
- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Promise of Payment in Cancer Navigation Falls Short, Panelists Report
When the news came in 2023 that CMS would create billing codes to reimburse oncology practices that provided patient navigation services,1 the initial reaction was, “Finally!”
Many hoped practices could be compensated for the work done by nurses, social workers, or even lay navigators, who guide patients through the morass of scheduling, paperwork, and emotional upheaval of the cancer journey. After all, evidence shows that navigators help keep patients out of the hospital, reduce costs, and close the survival gap between different racial groups.2,3
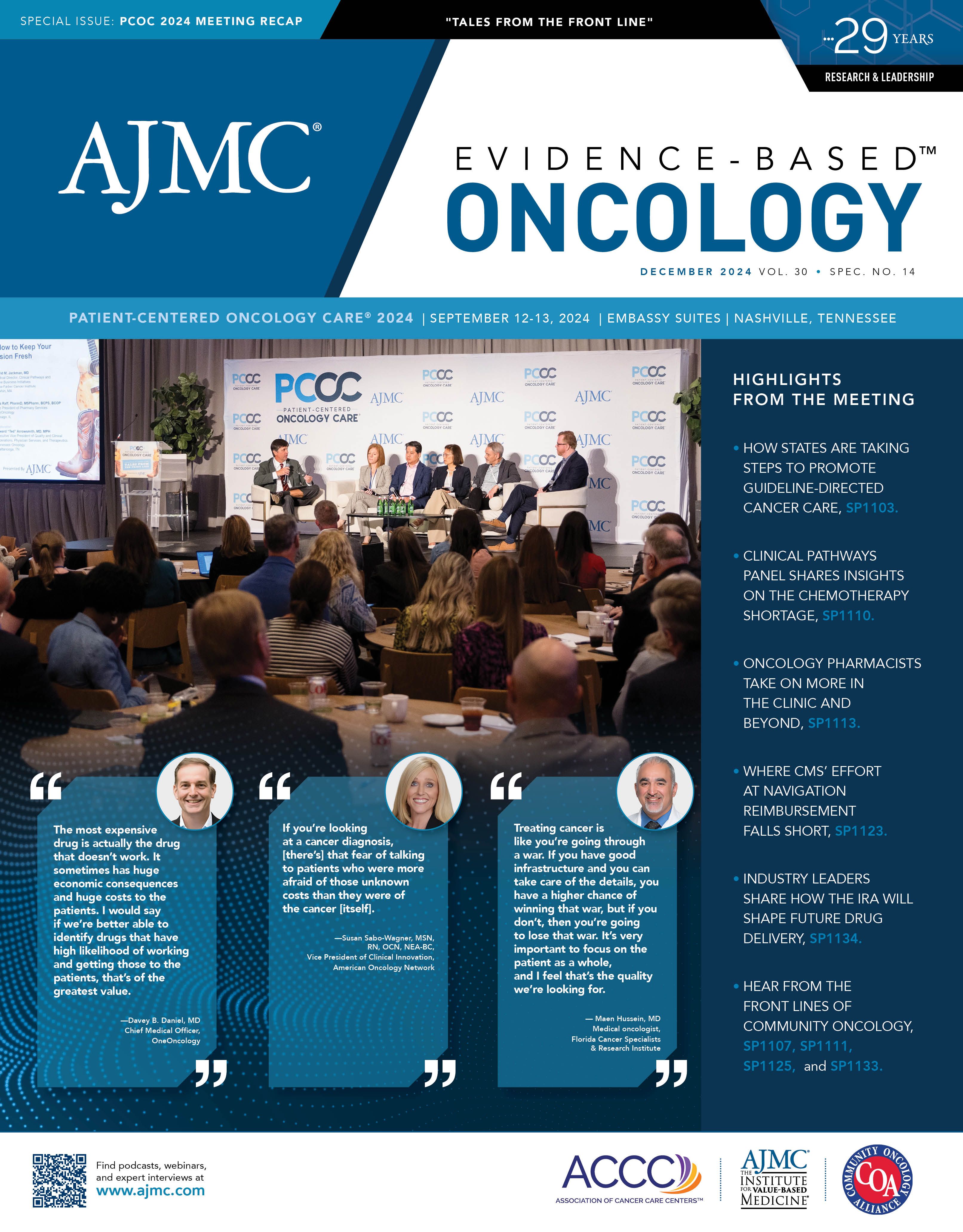
But 9 months into working with the principal illness navigation (PIN) codes, those in the trenches find that getting paid is not easy and can create unanticipated headaches. That was the assessment of panelists appearing during the second day of Patient-Centered Oncology Care (PCOC) for “The New Math: What Does PIN Mean to the Enhancing Oncology Model?”
Lalan Wilfong, MD | Image credit: LinkedIn

