- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
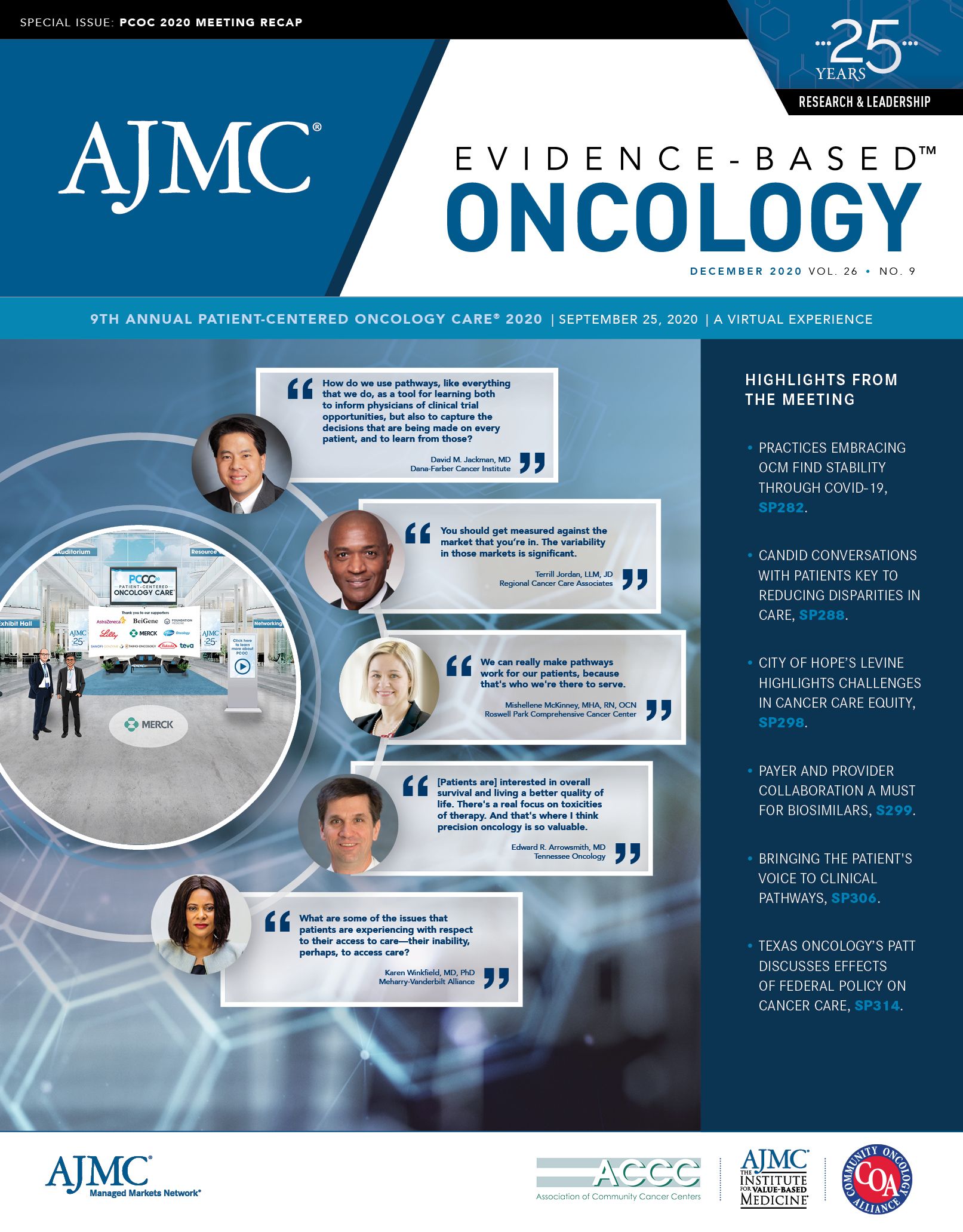
How Federal Policy Decisions Are Influencing Cancer Care
As novel therapies drive up the cost of cancer care, federal policy decisions are being made that influence oncologists' ability to deliver cancer care, said Debra Patt, MD, PhD, MBA, MPH, of Texas Oncology.
With unprecedented progress in treatments, cancer care is evolving into a chronic disease, but the introduction of novel therapies is happening during a time when focus is being placed on how much health care costs. As a result, federal policy decisions are being made that influence oncologists’ ability to deliver cancer care, said Debra Patt, MD, PhD, MBA, MPH, executive vice president of policy and strategic initiatives at Texas Oncology.
