- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
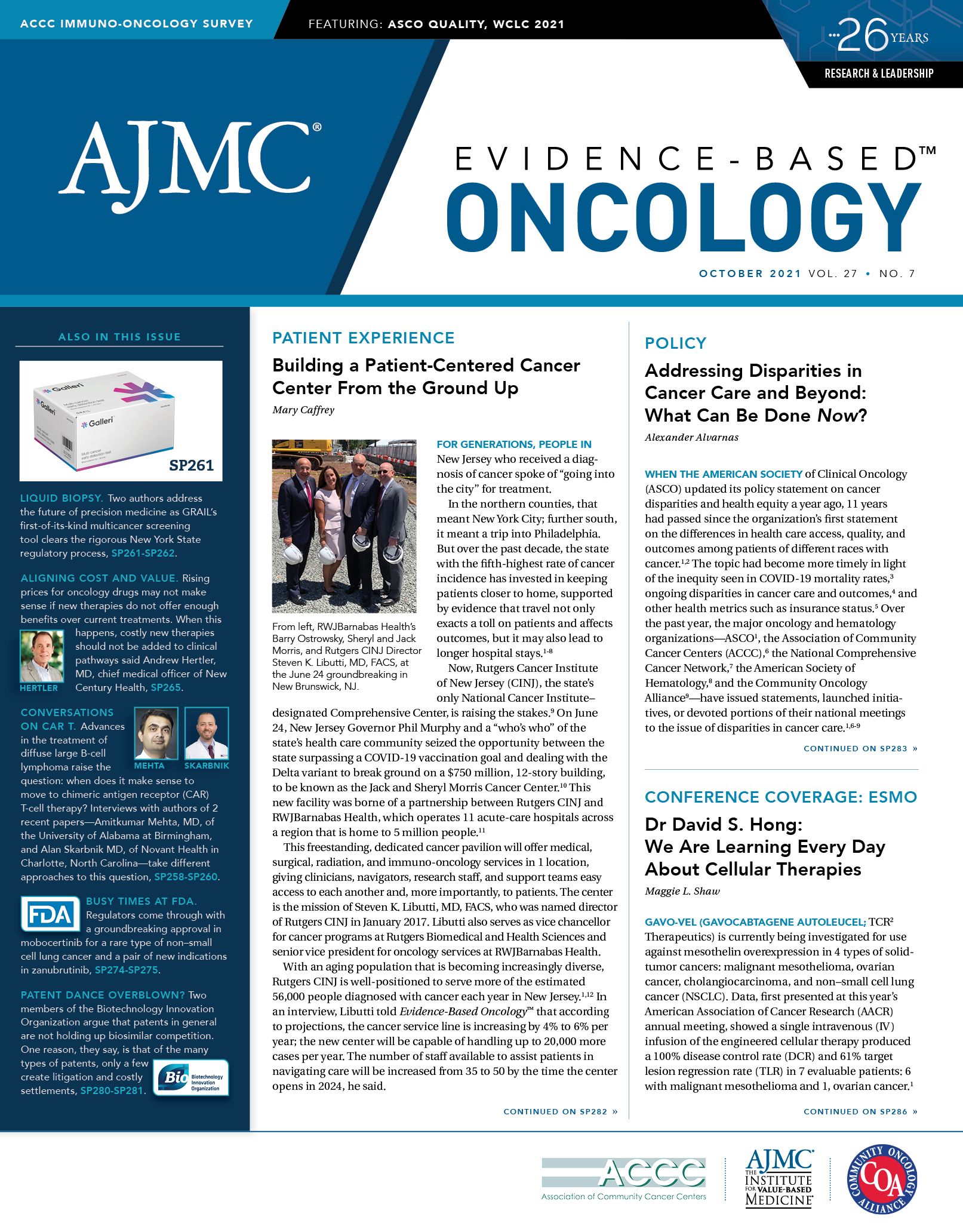
Specialty Therapies Offering Incremental Benefit Shouldn’t Be Added to Clinical Pathways, Hertler Says
Oncology drug costs have climbed rapidly, but price increases do not always align with the value the drugs offer, according to Andrew Hertler, MD, chief medical officer of New Century Health, a specialty care management company focused on oncology and cardiology in Brea, California.
