- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Real-World Evidence Backs Acalabrutinib in CLL Care
Real-world ONCare data show acalabrutinib lowers new-onset HTN, CV events, and discontinuations vs ibrutinib in R/R CLL/SLL.
For patients receiving treatment for relapsed/refractory chronic lymphocytic leukemia (R/R CLL) or small lymphocytic leukemia, experts recommend that oncologists administer acalabrutinib in the community setting instead of ibrutinib,1 although both are known as effective Bruton tyrosine kinase (BTK) inhibitors. In a new retrospective comparative study of patients treated with either acalabrutinib (n = 90) or ibrutinib (n = 180) over 7 years (January 1, 2017, through December 31, 2023), hypertension (HTN) and other cardiovascular medical events of interest (CV MEOIs) more often resulted from ibrutinib than acalabrutinib.
This study was recently published in the Journal of Medical Economics, using data from the ONCare Alliance Network, and the patients included had a prior treatment history of at least 1 line of acalabrutinib or ibrutinib monotherapy at a community practice in the US. The primary end point was development of new-onset HTN or exacerbation of existing HTN, and the key secondary end point was development of an MEOI from the start of BTK inhibitor therapy. The overall median follow-up time was 33 months: 26 months for those who received acalabrutinib and 42 months for those who received ibrutinib.
“A recent review of the literature suggested that the impact of CV MEOI on health care resource use (HCRU) in a real-world R/R CLL/SLL setting has not been evaluated,” the authors wrote when explaining their motivation for this analysis.
Baseline characteristics showed the acalabrutinib cohort to be older (median [IQR] age, 74.5 [54-89] vs 70.0 [47-88] years), comprised of fewer Black and “other” race patients (6.6% vs 12.2%), have a higher rate of Eastern Cooperative Oncology Group Performance Status of 0 or 1 (82.2% vs 68.9%), have lower median (IQR) systolic and diastolic blood pressures at therapy start (124 [102-161] and 72 [50-89] mm Hg vs 130 [99-184] and 74 [55-99] mm Hg), and have higher rates of most clinical comorbidities in the year leading up to the study:
- Atrial fibrillation: 14.4% vs 10.6%
- Congestive heart failure: 4.4% vs 3.3%
- Hypertension: 56.7% vs 58.3%
- Valvular heart disease: 5.6% vs 1.7%
- Clinically significant bleeding events: 2.2% vs 0.6%
- Venous thromboembolic events: 3.3% vs 0.6%
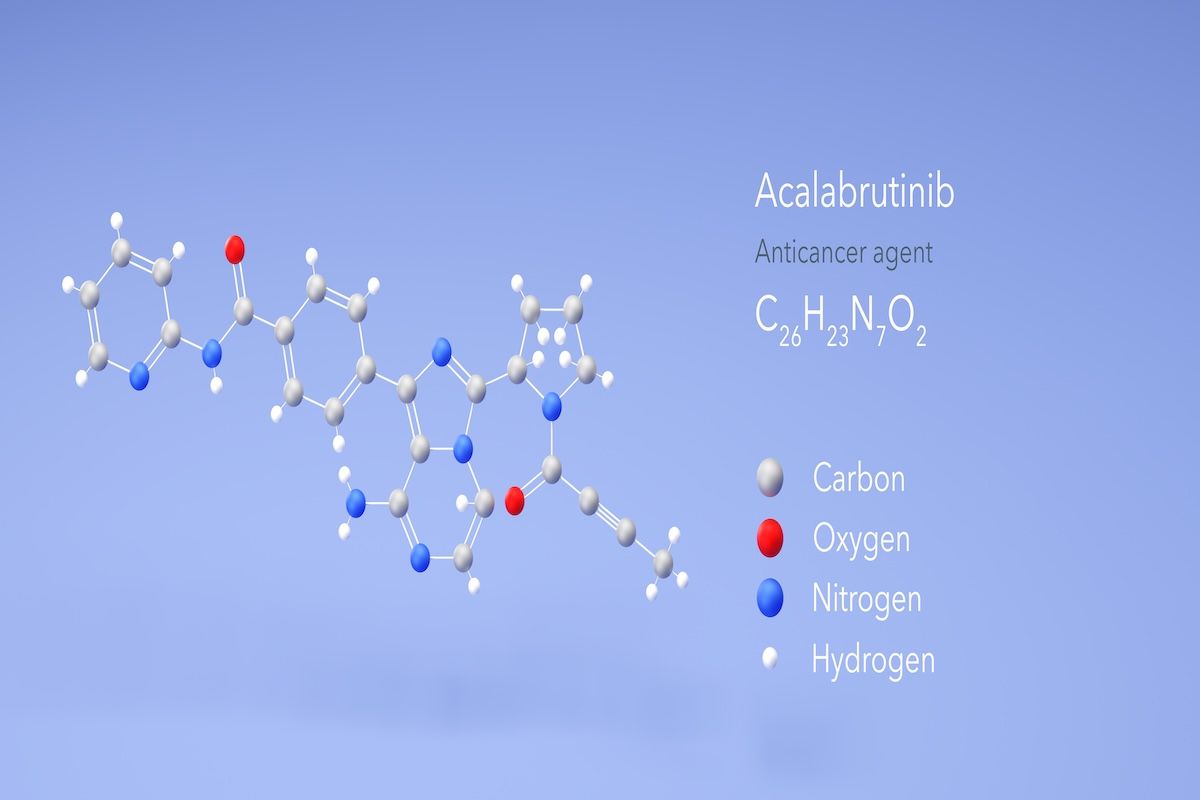
Previous research shows that acalabrutinib has been associated with a better safety profile vs ibrutinib and that although ibrutinib remains a recommended therapy for CLL/SLL, it is no longer considered “the BTK inhibitor of choice” due to associated toxicities. | Image Credit: © Сергей Шиманович-stocka.dobe.com.jpeg
Overall, at the median follow-up of 33 months among the patients who received acalabrutinib, there were far fewer cases of hypertension (OR, 0.27; 95% CI, 0.074-0.98; P = .046) and treatment discontinuation resulting from adverse events (OR, 0.39; 95% CI, 0.20-0.73; P = .002) vs the patients who received ibrutinib.
