to manage its patients by coordinating their care, and has had more than a decade of experience in shared savings arrangements. Between 2008 and 2010, CareMore expanded to Las Vegas, Tucson, Phoenix, and San Jose, High Desert, and Modesto. CareMore was purchased by Wellpoint in 2011, and expanded to Richmond, Virginia in 2013. Through each of these expansion phases, the organization learned that a large upfront investment in care managers, medical assistants, home monitoring devices, and on-site services can provide a substantial return on investment measured in avoided hospital and procedural costs.
The CareMore Model
Figure 1
CareMore’s mission is “to address the complex problems of aging while protecting the precious financial resources of our members and the federal government.” The CareMore model is designed to provide insurer-based, intensive, coordinated co-management to the sickest 20% of the senior population. The model is based on nurse care managers, nurse practitioners (NPs), and extensivist physicians (). The nurse care managers and NPs provide intensive outpatient management for patients with a set of common chronic conditions. The extensivists provide inpatient management for hospitalized CareMore patients, along with post hospital outpatient management for the sickest 5% of patients. The extensivists also coordinate all medical care for the frailest members, and in addition, perform fall risk and elective preoperative evaluations, make rounds at skilled nursing facilities, and evaluate and treat all members identified as high risk based on a predictive model applied during the initial healthy start visit.
Selection for Intensive Ambulatory Services
Each patient has a “Healthy Start” appointment on enrollment with CareMore, followed by an annual “Healthy Journey” appointment with a nurse practitioner or physician. During this 1-hour visit, the patient receives a health risk assessment and is screened for fall risk, depression, dementia, and functional status, as well as undergoes laboratory evaluation, including hemoglobin A1C testing, lipid panel, comprehensive metabolic panel, hemoglobin and urine testing.
Using a combination of predictive modeling, laboratory data surveillance, physician referrals, and patient self-identification, CareMore physicians identify patients most at risk for high-cost care and enroll them in one of the CareMore centers for disease-specific management. For example, CareMore nurse care managers scan the clinical laboratory database for patients with poorly controlled diabetes, chronic kidney disease, and signs of malnutrition, and subsequently reaches out to enroll them in intensive management.
Intensive Outpatient Management: “Surrounding With Care”
Approximately 30% of CareMore patients are referred to NP-run disease-specific management programs for chronic obstructive pulmonary disease, diabetes, heart failure, or hypertension. There are also Coumadin, wound, and podiatry clinics, an exercise and strengthening program, and a pharmacist-run multiple medication clinic for intensive medication management. The NPs treat their patients’ chronic conditions according to established protocols. A patient who has more than 1 chronic condition will see only 1 NP who, working from multiple disease management protocols, preserves a “one-touch” personalized approach for the patient. Each NP is paired with 2.5 medical assistants (MAs), who perform clinical tasks such as diabetic monofilament testing, Patient Health Questionnaire-9 depression screening, and immunizations.
Patients are seen frequently in the disease management clinics and contacted often between visits, until they have reached their disease-specific target—usually within 6 months. Once patients reach their goals (eg, glycated hemoglobin [A1C] less than 7.5%) they are discharged from the program to their primary care provider (PCP), although their data are still monitored and they may re-enter intensive disease management in the future should their conditions require.
Home Monitoring
Patients triaged to the heart failure or hypertension disease management programs receive a scale, a blood pressure kit, and a wireless modem that transmits data to the CareMore remote monitoring nerve center, staffed by NPs. Nurse care managers review incoming data from each patient. Blood pressure readings are reported twice daily and weight once daily. A 2-pound weight gain triggers a phone call from the patient’s NP who titrates medications according to protocol.
Nurse care managers also call the patients after discharge to check on any questions or problems on return home. The role of the care manager is to be a conduit between the patient and the clinician and to help gain patient trust; the goal is for the patient to have a strong bond with the care manager so that they will call him or her rather than 911 when a question arises.
Care manager extenders, who may be medical assistants or workers without specific clinical training, also play an important role, performing many of the clerical tasks associated with phone management, durable medical equipment authorizations, and communicating with the hospital-based care manager. Care manager extenders may also make a home delivery and set-up of the remote monitoring equipment. There are typically 2 care manager extenders assisting each nurse care manager.
Homecare Intervention SWAT Team
CareMore recognizes that many hospitalizations occur for social reasons, and has put together a homecare intervention SWAT team to reduce such hospitalizations. The SWAT team consists of 2 NPs, a licensed vocational nurse, and 1 physician dedicated exclusively to making house calls. In addition, a team of social worker, case manager, mental health clinician, and even an attorney is available for home visits. The team might help a patient with rheumatoid arthritis to obtain prescriptions in non-childproof bottles, arrange for free transportation to the clinic for a socially isolated patient, or intervene in family and legal matters that interfere with the patient’s health.
