- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
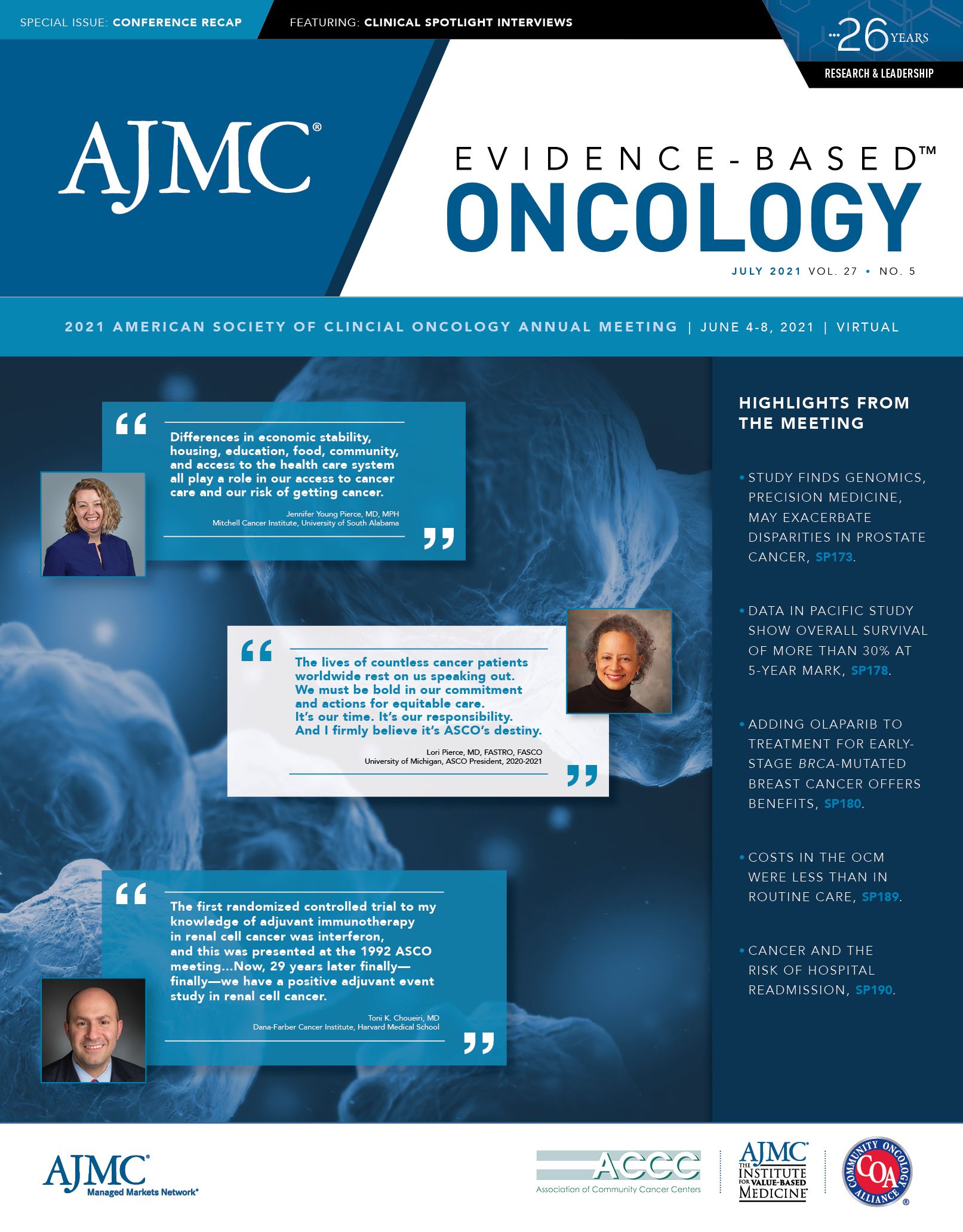
ASCO 2021 Recap: Disparities
Addressing Disparities in Women’s Cancer Care, at Home and Abroad
From Botswana to Bangladesh to Alabama, disparities in care are a worldwide problem for women with gynecological cancers, whether it’s a delay in starting treatment that allows disease to progress, poverty that puts medication out of reach, or what one speaker called the “systemic racism” that keeps Black patients from joining clinical trials.
“Equality in Care for All Women: Addressing Disparities in Gynecologic Malignancies” came on the first day of the 2021 annual meeting of the American Society of Clinical Oncology.
Health equity was a theme throughout the 5-day virtual meeting. This session, moderated by Surbhi Grover, MD, MBA, of the University of Pennsylvania, also featured Arunangshu Das, MBBS, of Square Hospital in Dhaka, Bangladesh, and Jennifer Young Pierce, MD, MPH, of Mitchell Cancer Institute at the University of South Alabama.
