- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
As Practices Await OCF Details, the Question of How to Factor in COVID-19 Emerges
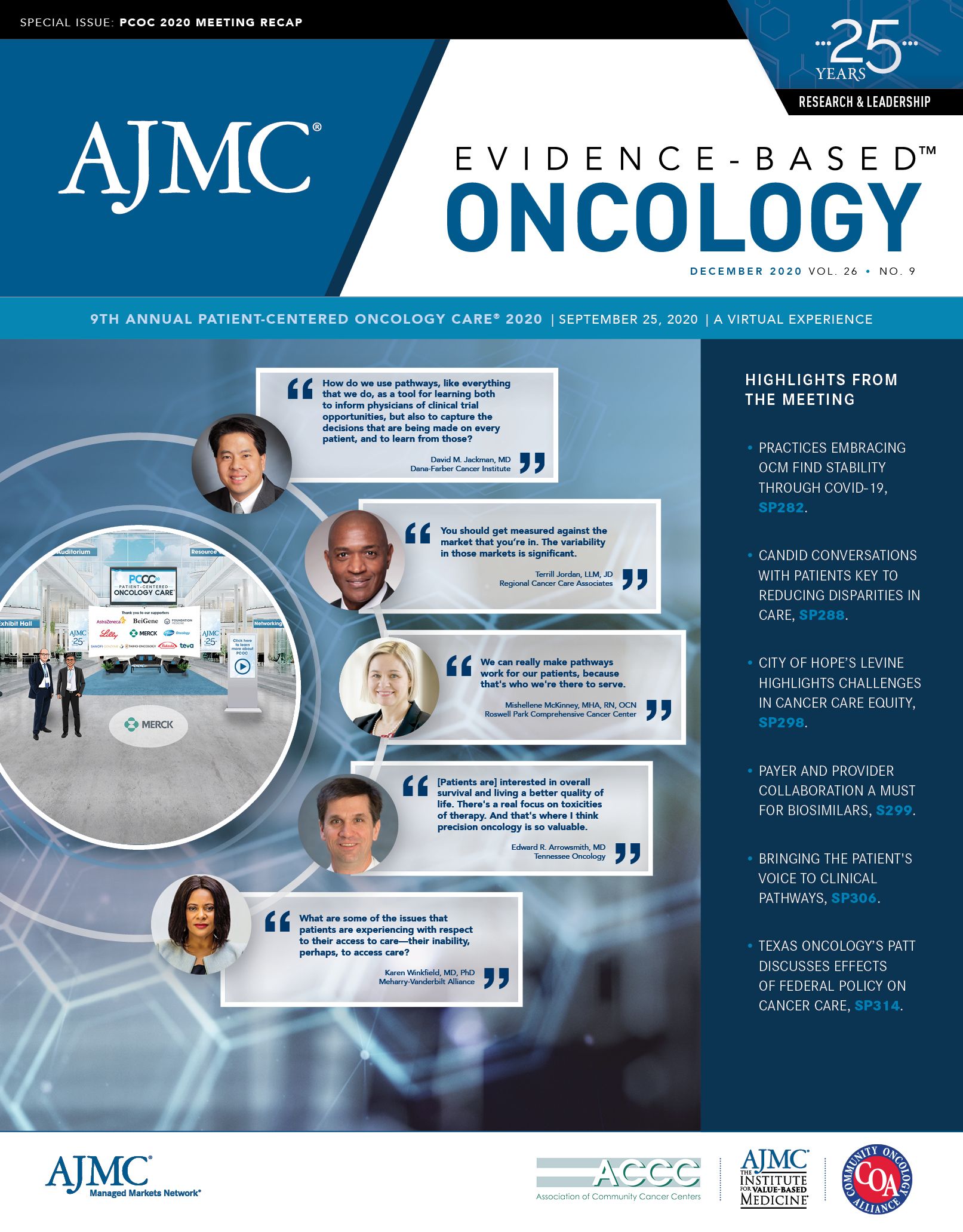
A panel at Patient-Centered Oncology Care® 2020 discussed the challenges of a pandemic as oncology practice transformation initiatives continue on.
As 2020 began, the biggest challenge facing practices in the Oncology Care Model (OCM) was the transition—for some—to 2-sided risk. And that’s still a challenge, but one compounded by a wild card that never factored into anyone’s forecast:
What happens if a global pandemic keeps people from being screened for cancer, and from being diagnosed, and thus from being treated? What if treatment regimens must be redesigned to keep patients out of the office or the infusion center as much as possible?