Hospitalization
Extensivist physicians provide hospital care to CareMore patients. At discharge patient records are color-coded. Red signifies a high need patient who will receive a nurse call within 24 hours of discharge and an appointment at the CareMore Center with their extensivist within 48 hours of discharge. Yellow signifies a patient who needs a call within 48 hours and an appointment with their extensivist within 1 week. Green signifies a stable patient whose follow-up will be with the patient’s primary care physician (PCP) and for whom no follow-up phone call is necessary.
Post Hospital Extensivist Follow-up
Extensivist physicians see most hospitalized patients at least once after discharge, and then turn the care back to the patient’s PCP. For the sickest 5% of the CareMore population—those most at risk for readmission—the extensivists see the patient on an ongoing basis and continue to co-manage with the patient’s PCP indefinitely.
Interface With Non-CareMore Physicians
CareMore physicians, NPs and care managers do not provide 100% of the care to CareMore patients; all CareMore patients are co-managed with their PCPs, even while in a phase of intensive disease management. PCPs in the CareMore network have an average of 75 CareMore seniors in their panel of patients. These PCPs are paid a capitated rate for the care of these patients, with additional incentive programs which encourage utilization of the CareMore chronic disease management programs. Quality measures such as Healthcare Effectiveness Data and Information Set (HEDIS) scores and emergency department visits are also included in the incentive program.
In southern California, CareMore employs its own cardiologists, pulmonologists, and dermatologists. As membership grows, CareMore may consider moving toward employed subspecialists in other markets. Most other subspecialists are paid on a fee-for-service basis, and are chosen for quality, accessibility, and their ability to work within the CareMore philosophy—for example, their commitment to follow evidence-based treatment guidelines, and to take the entire patient’s health status into account.
Staffing
Staffing varies by factors such as geographic concentration of members and maturity of the market. In general, a CareMore team of 2 extensivist physicians, 2 to 4 NPs, 2 to 3 case managers and 14 MAs, along with a nutritionist, social worker, and pharmacist provides the hospital and intensive outpatient management for the sickest quintile of patients within a “neighborhood” of 4000 to 5000 covered patients. At any given time, an NP typically has a panel of approximately 400 patients and an extensivist has a panel of 100 patients; panel size varies based on network composition, market maturity, and disease burden.
Data
Physicians and their teams are provided data to modify their practices. For example, on a monthly basis, readmission rates, hospital length of stay, wounds, and urinary tract infections are reported to the provider. In addition to the HEDIS measures, CareMore also tracks 114 clinical measures quarterly, such as average A1C and low-density lipoprotein levels, amputation rate, heart failure patients on ACE inhibitors, percentage of anticoagulated patients within therapeutic INR range, percentage of patients with heart failure enrolled in a heart failure program, and the percentage of patients with optimal A1C range after enrollment in a diabetes clinic.
On-site Exercise Facilities
Patients enrolled in any of CareMore’s insurance products have free access to the “Nifty after Fifty” exercise facility, located in a building adjacent to the center. Patients receive a customized exercise plan, prescribed by an exercise physiologist, programmed into their “key.” Patients place their key in each exercise machine, and the key triggers their individualized program; it also records their workout, which is later downloaded and sent back to their PCP. Nifty after Fifty also includes a physical therapy facility.
Results
Figure 2
Preliminary data suggest better outcomes at lower costs for CareMore patients: 42% fewer hospital admissions than national average; an amputation rate for diabetic patients 60% lower than national average; a 4% pressure ulcer rate in institutionalized patients compared with an average of 13% for the state of California. Per member per month (PMPM) spending is less than expected under a CMS model for similar risk patients: for patients in the intermediate risk category the actual cost is $1000 compared with an expected cost of $1500 PMPM. For the highest risk group the cost is $2250 PMPM compared with an expected cost of $3500 PMPM ().
What is it Like to Work at CareMore as a Physician?
CareMore physicians are not the downtrodden, overworked, under-supported PCPs so typical in many organizations. CareMore physicians work 40-hour weeks and spend the majority of their time caring for sick patients. CareMore extensivists are paid a base pay between $200,000 and $220,000 annually. With bonuses and other benefits, the average compensation by year 2 of employment is greater than $300,000. A typical CareMore physician schedule is in Figure 1.
What is Missing?
CareMore provides an impressive array of support services for patients. The model would be stronger with utilization of devices to increase medication adherence, such as a pharmacy-filled “med buddy” that reminds patients to take their medications at the appropriate time. CareMore staff members also look forward to having mental health counseling on site and to having interoperative records between the hospitals, PCP offices, and the CareMore center. Currently, for example, care manager extenders (MAs) manually transfer data from hospital systems to CareMore’s electronic health record. Some network PCPs would prefer not to receive voluminous notes and are sent summaries of the key interventions and findings.
Limitations
The CareMore model may be ideally suited to markets where existing care is splintered. While it has also been successful competing in markets with existing integrated networks, such networks may themselves be able to deliver similar care within their existing organization. The CareMore leadership also identifies the initial investment costs, and the requirement for smaller, well-organized PCP and subspecialty networks as a limitation.
Generalizability
While CareMore is a delivery arm of an insurance provider, there are lessons for the rest of the country in its model. For patients there is wrap-around care, and details are not left to chance. For example, the patient isn’t just advised to get a scale to do daily weights, the MA brings a scale to the home, sets up the remote monitoring system, and a nurse monitors the results.