Botswana
Grover has developed a practice of global radiation oncology at the Princess Marina Hospital in Gaborone, Botswana. She presented data showing that disparities in care in Africa start with
the limited number of radiotherapy machines in the central part of the continent, which leads to delays treatment for women with locally advanced cervical cancer.
Botswana has high HIV rates: About 20% of adults are HIV positive, with rates among women of reproductive age even higher. Most people know their HIV status and those who are positive are
receiving treatment, noted Grover. “More than 95% of the ones who are on treatment are actually virally suppressed,” she said. But that immunosuppression increases the risk of cervical cancer. If cancer occurs, “These are the patients who will need radiotherapy,” she said. “Overall survival for all patients at 2 years is close to 67%; at 5 years, it’s close to 56%.”
The challenge is getting patients treated in a reasonable time frame. It could take 25 days from a clinic visit to get the pathology report, and by the time the patient gets to the first radiation conference, 40 days have passed. Government-funded care doesn’t mean it’s fast, Grover explained. “During this period, a lot of the patients potentially get lost or get sicker. And that has a huge
impact on their outcomes,” she said.
In 2015, work began on a clinic within Grover’s hospital to set up care navigation to speed the process, connect the various physicians and laboratory staff , and cut down the number of days
from diagnosis to treatment. “Just with this simple intervention, we were able to reduce the [time] from biopsy to treatment from 120 days to 60 days, and we’re reanalyzing these data again, since
this [outcome] was last looked at in 2017,” she said.
Other interventions involve addressing problems with electronic medical records and using phone apps to track patients, which has allowed the hospital to record “every single patient” in an application, which eliminates paper and makes it easier to keep tabs on patients. Ninety percent of patients as well as providers found this “really useful,” said Grover, and patients are permitted to send free messages if they need to reschedule.
Other projects include using technology to figure out why some women do not follow up for radiation for their cervical cancer, to improve screening rates, and to adjust screening guidelines given the needs of patients who come to their clinic.
International Disparities
Das said the “striking disparities” in cancer management between rich and poor countries reach every aspect of care, whether it’s surgery, chemotherapy, radiotherapy, or pathological service.
“Almost 100% of these components are available in the public sector of high-income countries. But if we look at the low-income countries, we can see that only 40% of these essential components
are available [on average] in the public sector,” he said.
Large numbers of patients with gynecological cancers—cervical, endometrial, and ovarian—live in Africa and Asia, Das explained. But the global burden of where deaths occur does not align with
where the resources are.
Each year, Das said, about 207,000 women die of ovarian cancer; 300,000 women die of cervical cancer, and 80% of new cervical cancer diagnoses and deaths happen in Asia and Africa. “There
are 3 important components of cervical cancer management: vaccination, screening, and treatment. Human papillomavirus [HPV] vaccination lowers the risk of cervical cancer in a person.
However, huge disparities persist in the distribution of the HPV vaccine throughout the world,” Das said, pointing to maps and data from the New England Journal of Medicine to show that low- and middle-income countries are not keeping apace.1 Other data show that 19% of eligible women are screened for cervical cancer in low-income countries, compared with 63% of women in high-income countries.
As for treatment, access to the most modern therapies is often limited by price—for example, the cost of bevacizumab, he said, is typically beyond the reach of a wage-earner in a country like
Bangladesh. And technologies like next-generation sequencing, which are essential for today’s precision medicine strategies, may not even be available in some parts of the world, or even to some poor patients in developed countries.
Das noted how the revelation of disparities in care that were made clear during the COVID-19 pandemic had become a political issue. “Collaboration to reduce the gap is needed,” he said. Access to resources and “the commitment of international societies and organizations is needed to ensure equality.”
Disparities at Home
Pierce was direct in taking on the “paradox of ongoing disparities and emerging technology,” showing a map of the United States to highlight how cervical cancer rates vary by state and by population. “Specifically, by race, we see higher rates of mortality in Black, Hispanic, and Native
American women,” she said, noting, however, that disparities have decreased and access to guideline-based care has improved.
Still, “race is not the only category in which we see ongoing disparities. In each state, there are a
multitude of differences that each county within a state can have,” she said. Using maps from Alabama, she showed the overlap of HPV-associated cancer incidence and poverty.
“We know that in the United States, race is just a marker for other social determinants of health due
to systemic racism. And yet this can be true in other parts of the world as well,” Pierce said. "Differences in economic stability, housing, education, food, community, and access to the health care system all play a role in our access to cancer care and our risk of getting cancer.”
