- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
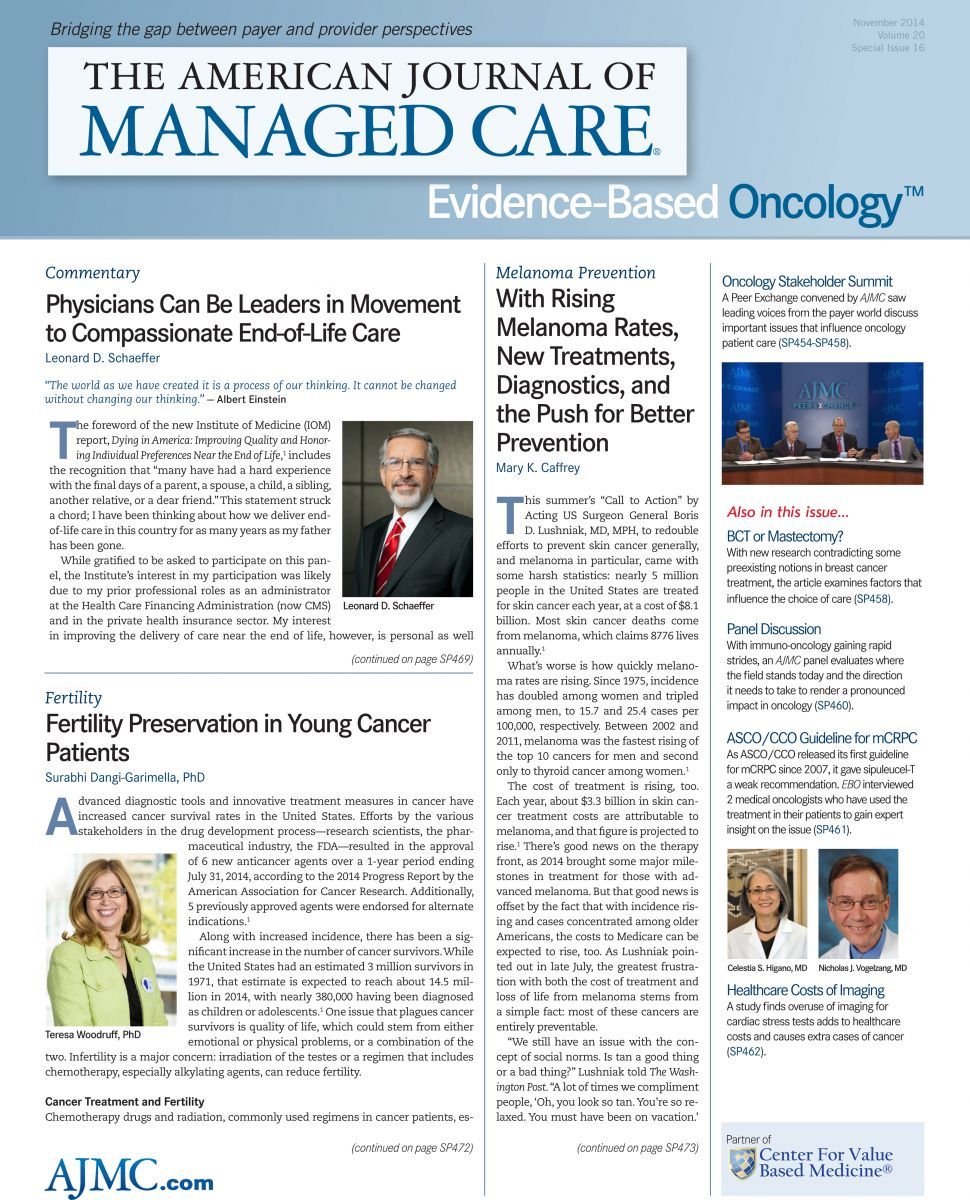
With Rising Melanoma Rates, New Treatments, Diagnostics, and the Push for Better Prevention
This summer’s “Call to Action” by Acting US Surgeon General Boris D. Lushniak, MD, MPH, to redouble efforts to prevent skin cancer generally, and melanoma in particular, came with some harsh statistics: nearly 5 million people in the United States are treated for skin cancer each year, at a cost of $8.1 billion. Most skin cancer deaths come from melanoma, which claims 8776 lives annually.1
What’s worse is how quickly melanoma rates are rising. Since 1975, incidence has doubled among women and tripled among men, to 15.7 and 25.4 cases per 100,000, respectively. Between 2002 and 2011, melanoma was the fastest rising of the top 10 cancers for men and second only to thyroid cancer among women.1 The cost of treatment is rising, too. Each year, about $3.3 billion in skin cancer treatment costs are attributable to melanoma, and that figure is projected to rise.1 There’s good news on the therapy front, as 2014 brought some major milestones in treatment for those with advanced melanoma. But that good news is offset by the fact that with incidence rising and cases concentrated among older Americans, the costs to Medicare can be expected to rise, too. As Lushniak pointed out in late July, the greatest frustration with both the cost of treatment and loss of life from melanoma stems from a simple fact: most of these cancers are entirely preventable.