For the physicians, there is remarkably less waste of physician resources than in a typical primary care practice. Whereas most generalist physicians in the United States are teamed with 1 MA, and devote a substantial portion of their day to lower-value documentation, billing, and clerical functions, CareMore physicians are each part of a team with an average of 2 NPs, 2 nurse case managers, and 7 MAs per physician. This larger but still socially integrated team extends the physicians’ reach. To the authors’ observation, CareMore physicians’ morale was higher than that of most generalist physicians. We suspect this comes from their working in a setting that allows them to spend most of their effort on physician-level work.
CareMore has much to teach the rest of us about the care of complex, chronically ill elderly: frequent contact, home monitoring, NP and case manager run protocols, and a culture that promotes aggressive, low-cost interventions over expensive, high-tech interventions.
Conclusion: The Way Forward
Many hospitals and clinics are oriented toward attracting relatively healthy patients for high-cost, high-margin services such as radiation therapy, orthopedic procedures, or interventional cardiology. Physicians delivering these high margin services are paid well and are typically surrounded by a team of support staff to help maximally leverage their skills and training.
Yet in most communities, services for the frail elderly are delivered on a limited budget, sometimes in crowded, unattractive settings, by physicians who are paid the least among their peers. Physicians providing this care often work without much clinical support, and consequently, spend much of their day on non—physician-level work (ie, locating information, calling payers for prior authorizations, and typing the visit note). This is not a formula for optimizing the clinical outcomes and financial health of the US healthcare system. Burnout is common and coordination with other points within the healthcare system is spotty and inconsistent—a complex patient is a liability to be avoided.
CareMore, by contrast, actively seeks out the sick and vulnerable, and has built systems to coordinate their complex care. CareMore is delighted to enroll the homebound, fragile 78-year-old with emphysema, diabetes, and chronic venous ulcerations. CareMore wants the confused 84-year-old who cannot keep track of her medications, has little social support and who has been hospitalized twice within the past year. CareMore is not a low-budget, charitable organization. Rather it is a highly successful, entrepreneurial enterprise in a setting where the financial incentives allow them to do well taking good care of sick people. As an insurance company, it is a risk bearer that has invested heavily in upfront chronic illness care to reduce the total global costs of care for its population. The CareMore experience highlights some of the dysfunctions in the current reimbursement system and points the way toward a model of care that benefits patients, is sustainable for the physicians and staff providing the care, and cost-effective for those who finance the care.AUTHORSHIP INFORMATION
Author Affiliations: Medical Associates Clinic and Health Plans (CS, TS), Dubuque, IA.
Source of Funding: None.
Author Disclosures: Dr Christine Sinsky serves on the advisory board of healthfinch, where she has a minimal stock option; she is also the vice president of Professional Satisfaction at the American Medical Association. Both authors have consulted with healthcare organizations on practice redesign and have received honoraria for grand rounds presentations.
Authorship Information: Concept and design (CS, TS); acquisition of data (CS, TS, and CareMore staff); analysis and interpretation of data (CS, TS, and CareMore staff); drafting of the manuscript (CS); critical revision of the manuscript for important intellectual content (CS, TS); statistical analysis (CareMore staff).
Address correspondence to: Christine A. Sinsky, MD, Medical Associates Clinic and Health Plans, 1000 Langworthy St, Dubuque, IA 52001. E-mail: csinsky1@mahealthcare.com.REFERENCES
1. Conwell LJ, Cohen JW. Characteristics of people with high medical expenses in the U.S. civilian noninstitutionalized population, 2002. Statistical brief #73. Agency for Healthcare Research and Quality, Rockville, MD. http://meps.ahrq.gov/mepsweb/data_files/publications/st73/stat73.pdf. Published March 2005. Accessed April 28, 2015.
Quality of Life: The Pending Outcome in Idiopathic Pulmonary Fibrosis
February 6th 2026Because evidence gaps in idiopathic pulmonary fibrosis research hinder demonstration of antifibrotic therapies’ impact on patient quality of life (QOL), integrating validated health-related QOL measures into trials is urgently needed.
Read More
Building Trust: Public Priorities for Health Care AI Labeling
January 27th 2026A Michigan-based deliberative study found strong public support for patient-informed artificial intelligence (AI) labeling in health care, emphasizing transparency, privacy, equity, and safety to build trust.
Read More
Ambient AI Tool Adoption in US Hospitals and Associated Factors
January 27th 2026Nearly two-thirds of hospitals using Epic have adopted ambient artificial intelligence (AI), with higher uptake among larger, not-for-profit hospitals and those with higher workload and stronger financial performance.
Read More
Motivating and Enabling Factors Supporting Targeted Improvements to Hospital-SNF Transitions
January 26th 2026Skilled nursing facilities (SNFs) with a high volume of referred patients with Alzheimer disease and related dementias may work harder to manage care transitions with less availability of resources that enable high-quality handoffs.
Read More