It’s not a good time to be thinking about moving even further down the payment reform road to Oncology Care First (OCF), and thus the successor to OCM has been delayed until 2022.
All the wild cards of 2020 were part of the discussion as Kashyap Patel, MD, cochair of Patient-Centered Oncology Care® 2020, led a panel discussion on shifting from the OCM to the OCF. Panelists were Aaron Lyss, MBA, director of Strategic Payer Relations, OneOncology; Terrill Jordan, LLM, JD, president and CEO, Regional Cancer Care Associates; Mariam Alboustani, RPh, clinical pharmacy manager, Pharmacy Services, Blue Cross Blue Shield of Michigan; and Randall A. Oyer, MD, medical director of oncology and the cancer institute at Lancaster General Health/Penn Medicine.
Early in the day, Patel likened the OCM to “an architect’s blueprint” of how cancer care should work, one that reflects the time and resources participants have invested to build it. He launched the panel discussion by asking what the OCF should look like when it’s fully presented. Jordan said that the ground has shifted with coronavirus disease 2019 (COVID-19) and the Center for Medicare and Medicaid Innovation (CMMI) must acknowledge that the population who comes through the door post pandemic will be different. “We will have to think about that, and challenge CMS/CMMI to take that into account appropriately,” he said.
CMMI had a brief stakeholders’ meeting on November 4, 2019, to discuss its OCF outline, Patel said, but there has been little information since that time. Oyer said the concerns among practices remain: Physicians worry about improving outcomes, decreasing administrative burden, and maintaining revenue.
“We are also concerned about what our patients are facing, making access available to people across our entire community, [and] providing quality outcomes and patient experience,” Oyer continued. “And then we’re all concerned about our organizations—we work in these organizations.”
With financial stability at the practice level, Oyer said, it’s hard to deliver good care and be a community resource. Doing things the right way depends on having resources to build a good team, he noted, adding, “One of the really good things that came out of OCM for us was that everybody on the team understood their value.”
Like Jordan, Oyer values transparency. “People see a line of sight between what they do in their daily practice and what results they want to accomplish,” he said.
Lyss said achieving buy-in throughout an organization was important for success in the OCM and will be even more so in the OCF. The challenges ahead only become achievable, he said, “through a culture throughout the organization that is committed to value and committed to evolve, adapting to change.”
Practice transformation, said Lyss, “will take time. It’s going to be really hard; there are no shortcuts.”
Alboustani said her payer is working with practices on the data-sharing challenges of the OCM, but that success in shifting to value-based care isn’t just about an individual model—it’s about recognizing that value-based care isn’t going away. “It’s not a phase,” she exclaimed. “It’s probably going to become the norm down the line—and we all have to collaborate. We all have to work better into making this efficient for everyone—for the patient, for the plan, and for the provider.”
As practice transformation evolves, Jordan said the concept of shared savings must do so as well. Practices cannot keep squeezing savings out the practice of oncology—and it’s a reason why some have left the OCM even as they embrace its transformation principles. “The idea that you’re essentially judged against or measured against your own historic performance is, I think, a real problem,” he said. “You should get measured against the market that you’re in. The variability in those markets is significant.”
Jordan said his practice started out in the COME HOME Project, a precursor to OCM, “You’ve already taken a lot of the actions that were necessary to reduce costs. And so your baseline is lower. It completely undercuts your eff orts,” he said. “In terms of where we’re going, I think, we’re probably headed toward capitation. That’s what it looks like, in some form.”
In the end, Alboustani said, “The lesson learned here is: What is the value we’re providing for the member? [And,] what is the value in cost containment for providers through plans?” she asked.
“The key word is collaboration. We all have to own a piece of taking better care of the member, [and] of controlling the rising cost of health care, and I think that’s the only way to succeed.”
The Importance of Examining and Preventing Atrial Fibrillation
August 29th 2023At this year’s American Society for Preventive Cardiology Congress on CVD Prevention, Emelia J. Benjamin, MD, ScM, delivered the Honorary Fellow Award Lecture, “The Imperative to Focus on the Prevention of Atrial Fibrillation,” as the recipient of this year’s Honorary Fellow of the American Society for Preventive Cardiology award.
Listen
Promoting Equity in Public Health: Policy, Investment, and Community Engagement Solutions
June 28th 2022On this episode of Managed Care Cast, we speak with Georges C. Benjamin, MD, executive director of the American Public Health Association, on the core takeaways of his keynote session at AHIP 2022 on public health policy and other solutions to promote equitable health and well-being.
Listen