“We still have an issue with the concept of social norms. Is tan a good thing or a bad thing?” Lushniak told The Washington Post. “A lot of times we compliment people, ‘Oh, you look so tan. You’re so relaxed. You must have been on vacation.’
Part of the thing we really want to emphasize in this call to action is that tanned skin is damaged skin.”2
Lushniak’s alarm had not been shared across federal landscape, at least until recently. Even within the FDA, there is a dichotomy. Within the FDA’s Center for Drug Evaluation and Research (CDER), the office that approves new cancer therapies has moved with great speed in recent years, approving 6 new melanoma therapies since 2011.3,4 But a different section of CDER that approves new ingredients for sunscreen has moved so slowly that it took a bill backed by the Melanoma Research Foundation (MRF) to finally stir activity on the prevention side.
The FDA finally began to act on a 12-year backlog of approvals for new sunscreen ingredients when legislation backed by the MRF, the Sunscreen Innovation Act, began to move through the Congress.5 The bill has passed both the US House of Representatives and the Senate, and final adoption could come after midterm elections.
According to Timothy Turnham, PhD, executive director of the MRF, rising melanoma rates demand equal attention to treatment and to prevention measures, including strategies to trim the use of tanning salons by teenagers and young adults. “What both the call to action and the legislation show is the growing awareness of the healthcare crisis that is melanoma,” he told Evidence-Based Oncology.
Advances in Treatment
Trametinib and dabrafenib. On January 10, 2014, the FDA approved the use of trametinib (Mekinist) and dabrafenib (Tafinlar) in combination to treat unresectable or metastatic melanoma. Both drugs had been approved as monotherapy in May 2013,3 but the January action confirmed what leaders of clinical trials had discussed with EBO that previous summer: for some patients, the combination of the 2 drugs produces a more durable response than either drug alone.6
In granting approval for the combination, the FDA cited trial results that found 76% of patients treated with the combination had their cancer shrink, and the response lasted an average of 10.5 months. Among patients treated with dabrafenib as a single agent, 56% had an objective response that lasted an average of 5.6 months. However, this study involved only patients who had not received prior therapy.3
The Journal of Clinical Oncology reported results October 6, 2014, from a study of patients who received the combination following disease progression prior to treatment.7 The phase 1/2 open-label study included 26 patients who received the combination therapy after previous treatment with a BRAF inhibitor (known as group B). Another 45 patients who had received prior treatment with dabrafenib were eligible for combination therapy at the time of tumor progression (known as group C).
Overall response rates were 15% for patients in group B and 13% for patients in group C, with 50% of the patients in group B and 44% in group C experiencing stable disease for at least 8 weeks. For those in group C, progression-free survival (PFS) was 3.6 months and median overall survival was 11.8 months. Those who had been treated with dabrafenib alone for at least 6 months had better outcomes than those who had been treated with dabrafenib alone for less than 6 months, due to rapid disease progression. Median PFS was 3.9 months, and compared with 1.8 months. The researchers concluded that the drug combination could offer modest benefits to some patients with prior treatment, but not to those whose disease progressed very rapidly.7
Vemurafenib and cobimetinib. FDA approved vemurafenib in 2011 as one of the earliest therapies aimed at inhibiting the BRAF mutation that signals melanoma cells to proliferate. New results reported in September in the New England Journal of Medicine show that the therapy may be even more effective in combination with cobimetinib.8 Researchers sought to resolve a quandary among patients treated with vemurafenib: about 25% developed a second cancer.9 A randomized clinical trial of 495 patients found that median PFS was 9.9 months in the combination group and 6.2 months in the control group that received vemurafenib and placebo.