During her featured session at The American Journal of Managed Care®’s Patient-Centered Oncology Care® meeting, Patt discussed the current landscape of cancer care delivery, trends in drug pricing, alternative payment models, and more.
Health care costs as a percentage of gross domestic product continues to increase in the United States and is already higher than in any other country, she pointed out. That increase translates to higher out-of-pocket costs for patients and premium contributions by employers to health plans. “Regardless of the value, know that the increase in cost is not sustainable,” Patt said.
There are a number of relevant executive orders on drug pricing, including one on rebates to lower prices by eliminating kickbacks to middlemen, one that allowed for drugs to be imported from Canada, and one to change the mechanism of 340B reimbursement as it pertains to insulin and epinephrine. One executive order where there remains a lot of uncertainty is the so-called International Pricing Index (IPI), which was first announced in 2018.1
After it was introduced, nothing happened with the IPI until September 2020 when President Donald Trump announced the Most Favored Nation Price executive order for Medicare Part B and Part D drugs.2 Under the plan, HHS would create a program through which Medicare paid no more for drugs than the lowest price paid by countries in the Organization for Economic Cooperation and Development. However, the details remain unclear, Patt said. For instance, it’s not clear which drugs will be included or how quickly a pilot might be implemented.
“So, I think that when we look at health care policy changes, abrupt and sudden changes that are drastic to the system are very challenging for the system to continue to operate effectively,” she said. “And I will say that oncology care delivery does happen very effectively.”
Changing how finances are managed is an interest that the current administration shares with the previous administration. The Oncology Care Model (OCM) launched in 2015 under the Obama administration, and it is being extended as Oncology Care First in 2022. Although the early results of the OCM didn’t demonstrate “a tremendous amount of cost savings,” Patt believes that “the jury’s still out.” In addition, CMS isn’t the only entity interested in alternative payment models, as there are more pilots popping up in the commercial space.
“I can say my practice alone has 5 alternative payment model pilots with commercial payers, and they mirror many aspects of the oncology care model,” she said. “So, as we try to make the walk from volume to value in oncology, I think alternative payment model pilots are a really important way to do that.”
The Center for Medicare and Medicaid Innovation also finalized the Radiation Oncology (RO) Model3; however, since Patt’s talk, CMS announced it will delay the model until July 1, 2021.4 The RO Model uses episode-based payments for radiation oncology and includes physician group practices, freestanding radiation centers, and hospital outpatient departments. The model includes several payment episodes for 16 cancer types.
The challenge of the RO Model, compared with OCM, is that the RO Model is mandatory for one-third of ZIP codes. A mandatory pilot is always difficult, but especially so during a time when “cancer care is suffering quite a bit,” Patt said.
The growth of biosimilars is also an incredibly important part of cancer care, as they allow for a switch from an innovator product. However, many biosimilars entering the market presents a challenge as insurance companies pick and choose among the biosimilars. The result can be different insurance companies dictating that the same practice use different biosimilars.
“And it's unrealistic to think that you can keep multiple biosimilars of one particular innovator product in inventory and manage that inventory at a low cost,” Patt explained.
Finally, Patt highlighted that the election outcome may impact health care. The Trump administration’s main focus has been to cut prescription drug prices, and the president has used a lot of executive orders in this area. However, Patt believes that the Biden campaign “actually has a real focus on health care.” While former Vice President Joe Biden also wants to deal with prescription drug prices, his focus has been on access to care and providing a public health option for all to try and create affordable, quality health care and system that is less complex.
“So, I think whether Trump remains in the White House, or Biden is elected to the White House, I think drug pricing [and] cancer care will be center stage, and health care will be a central focus of the election and of the next presidency,” Patt said.
References
1. Joszt L. Trump proposes allowing Medicare to base drug prices on what other countries pay. The American Journal of Managed Care®. October 25, 2018. Accessed October 30, 2020. https://www.ajmc.com/view/trump-proposes-allowing-medicare-to-base-drug-prices-on-what-other-countries-pay
2. White House. Executive order on lowering drug prices by putting America first. White House. September 13, 2020. Accessed October 30, 2020. https://www.whitehouse.gov/presidential-actions/executive-order-lowering-drug-prices-putting-america-first-2/
3. Caffrey M. Too much, too fast: providers push back on CMS’ final RO Model. Am J Manag Care. 2020;26(8 spec no):SP237-SP238.
4. ASTRO. ASTRO responds to CMS announcement on delayed Radiation Oncology Model start date. American Society for Radiation Oncology. October 21, 2020. Accessed November 2, 2020. https://www.astro.org/News-and-Publications/News-and-Media-Center/News-Releases/2020/ASTRO-responds-to-CMS-announcement-on-delayed-Radi