- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
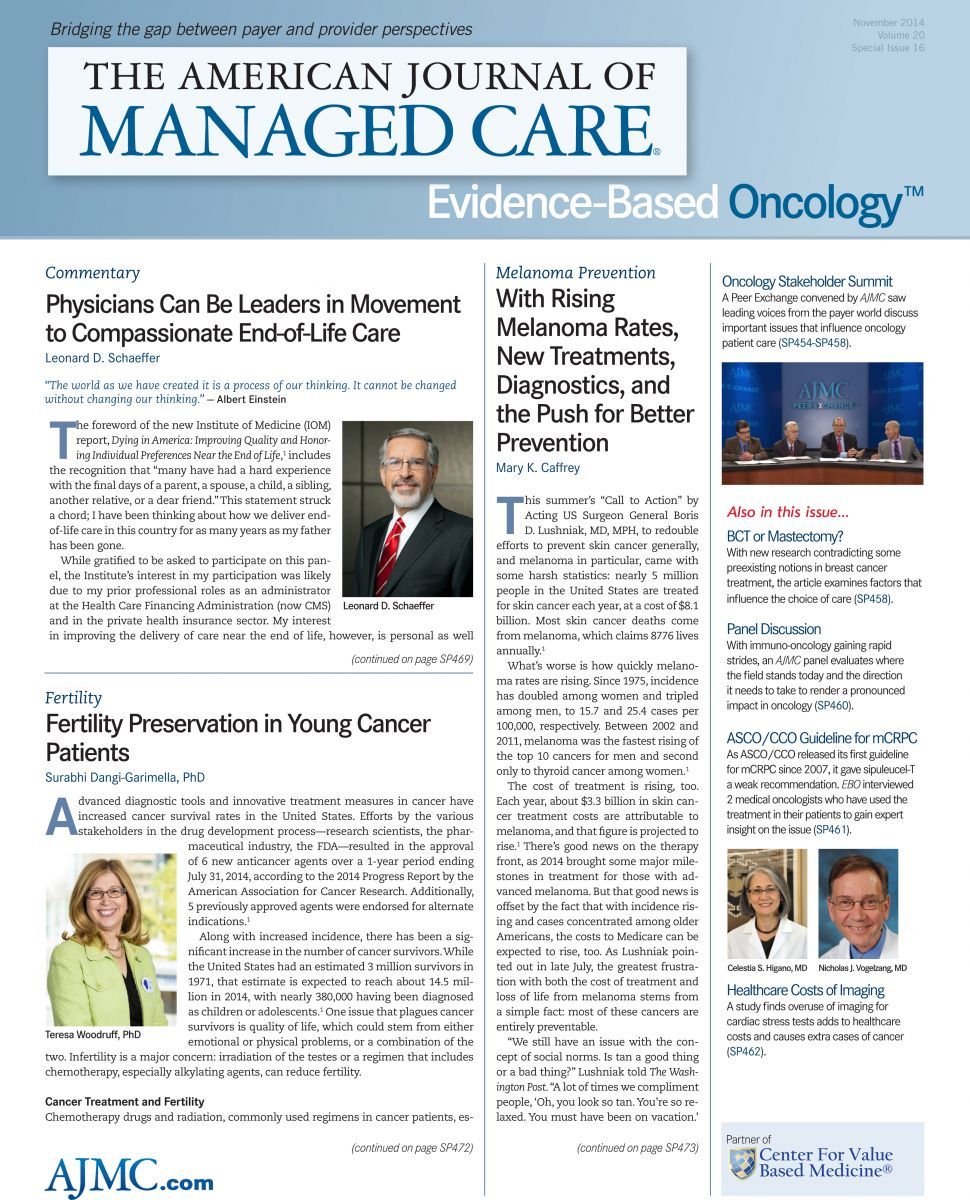
AJMC Panel Explores Immuno-oncology, and What Making Cancer a Chronic Condition Means for Payers
The emergence of immuno-oncology, in which a patient’s own immune system is activated to fight the cancer, has shown promise in certain tumor subtypes, notably with therapies such as ipilimumab, which has been approved for metastatic melanoma.
But immuno-oncology presents certain challenges. Patients may not be “cured” in the conventional sense; rather, the disease may be converted to a chronic condition. In some cases the person can return to work, but in others, that’s not possible. This raises important policy choices when employers pay for healthcare.
Surabhi Dangi-Garimella, PhD, managing editor of Evidence-Based Oncology, served as moderator of the panel, which featured Michael Kolodziej, MD, medical oncologist and national medical director for Oncology Strategies at Aetna; Kimberly Shafer-Weaver, PhD, tumor immunologist and program director for immunology, oncology, and metabolic disease at Health Analytics; and Jianda Yuan, MD, assistant lab member at the Immune Monitoring Core, Memorial Sloan Kettering Cancer Center.