The value of new oncology therapies comes from increasing survival and improving the quality of life for patients, but new therapies may provide only incremental benefit that comes with a high price tag, he said in a recent interview. “In 2020 alone, the average prices of new drugs coming to market [were] between $100,000 and $200,000 a year, with some drugs costing as much as $400,000 for an individual dose,” Hertler said.
“Realistically, there has to be a consensus solution for these high costs,” he added. “What we can do as physicians is to follow the clinical pathways for any clinical situation for what is the highest-value drug. To me, if a drug just isn’t that good, we shouldn’t use it. We routinely see approved drugs with 1.4 months to 1.6 months’ improvement in progression-free survival. For marginal drugs, we don’t have to put them on our pathways.”
Competition from newly approved therapies in the same class hasn’t worked to lower the cost. “Prices go up about 10% a year at pricing that is determined by what the market will bear. Patients really don’t have an option because they want to live. We don’t really have a shock on the price,” Hertler said.
An example, he said, is the checkpoint inhibitor class. Pembrolizumab (Keytruda; Merck), which targets the PD-1/PD-L1 pathway, was seen as a breakthrough when it received approval in 2014 to treat patients with advanced melanoma. It has since received additional approvals for 30 indications, the most recent being for the treatment of patients with high-risk early-stage triple-negative breast cancer in combination with chemotherapy before surgery and then continued as a single agent after surgery.1
Today, pembrolizumab has a wholesale acquisition cost of $10,0672 when given every 3 weeks compared with a monthly cost of $8,725 when it was approved.3 Since then, several other PD-1 checkpoint inhibitors have become available, including Bristol Myers Squibb’s nivolumab (Opdivo), Genentech’s atezolizumab (Tecentriq), and Regeneron’s cemiplimab (Libtayo).
The newest innovations, the chimeric antigen receptor (CAR) T-cell therapies, have an even higher price tag, especially when considering the total cost of patient care. In fact, the total cost of administering CAR T-cell therapies averaged more than $700,000 and, in some cases, exceeded $1 million, even though the wholesale acquisition cost of the treatment is $373,000, according to data from a recent real-world study from Prime Therapeutics in Eagan, Minnesota.4
Over 2.5 years, Prime Therapeutics’ investigators looked at 74 members of Blue Cross Blue Shield plans who received Novartis’ tisagenlecleucel (Kymriah) or Kite Pharma’s axicabtagene ciloleucel (Yescarta) for the treatment of B-cell lymphoma. The cost of CAR T-cell medication alone was $527,000 on average, which was 74% of the total cost during the initial treatment period. However, 12% of patients with post–CAR T-cell events incurred more than $1 million for their total cost of care, including drug and other costs, such as those for infusion center visits or transplants.
A 2018 Institute for Clinical and Economic Review (ICER) report estimated the cost-effectiveness of the 2 CAR T-cell therapies in B-cell cancers and suggested the therapies are priced in alignment with their clinical value, despite their high cost. The cost-effectiveness of both CAR T-cell therapies fell near or within commonly cited thresholds of $100,000 to $150,000 per quality-adjusted life years, according to the report.5 Because ICER’s study estimated only total treatment cost, Prime’s real-world evidence is another barometer to consider when evaluating whether CAR T cell’s pricing is in line with value.
A version of this article first appeared in Formulary Watch®.
References
1. FDA approves Keytruda (pembrolizumab) for treatment of patients with high-risk, early-stage triple negative breast cancer in combination with chemotherapy as neoadjuvant treatment then continued as single agent after surgery. News release. FDA. July 27, 2021. Accessed August 18, 2021 https://bit.ly/3CnyVO3
2. Keytruda cost info & financial help. Merck. Accessed August 18, 2021. https://www.keytruda.com/financial-support/
3. Cancer drug costs for a month of treatment at initial Food and Drug Administration approval. Center for Health Policy and Outcomes at Memorial Sloan Kettering Cancer Center. July 2, 2015. Accessed August 18, 2021. https://bit.ly/2W9de4H
4. Prime Therapeutics’ study shows total cost of care for CAR-T plus post-treatment events can exceed $1 million. News release. April 12, 2021. Accessed August 18, 2021. https://bit.ly/3kamTzZ
5. Institute for Clinical and Economic Review. Chimeric antigen receptor T-cell therapy for B-cell cancers: effectiveness and value final evidence report. March 23, 2018. Accessed August 18, 2021. https://bit.ly/3yV09tT