The rate of complete or partial response in the combination group was 68%, compared with 45% in the control group, while rates of complete response were 10% in the combination group and 4% in the control group.8 According to a statement from UCLA’s Jonsson Cancer Center, where a part of the research was conducted, the next step will be to seek FDA approval for the combination.9
Pembrolizumab. On September 4, 2014, the FDA approved pembrolizumab, the first PD-1 inhibitor to be approved; the PD-1 protein prevents the immune system from attacking melanoma cells. This therapy, marketed as Keytruda by Merck & Co, is designed for patients with end-stage melanoma and intended to be used in combination with ipilimumab in patients who have previously been treated with ipilimumab and a BRAF inhibitor.4 Pembrolizumab had been given breakthrough status last year, a designation given to drugs when preclinical evidence shows they will offer a substantial improvement over available therapies. The trametinib-dabrafenib combination also went through an accelerated approval process.3,4
According to Turnham, the wave of new melanoma therapies shows the “nimble approach” that Richard Pazdur, MD, has pursed as director of the Office of Hematology and Oncology Products within CDER. The rapid movement of many drugs “from bench to approval” has saved lives, said Turnham, who added that he was not sure why this mind-set did not permeate other parts of the agency, including those that deal with over-the-counter products.
Potential in Diagnostics
As drugs are increasingly used in combination or in sequence, treatment prices can rise steeply. The wave of new treatments for advanced melanoma has raised concerns about cost; including administrative expenditures, 1 cycle of ipilimumab costs nearly $31,000.10 Concerns include making sure that therapies go only to those patients who need them, and that treatment starts as soon as possible before the disease progresses. These prohibitive prices have created interest in better diagnostic tools.
In September, Myriad Genetics, Inc, announced results of a clinical utility study presented at the College of American Pathology meeting in Chicago, Illinois. The study presented data involving 687 cases of pigmented skin lesions that were submitted by 42 dermatopathologists, who were asked to document a diagnosis and treatment strategy both before and after analyzing the lesions with the myPath melanoma test score.11 According to Loren Clarke, MD, vice president of medical affairs at Myriad Genetics, Inc, the myPath score caused the dermatopathologists to revise treatment recommendations in 35% of the cases, and testing led to a 76% reduction in “indeterminate” diagnoses—cases in which the dermatologist would otherwise have to wait and watch a suspicious mole before making a decision to treat.11 At press time, the results had not yet been published in a peer-reviewed journal.
Clarke said the diagnostic tool shows promise, especially in cases of “indeterminate” results, which he said represent at least one-third of cases, when cancers are biopsied before they have developed defining characteristics. “The test is designed for exactly that situation,” he said in an interview with EBO. The myPath test would allow physicians to treat only those cases that are definitely cancer and avoid overtreatment of pigmented marks that pose no danger, Clarke told EBO.
Better Sunscreen, Better Prevention
The Sunscreen Innovation Act came about after MRF exhausted other options in trying to prod the FDA to address the 12-year backlog of pending applications for new sunscreen ingredients. Turnham said improved sunscreens could offer better protection against harmful ultraviolet rays that cause at least 80% of all melanoma cases.
The group is also pursuing stronger regulations on indoor tanning beds. At present, they are considered Class 1 medical devices; the MRF believes they should be moved to Class 2, at a minimum. Turnham said draft regulations to allow this change have been pending at the FDA for more than a year.
Other strategies could include expanding taxes on tanning beds, since this measure has been shown to curb tobacco use among teens and young adults, Turnham said. He has started talking to payers about creating financial incentives in healthcare to discourage indoor tanning, especially among young women. The “Call to Action” report and other data have shown what Turnham called a “bubble” of melanoma cases among young women in their late 20s, while cases among men tend to peak when they are in their 50s and 60s.1
It’s impossible to say how quickly melanoma rates would fall once consumers have better sunscreens, Turnham said, but “with better ingredients, and better options it will have a positive impact.”