PCOC Cochair Lalan Wilfong, MD, senior vice president for value-based care at Thyme Care, moderated a panel experienced with the details of CMS’ Oncology Care Model (OCM), including some who are also working with the current Enhancing Oncology Model (EOM). The panelists included the following:
- Grant Andres, MSN-RN, BSc, DC, CLSSBB, CPHQ, senior director for clinical operations at Arizona Oncology;
- Samyukta Mullangi, MD, MBA, medical oncology director, Thyme Care and a medical oncologist at Tennessee Oncology;
- Judi Payne-De Bock, BSN, senior director of clinical services with The US Oncology Network;
- Barry Russo, MBA, CEO at The Center for Cancer and Blood Disorders, which serves the Dallas-Fort Worth, Texas, region; and
- Dax Kurbegov, MD, senior vice president at Sarah Cannon Cancer Network, in Nashville, Tennessee.
The question of whether navigation works isn’t the issue, the panelists agreed.
Samyukta Mullangi, MD, MBA | Image credit: LinkedIn

“In study after study, we’ve seen that navigation can drive benefits for patients in both fee-for-service and value-based care settings,” Mullangi said. “The outcomes that we see are positive across the board in terms of not just physician experience and patient experience, but metrics such as time to treatment, persistence and retention on treatment, quality of life, symptoms, acute care utilization, and, in sum, total cost of care for the system.”
Initially funded by grants, navigation is now “embedded in the context of sustainable business models,” she said.
Russo said his practice started navigation in 2006. “We didn’t know what we were doing, but we started with a mindset of advocacy,” he said. “We wanted somebody in our practice whose role was advocacy and had enough clinical knowledge to help patients.”
The addition of social workers, dietitians, geneticists, and other professionals “has made a huge difference,” Russo said. “It’s managing the whole person, and it takes a village to do that.” And when practices do things the right way, he said, “Miraculously enough, what you’re supposed to be doing also reduces costs.”
Dax Kurbegov, MD | Image credit: Sarah Cannon

Kurbegov said within a large health system, navigators can play a crucial role in keeping patients from falling through the cracks when moving from a medical oncologist to a radiation oncologist. “How do we support those patients through their transitions?” he said. “When that patient leaves the medical oncologist domain to move into radiation therapy, we saw so many gaps that occurred there, and so for our health system, it was about helping that patient stay on the treatment program.”
The new PIN codes to pay for navigation don’t arrive in a vacuum, panelists explained. CMS has previously introduced other codes for principal care management (PCM) and chronic care management (CCM) for patients who have a single or multiple serious chronic conditions, respectively. On top of that, CMS has launched the EOM to replace the OCM, and it has now tweaked the EOM to upgrade the reimbursement formula more favorably for practices.
Grant Andres, MSN-RN, BSc, DC, CLSSBB, CPHQ | Image: Arizona Oncology