The discussion involved checkpoint inhibitors on the market and those under development, including the CTLA-4, PD-1, and PD-L1 inhibitors.
Matching the Therapy to the Patient
Dangi-Garimella asked the panelists whether there are good biomarkers to help clinicians match a patient to a specific drug and to measure patient response to treatment.
This issue is important to payers, Kolodziej explained. In his view, cost is not the first thing payers examine; instead, it’s the evidence of whether a therapy works and for whom it works. If the evidence supports using the therapy in a particular patient, payers then look into how to fund it.
As Schafer-Weaver discussed, the field is challenged by the lack of consistency in testing for how well some immunotherapies will work in a given patient. But both she and Yuan said this is changing. Yuan added that technology is helping to make things more cost-effective. “It would be ideal to find good markers (that) could predict the patient’s initial response to the immunotherapies,” he said, which would improve clinical response.
To ensure matching the therapy to the patient requires better education of physicians, at conferences and through other means. But there is still a knowledge gap between the leading researchers in the field and the treating physicians. “I cannot tell you the number of people, (with questions) from their families or from their friends who get diagnosed with cancer, who call me up and ask me, ‘What should I be asking?’ And it is amazing that, right now, standard of care is not immunotherapy,” she said.
Researchers are quickly learning that immunotherapy should happen sooner rather than later, she said, “when the patient has a good ability to respond because their immune system is intact.”
The Right Amount of Therapy
Kolodziej said that today, approval from the FDA, along with appearance on the guidelines of the National Comprehensive Cancer Network, typically guides commercial payers. That said, immunotherapies are very expensive. “Because of the high cost, there is a lot of scrutiny in managed care to make sure that the right patient gets the treatment,” he said.
Development of better biomarkers is encouraging, Kolodziej said, because when therapies can be better matched to patients who will see a response, everyone benefits. All this will become increasingly important to payers as decisions are made about how to sequence different therapies, or whether to use them in combination.
“There is a great deal of desperation in patients with advanced malignancy,” he said, speaking from years of experience. “In the era when we did not have anything that worked, we wanted to try everything. Those days are over.”
How Do We Measure Benefits?
Dangi-Garimella asked how heavily patient-reported outcomes should be weighed in deciding the value of immunotherapy. This raised another issue: who should pay for these therapies?
Kolodziej said more is being done to include patient-reported outcomes, but the approach is in its “infancy.” Shafer-Weaver agreed and said that “quality of life” is defined differently by different people. One question that will arise is whether a patient’s employer should continue to pay for therapy if the cancer has become a chronic condition but there is no possibility the person will return to work.
The old way of measuring response—reduced tumor size on a scan—may no longer apply. “We are looking at a progression-free, stable disease as almost a win,” Shafer-Weaver said.
Kolodziej agreed that different measures of clinical benefit, which he called “nontraditional end points,” will apply when assessing the success of immunotherapy in the future. Doing this will require better post marketing data collection than the field has seen to date. “I think the track records for post approval, post marketing collection of that data is extremely poor,” he said. “And there is a good reason for it; it is difficult, it is expensive, and it does not impact selling the product.”
Better Data Collection
As drug options for formulary managers increase, more data will be needed. If, for example, there are up to 4 different PD-1 or PD-L1 therapies from which to choose, pharmaceutical companies will have to perform studies to allow different treatments to distinguish themselves. This will be a good thing, Kolodziej said, as it will require better reporting of patient outcomes than has been done to date.
EBO
“If we could find a way to collect those data and tie them to other more traditional end points, that would be a great service,” he said. “And it would help us understand perhaps what the optimal utilization of these agents should be.”
To hear the full discussion, please visit: http://www.ajmc.com/ajmc-tv/panel-discussion/immuno-oncology-brings-forth-promises-and-challenges.
Ambient AI Tool Adoption in US Hospitals and Associated Factors
January 27th 2026Nearly two-thirds of hospitals using Epic have adopted ambient artificial intelligence (AI), with higher uptake among larger, not-for-profit hospitals and those with higher workload and stronger financial performance.
Read More
Exploring Racial, Ethnic Disparities in Cancer Care Prior Authorization Decisions
October 24th 2024On this episode of Managed Care Cast, we're talking with the author of a study published in the October 2024 issue of The American Journal of Managed Care® that explored prior authorization decisions in cancer care by race and ethnicity for commercially insured patients.
Listen
Motivating and Enabling Factors Supporting Targeted Improvements to Hospital-SNF Transitions
January 26th 2026Skilled nursing facilities (SNFs) with a high volume of referred patients with Alzheimer disease and related dementias may work harder to manage care transitions with less availability of resources that enable high-quality handoffs.
Read More