References
1. The Surgeon General’s Call to Action to Prevent Skin Cancer. http://www.surgeongeneral.gov.www.surgeongeneral.gov/library/calls/prevent-skin-cancer/call-to-action-prevent-skin-cancer.pdf. Washington, DC: HHS, Office of the Surgeon General; 2014.
2. Dennis B. Why acting surgeon general thinks skin cancer is a major public health problem. The Washington Post. http://www.washingtonpost.com/news/to-your-health/wp/2014/07/29/why-theacting-surgeon-general-thinks-skin-cancer-is-a-majorpublic-health-problem/. Published July 29, 2014. Accessed October 21, 2014.
3. FDA approves Mekinist in combination with Taflinar for advanced melanoma [press release]. Silver Spring, MD: FDA Newsroom; January 10, 2014.http://www.fda.gov/newsevents/newsroom/pressannouncements/ucm381159.htm.
4. FDA approves Keytruda for advanced melanoma [press release]. Silver Spring, MD: FDA Newsroom; September 4, 2014. http://www.fda.gov/newsevents/newsroom/pressannouncements/ucm412802.htm.
5. Hackman M. House passes bill to speed FDA sunscreen approvals. The Wall Street Journal. http://online.wsj.com/articles/house-passes-bill-to-speedfdas-sunscreen-approvals-1406585979. Published July 28, 2014. Accessed October 20, 2014.
6. Beagin N. Melanoma: from impossible to treat to poster child for targeted therapies. Am J Manag Care. 2013;19(SP9)SP280-SP285.
7. Johnson DB, Flaherty KT, Weber JS, et al. Combined BRAF (dabrafenib) and MEK inhibition (trametinib) in patients with BRAFV600-mutant melanoma experiencing progression with single-agent BRAF inhibitor [published online October 6, 2014]. J Clin Onc. doi:10.1200/JCO.2014.57.3535.
8. Larkin J, Ascierto PA, Dreno B, et al. Combined vemurafenib and cobimetinib in BRAF-mutated melanoma [published online September 29, 2014]. N Engl J Med. doi:10.1056/NEJMoa1408868.
9. Kulmar R. New melanoma drug therapy improves survival rate while lowering chances of side effects [press release]. Los Angeles, CA: UCLA Newsroom; October 6, 2014. http://newsroom.ucla.edu/ releases/new-melanoma-drug-therapy-improvessurvival-rate-while-lowering-chances-of-side-effects.
10. The economic value of ipilimumab as a secondline treatment in patients with advanced melanoma. OncLive website. http://www.onclive.com/publications/obtn/2013/March-2013/The-Economic-Value-of-Ipilimumab-as-a-Second-Line-Treatment-in-Patients-With-Advanced-Melanoma. Published April 3, 2013. Accessed October 22, 2014.
11. Myriad myPath melanoma test reduced indeterminate cases by 76% and changed treatment in 35% of cases [press release]. Salt Lake City, UT: Myriad Genetics; September 9, 2014. http://investor.myriad.com/releasedetail.cfm?releaseid=869792.
12. Senate unanimously approves Sunscreen Innovation Act [press release]. Washington, DC: Melanoma Research Foundation; September 17, 2014. http://www.melanoma.org/about-us/news-press-room/press-releases/senate-unanimously-approvessunscreen-innovation-act.
Empowering Children and Parents Through Technology: Opportunities, Challenges, and Future Directions
January 15th 2026Digital health platforms improve pediatric care by offering customized, interactive tools for children and parents. They enhance education, support, and engagement while tackling challenges related to access, usability, and privacy.
Read More
Insights Into Patient Portal Engagement Leveraging Observational Electronic Health Data
January 12th 2026This analysis of more than 250,000 adults at least 50 years old with chronic conditions showed lower portal use among older, non–English-speaking, and Black patients, underscoring digital health equity gaps.
Read More
Subjective and Objective Impacts of Ambulatory AI Scribes
January 8th 2026Although the vast majority of physicians using an artificial intelligence (AI) scribe perceived a reduction in documentation time, those with the most actual time savings had higher relative baseline levels of documentation time.
Read More
Telehealth Intervention by Pharmacists Collaboratively Enhances Hypertension Management and Outcomes
January 7th 2026Patient interaction and enhanced support with clinical pharmacists significantly improved pass rates for a measure of controlling blood pressure compared with usual care.
Read More