Andres explained how complex it is for practices to decide how to bill for a patient with this cornucopia of options. On the plus side, he’s encouraged to see billing for navigation introduced. “I can say that our support services, including navigation, social work, and nutrition, have had a profound impact on our patient care.”
“However, on the challenging side, you know you can’t talk about [PIN] without talking about principal care management,” Andres said. “The 2 go hand in hand, and they have subtly different rules that dictate how you might implement them.”
Practice technology, including the electronic health record, must be able to capture time down to the minute or it will be impossible to accurately log how much time has been spent with a patient, which is the essential factor needed for billing. The challenges cited by Andres and others include the following:
Billing under PIN codes must be for a full hour, but that is not typically how navigation services are delivered. By contrast, Payne-De Bock said, PCM requires 30-minute increments and time can be spent on non-nursing tasks such as working through prior authorization challenges.
Barry Russo, MBA | Image credit: The Center for Cancer and Blood Disorders

PIN codes can be billed alongside the EOM, but CCM and PCM cannot, so practices must evaluate in advance which program best fits a patient’s needs.
Although many practices converted to navigation via telehealth during the pandemic, PIN codes cannot be billed if services are administered this way, which Andres said is a major problem for many practices.
Some Medicare patients were being charged very high co-pays, which practices were required to collect. So, in some cases, navigation billing is skipped to avoid billing patients a co-pay.
Andres said for Arizona Oncology, “The only way our team of 4 navigators can be effective is by telehealth. And so that became an unfortunate deal-breaker.”
As the PIN codes are brand new, Wilfong said he hoped CMS would revisit some of the “boneheaded” parts of the new rule. “These codes are for the patients most at risk, and there’s a co-pay, and you have to collect the co-pay, right? You were legally obligated to collect the co-pay unless patients meet criteria for waiving it, which is really hard. And there’s no telehealth. So, the patients who have the hardest time getting to our clinics and they’re most at risk—we can’t use telehealth to reach out to them.”
Mullangi said she, too, interpreted the language as a barrier to the use of telehealth. “I do think that it’s actually worthwhile for Medicare or CMS to issue some sort of clarification around the telehealth issue because I read it the same way, which is that it’s not really available as a mechanism of reaching patients. But I also was wondering whether they were vague on whether we could use telehealth because they didn’t want to tie the provision of this service to the ongoing renewal cycle of the Telehealth [Modernization] Act and appropriations toward that.”
Andres noted that additional requirements from CMS at the end of the OCM, including that practices return to participation in the merit-based incentive payment system, meant that resources were necessarily put into these areas. But Andres believes that the oncology community shouldn’t give up on billing for navigation just yet.
Judi Payne-De Bock, BSN | Image credit: The US Oncology Network

“It’s really a step forward for Medicare to put these codes in place,” he said. “I think we have a responsibility to do everything we can to put our pieces in place, like time capture and the billing piece of that, but we also have a responsibility to advocate with Medicare about what the true needs are associated with establishing these programs and making them work effectively to benefit patients.”
Payne-De Bock said work is ongoing to create a decision-making tool that will help care teams evaluate a patient based on comorbidity status to gauge which billing program makes the most sense. “If it is an intense patient with lots of comorbidities, a lot of other needs as well, then you know the appropriate program would be PIN,” she said. “If there are patients who are newly diagnosed and [on a] complicated therapy, maybe then it’s [PCM]. It’s really trying to fit the patient into the best program to meet their needs.”
References
1. CMS-1784-F. CMS. November 16, 2023. Accessed January 19, 2024. https://www.cms.gov/medicare/medicare-fee-service-payment/physicianfeesched/pfs-federal-regulation-notices/cms-1784-f
2. Kline RM, Rocque GB, Rohan EA, et al. Patient navigation in cancer: the business case to support clinical needs. J Oncol Pract. 2019;15(11):585-590. doi:10.1200/jop.19.00230
3. Chan RJ, Milch VE, Crawford-Williams F, et al. Patient navigation across the cancer care continuum: an overview of systematic reviews and emerging literature. CA Cancer J Clin. 2023;73(6):565-589. doi:10.3322/caac.21788
2 Commerce Drive
Cranbury, NJ 08512
AJMC®
All rights reserved.