The patients who received acalabrutinib also had a lower rate of hospital admission for CV MEOI (0.20 vs 0.24 per patient), hospital stays that were half the length of the ibrutinib group (3 vs 6 days), fewer specialist consults (0.11 vs 0.22 per patient), and fewer associated medical procedures (0.11 vs 0.18 per patient).
Additional results show ibrutinib to potentially be inferior as a monotherapy, with a greater proportion of this cohort requiring dose decreases compared with the acalabrutinib group (31.1% vs 22.2%). The risk for treatment discontinuation was also significantly higher among the patients who received ibrutinib because of CV MEOI and other adverse events (OR, 2.54; 95% CI, 1.36-4.91). There were 3.4 times as many total hospital days in the ibrutinib cohort vs the acalabrutinib cohort: 266 vs 77 days.
Previous research shows that acalabrutinib has been associated with a better safety profile vs ibrutinib2,3 and that although ibrutinib remains a recommended therapy for CLL/SLL, it is no longer considered “the BTK inhibitor of choice” due to associated toxicities.4-6 To this, the authors add that real-world data support the use of newer-generation therapies, of which acalabrutinib is one.
“Given these findings,” the authors concluded, “acalabrutinib should be the preferred alternative to ibrutinib because of its superior tolerability and its potential to minimize future health care costs.”
Limitations on these findings are the observational nature of the data, which may have led to an imbalance in the baseline patients and disease characteristics; the long follow-up could have caused data points to be missed; and performing multiple comparative tests could have resulted in Type 1 statistical errors.
References
- Dranitsaris G, Peevyhouse A, Neuhalfen H, et al. A real-world study evaluating drug tolerability and health care resource use with acalabrutinib vs ibrutinib in patients with relapsed/refractory chronic lymphocytic leukemia/small lymphocytic lymphoma. J Med Econ. 2026;29(1):30-40. doi:10.1080/13696998.2025.2604971
- Byrd JC, Hillmen P, Ghia P, et al. Acalabrutinib versus ibrutinib in previously treated chronic lymphocytic leukemia: results of the first randomized phase III trial. J Clin Oncol. 2021;39(31):3441-3452. doi:10.1200/JCO.21.01210
- Seymour JF, Byrd JC, Ghia P, et al. Detailed safety profile of acalabrutinib vs ibrutinib in previously treated chronic lymphocytic leukemia in the ELEVATE-RR trial. Blood. 2023;142(8):687-699. doi:10.1182/blood.2022018818
- Stephens D. NCCN guidelines update: chronic lymphocytic leukemia/small lymphocytic lymphoma. J Natl Compr Canc Netw. 2023;21(5.5):563-566. doi:10.6004/jnccn.2023.5007
- Dong R, Yan Y, Zeng X, Lin N, Tan B. Ibrutinib-associated cardiotoxicity: from the pharmaceutical to the clinical. Drug Des Devel Ther. 2022;16:3225-3239. doi:10.2147/DDDT.S377697
- Christensen BW, Zaha VG, Awan FT. Cardiotoxicity of BTK inhibitors: ibrutinib and beyond. Expert Rev Hematol. 2022;15(4):321-331. doi:10.1080/17474086.2022.2067526
Quality of Life: The Pending Outcome in Idiopathic Pulmonary Fibrosis
February 6th 2026Because evidence gaps in idiopathic pulmonary fibrosis research hinder demonstration of antifibrotic therapies’ impact on patient quality of life (QOL), integrating validated health-related QOL measures into trials is urgently needed.
Read More