Pierce addressed several realities of vaccination:
• Rates of HPV vaccination range from 39% to 60%, and Pierce said uptake can be affected
by cultural concerns that vaccination of young adolescents is akin to an invitation to engage in premarital sex.
• In Alabama, those with public insurance are more likely to get the HPV vaccine than those with private coverage.
Guidelines that call for HPV screening and testing, along with Pap screening, and take into account a patient’s history and near- and long-term risk, may help. Such factors “ultimately result in a recommendation that is specific to that patient on that day,” Pierce said, but they may not be helpful in other countries.
Social determinants play a role in many aspects of health care, ranging from lack of transportation to reach facilities and not having child care (leading to missed appointments) to not being enrolled in clinical trials. “It’s important to note that differences in screening do account for differences in mortality: Up to 50% of women dying of cervical cancer [did not have] recent screening. However, these [differences] do not account for the disparities,” Pierce said.
Why, Pierce asked, are women of different races with cervical cancer at the same stage often given
different surgical recommendations? It’s a big problem if patients are receiving guideline-based
care and yet even in a high-volume hospital the disparities are not completely eliminated, she said.
“Genetic alterations may contribute to these disparities, and increasingly, data support molecular
differences at the tumor level by race and other cancers,” Pierce said. “These genetic differences may play a role in the treatments that we are offering patients and their response to treatment,”
Pierce said.
The problem: White women account for most of the patients in the studies used to develop the guidelines.
For women of other races, “if we want to find different treatments that may work differently, we’ve
got to look harder,” she said.
Reference
1. Lei J, Ploner A, Elfström KM, et al. HPV vaccination and the risk of invasive
cervical cancer. N Engl J Med. 2020;383(14):1340-1348. doi:10.1056/1. NEJMoa1917338
Study Finds Genomics, Precision Medicine May Exacerbate Racial Disparities in Prostate Cancer
Racial disparities in health outcomes, including in cancer, are well documented. However, it’s not always clear how biological or socioeconomic factors affect these disparities, or whether advances in genomics and precision medicine have an impact.
Now, new research presented at the 2021 American Society of Clinical Oncology Annual Meeting is painting a clearer picture of what drives differences in mortality and outcomes for patients with prostate cancer, which has higher incidence and mortality among Black men.
The lifetime probability of developing prostate cancer is 18.2% among Black men compared with 13.3% among White men. Black men are also significantly more likely to die of prostate cancer than White men (4.4% vs 2.4%).1
Although the advances in genomics and precision medicine promise to improve risk prediction and outcomes for many cancers, they may also actually exacerbate these disparities. In a study presented as an abstract by Foundation Medicine and collaborators, Brandon Mahal, MD, assistant professor of radiation oncology and assistant director of community outreach and engagement at the Sylvester Comprehensive Cancer Center, and colleagues looked at how patterns of comprehensive genomic profiling and treatment varied by race.2
The data, coming from the largest known cohort of its kind, revealed that despite having similar frequency of actionable gene alterations, men of African descent were less likely than men of European ancestry to receive early comprehensive genomic profiling and to be enrolled in clinical trials.
The researchers collected data on more than 11,000 patients with advanced prostate cancer with comprehensive genomic profiling, including 1400 men of African descent and 9200 patients of European descent. They also analyzed real-world data from nearly 900 patients from Foundation Medicine and Flatiron Health’s clinic-genomic database.
The rates of alterations in BRCA1/2, AR, DNA damage response pathway genes, and actionable genes were similar across the 2 ancestry types. And while both groups were just as likely to receive
immunotherapy and PARP inhibitor treatment, men of African descent were nearly 3 times less likely to receive an investigational treatment in a clinical trial compared with men of European
descent (11% vs 30%). This remained true even among men with actionable alterations (1% vs 6%).
“Men of African ancestry experience the greatest burden of disease in prostate cancer, and this research indicates that differences in cancer care are not solely based on biological factors, but
rather points to socioeconomic factors such as access to comprehensive genomic profiling and clinical trial enrollment,” Mahal said in a statement.3 “To ensure equitable opportunities for precision medicine, we need to expand access to and awareness of advances that impact patient care and outcomes, including timely use of genomic testing to help make informed treatment decisions.”
During a separate presentation, Mahal explained that most genomic studies are based on Eurocentric cohorts, with approximately 80% of patients included in the genome-wide association study being of European descent despite accounting for 16% of the population, leaving the door open to worsening disparities due to a lack of representative studies.4
Mahal outlined several approaches that could be taken to both study and address disparities in
prostate cancer, including: transdisciplinary research that bridges basic, clinical, and epidemiological research; trials that include diverse populations; precision medicine used as a means to identify mechanisms of disparity; and outreach programs to bring care delivery and
cutting-edge science to diverse communities.
