- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Infrastructure of OCM Helps Practices Through COVID-19
The keynote address at Patient-Centered Oncology Care® 2020 focused on the way practices have benefitted from the Oncology Care Model as the pandemic wears on.
Nothing about taking care of patients with cancer during the coronavirus disease 2019 (COVID-19) pandemic has been easy, but those practices that had already embraced transformation under the Oncology Care Model (OCM) are finding that its monthly payments and other features off er stability during an unprecedented health emergency.
That’s what Alexandra Chong, PhD, lead for the OCM within the Center for Medicare and Medicaid Innovation (CMMI), told the hundreds of online attendees on September 25, 2020, as she kicked off the 9th annual meeting of Patient-Centered Oncology Care®, the marquee annual event presented by The American Journal of Managed Care®.
“We are living in a totally different world,” said event Cochair Kashyap Patel, MD, who is CEO of Carolina Blood and Cancer Care Associates of Rock Hill, South Carolina, as he introduced Chong. “What we are learning is how COVID-19 impacts not just us as what we do in the office, but how it impacts the rapid adaptation and changes from the payer perspective.”
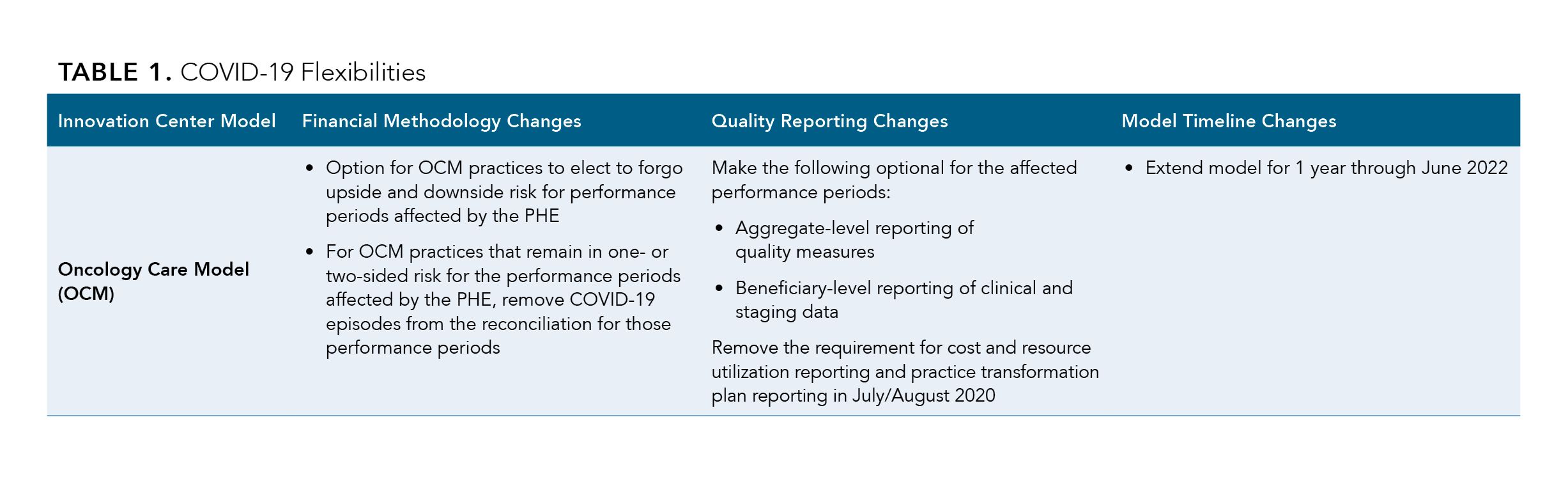
Chong spent much of her talk walking attendees through the fine points of the OCM, which had been poised to transition on January 1, 2021, to Oncology Care First (OCF), a next-generation model built on a bundled-payment framework instead of fee-for-service (FFS). As Chong explained, due to COVID-19, the OCM was extended another year through 2022, and CMMI has not yet fleshed out the details of OCF.
OCM is “an episode-based model,” Chong said, one that attaches 2 reimbursement elements to each practice’s commitment to reach certain financial and quality benchmarks while meeting practice standards that include having 24/7 access to medical records and developing care and survivorship plans with patient input. Although the number of practices in the OCM is 138, the number of physicians involved exceeds 7000, and the model now reaches 150,000 Medicare patients each year, or about a quarter of all FFS beneficiaries with cancer. Practices in the OCM receive $168 per patient per month in Monthly Enhanced Oncology Services (MEOS) for delivering this higher-level care, as well as Performance-based Payments which come after each
6-month evaluation period ends. As Chong explained, the work that practices undertook to redesign their procedures for the “high-touch” requirements of the OCM was not easy—and a
learning process for both sides. But it’s paying dividends now. Practices that rely on administering expensive therapies—and having new patients walk through the door—have seen revenue plummet as people skip cancer screenings. But those in the OCM have had some lifelines.
“We decided to retain the billing and to keep up those MEOS payments, because we have heard across…a majority of our practices, that a lot of the infrastructure that was put into place for the implementation of OCM has really helped our practices in terms of still achieving or [staying focused] on the of their beneficiaries,” Chong said.
For these practices, the time and investment in “practice redesign activities” is paying off. These include (1) enhanced services, including offering patients or other providers 24/7 access to their medical records; (2) utilization data for quality improvement; and (3) providing a reconciliation on what performance looks like during the 6-month episodes in each performance period. Meeting the “high-touch” expectation means practices are connecting with patients more frequently than they might have under prior practice designs.
To be sure, the OCM is not perfect, and Chong said CMMI has heard the message from participating physicians that it must rethink reporting requirements and turn around performance data in a time frame that lets practices fix problems quickly. Because of the epidemic, CMMI has made some data reporting requirements optional during the COVID-19 public health emergency, including aggregate quality measure reporting and beneficiary-level clinical and staging data reporting.
“A majority of our practices still reported on these data, even though doing so was optional,” Chong said.
Before COVID-19 hit, she noted, the OCM was gaining momentum as it headed into its final year. A third of the practices in the model had agreed to take on 2-sided risk or “some type of downside risk,” she said.
By embracing the tools that make the OCM work, Chong said, “Participants have been able to not lose that momentum in providing the high-quality care that they committed to their beneficiaries.
OCM Flexibilities in COVID-19