References
1. Cancer facts & figures for African Americans 2016-2018. American Cancer Society website. Accessed June 18, 2021. https://www.cancer. org/research/cancer-facts-statistics/cancer-facts-figures-for-africanamericans.html
2. Sivakumar S, Kim Lee J, Moore JA, et al. Ancestral characterization of the genomic landscape, comprehensive genomic profiling utilization, and treatment patterns may inform disparities in prostate cancer: a largescale analysis. J Clin Oncol. 2021;39(Suppl 15):abstr 5003. doi:10.1200/
JCO.2021.39.15_suppl.5003
3. New study results presented by Foundation Medicine and collaborators at ASCO21 on ancestry-based disparities in prostate cancer care underscore importance of equitable access to precision medicine advances. News release. Foundation Medicine; June 4, 2021. Accessed June 6, 2021. https://www.foundationmedicine.com/press-releases/aa904bd1-4854-44e9-8d03-24b5af5ff392
4. Martin AR, Kanai M, Kamatani Y, Okada Y, Neale BM, Daly MJ. Clinical use of current polygenic risk scores may exacerbate health disparities. Nat Gen. 2019;51(4):584-591. doi:10.1038/s41588-019-0379-x. Published correction appears in Nat Gen. 2021;53(5):763.
Community-Based Initiative Doubles Accrual Rate of Black Participants in Cancer Trials
A 5-year initiative to encourage the enrollment of Black participants in cancer clinical trials was associated with improved accrual rates at the Abramson Cancer Center (ACC) at the University of Pennsylvania, according to research results published during the 2021 annual meeting of the American Society of Clinical Oncology.
Using targeted community outreach and engagement strategies, the effort aimed to address the broader issue of underrepresentation of Black participants in cancer research—nationwide, only 5% of Black patients are enrolled in clinical trials, although Black individuals comprise about 14% of the overall US population.
In 2014, baseline findings of the 12-county catchment area near Philadelphia showed that while Black residents comprised 19.0% of the population and 16.5% of patients with cancer, only 11% of ACC patients were Black. The rates of enrollment of Black participants in 3 kinds of trials—treatment, nontherapeutic interventional, and noninterventional—were 12.2%, 8.3%, and 13.0%, respectively.
The ACC launched the community-based engagement initiative to address these gaps. The program implemented culturally tailored marketing strategies for cancer clinical trials; protocol-specific plans to facilitate Black participant enrollment; new partnerships with faith-based organizations serving Black communities to conduct educational events about clinical trials; and pilot programs with Lyft and Ride Health to address transportation barriers. It also promoted patient education by nurse navigators regarding cancer and clinical trials and established an improved informed consent process.
Using formats ranging from educational forums to wellness fairs, the program reached more than 10,000 individuals in venues such as churches, neighborhood community centers and parks, and health centers.
By 2018, the outreach was bearing fruit, with the percentage of Black patients treated at the ACC increasing to 16.2%, an approximate 5% increase over 2014. It matched the percentage of Black cancer patients in the areas around the hospital.
Other findings showed:
• The number of Black participants enrolled in cancer clinical trials at ACC rose to 13,170, up 41.5% from 2014.
• There was a 1.7- to 4.0-fold increase in enrollment rates in the 3 types of clinical trials, with accrual rates in treatment, nontherapeutic interventional, and noninterventional trials at 23.9%, 33.1%, and 22.5%, respectively.
The results of the program suggest that gaps in accessibility to cancer centers exacerbate issues of underrepresentation of the Black community in cancer research, said the authors, who noted that further research should take into account the effect of Medicaid expansion, which was happening during the 5 years of the study in the states served by the ACC (Pennsylvania, New Jersey, and Delaware).
“Aligning the number of Black patients with cancer we care for with the number enrolled in our trials is how we can help bring more equitable care in the community, close gaps in disparities,
and sustain trust,” said senior author Robert H. Vonderheide, MD, DPhil, director of the ACC and vice president for cancer programs in the University of Pennsylvania Health System, in a statement.
“There’s more work to be done to improve access and inclusion of minority groups, and the impact of this outreach and engagement effort is an important step forward.”
Reference
Guerra CE, Sallee V, Hwang W-T, et al. Accrual of Black participants to cancer clinical trials
following a five-year prospective initiative of community outreach and engagement. J Clin
Oncol 2021;39(Suppl 15):abstr 100. doi:10.1200/JCO.2021.39.15_suppl.100