- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
After CAR T in Mantle Cell Lymphoma, Choices and a Robust Pipeline
Mantle cell lymphoma treatment offers options if patients relapse after CAR T-cell therapy, from bispecific antibodies, antibody drug conjugates, and other emerging therapies.
Five years ago this week, treatment for mantle cell lymphoma (MCL) took a leap forward with FDA’s approval of brexucabtagene autoleucel, or brexu-cel (Tecartus; Kite Pharma/Gilead).1 Patients who had been resistant or relapsed on other therapies showed a 62% complete remission rate in the ZUMA-2 trial (NCT02601313),2 offering hope in this rare form of non-Hodgkin lymphoma that presents differently in patients depending on age and risk factors. Prior to the approval, the National Institutes of Health reported a 5-year progression free survival (PFS) rate of 62% for MCL among patients under age 65, compared with 37% for those age 75 or older.3
Named for the mantle zone—where cancerous B cells germinate in the lymph nodes—the disease is typically not diagnosed until it has already reached an advanced stage. Even when early treatment is successful, relapse is expected. Thus, the hope of CAR T-cell therapy is tempered by the likelihood that many patients will need someday need more treatment.
The question in MCL then is, what comes after CAR T? And what options are available to patients who are not CAR T eligible?
Options abound, thanks to improvements in both therapy and the ability to predict the course of the disease, according to a review article appearing this month in Cancers.4 Adding the Ki-67 proliferation index to the Mantle Cell Lymphoma International Prognostic Index (MIPI) and use of other indicators—TP53 and blastoid status—have allowed clinicians to identify patients with aggressive disease, who need treatment other than traditional chemoimmunotherapy followed by autologous stem-cell transplant. More recently, the use of minimal residual disease (MRD) assessment has shown promise.5
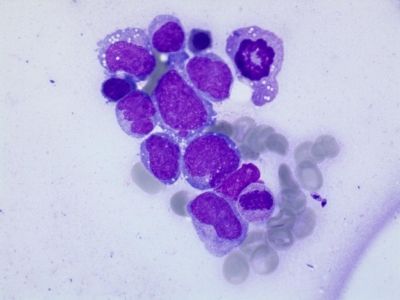
Bone marrow smear from a patient with relapsed mantle cell lymphoma | Image: GECH Atlas
For years, younger, fit patients with MCL received chemotherapy followed by ASCT, with rituximab for maintenance, while older and less fit patients received a combination with bendamustine plus rituximab. Use of Bruton tyrosine kinase (BTK) inhibitors in frontline therapy changed all that, and second-generation therapies such as acalabrutinib and zanubrutinib have improved both efficacy and safety, both as monotherapy and in combinations. Pairing BTK inhibitors with venetoclax, a BCL-2 inhibitor, offered complementary benefits; several recent and ongoing trials involve both early- and next-generation BTK and BCL-2 inhibitors.4 Of note, the phase 2 BOVen trial offered the chemotherapy-free combination of zanubrutinib, obinutuzumab, and venetoclax in untreated patients with MCL and a TP53 mutation; among 25 patients, the overall response rate (ORR) was 96% and the complete response rate was 86%. Two-year PFS was 72%, and OS 76%.6
Since 2020, CAR T-cell therapy has proved transformative—but not for everyone. Those treated recently treated with bendamustine did not see the same benefits.7 Today’s approved therapies and new treatments in the pipeline offer multiple mechanisms of action for clinicians and for patients. The review article lists more than 50 ongoing clinical trials that involve both new therapies and new combinations of approved therapies for patients with MCL already treated with CAR T and a BTK inhibitor.4
Non-covalent BTK Inhibitors
Led by pirtobrutinib (Jaypirca; Eli Lilly), these therapies offer promise to patients who have developed resistance to first-generation BTKs. Pirtobrutinib has received accelerated approval for patients with MCL after at least 2 therapies,8 while Merck’s nemtabrutinib is being studied in various NHL subtypes (NCT04728893), including MCL. Investigators are still examining why non-covalent BTK inhibitors may be especially effective in MCL; the authors write that mutations of the cyclin D1 gene already present, along with acquired mutations in the BTK enzyme, may “prevent formationof an irreversible covalent bond between the drug and enzyme,” limiting efficacy of early-generation BTKs.4
Monoclonal Antibodies
The authors cover progress in studying both unconjugated and antibody-drug conjugates (ADCs), including:
- Zilovertamab vedotin is described as “an immunoconjugate targeting ROR1, carrying the toxin monomethyl auristatin E.” In the waveLINE-006 study (NCT05458297) that included 40 R/R patients with MCL, the overall response rate was 40%.9
- Loncastuximab-tesirine, which targets CD19, is previously approved in R/R diffuse large B-cell lymphoma. It is being studied as both a monotherapy and in combination with ibrutinib and durvalumab in various R/R B-cell malignancies, including MCL.4
Bispecific Antibodies
These agents, many of which have approvals in more common types of NHL, harness distinct immune mechanisms to target MCL cells. These include:
- Glofitamab (Columvi; Genentech), approved in DLBCL after 2 lines of therapy, targets CD20xCD3 with a 2:1 tumor–T-cell binding configuration, which the authors write, “translates into bivalent binding to CD20 on B cells and monovalent binding to CD3 on T cells, leading to T-cell engagement and redirection against malignant B cells.” Its phase 2 study (NCT03075696) produced an ORR of 85.0% and a CR of 78.3% with manageable toxicities; the authors note that the trial was complicated by COVID-19, which contributed to dose interruptions for 60% of the patients and 8 deaths, with 6 due to COVID-19.4,10
- Epcoritamab (Epkinly; Genmab/AbbVie), approved in DLBCL and follicular lymphoma,also targets CD20 and CD3; here, the dose-escalation study included only 4 patients with MCL.4
- Mosunetuzumab (Lunsumio; Genentech) targets CD20xCD3 but has an altered Fc that does not bind to the complement or Fc gamma receptor. It is approved in follicular lymphoma after 2 lines of therapy and is being studied across NHL subtypes, including MCL, both as a single agent and in combinations, including 1 with polatuzumab vedotin. In a study that included 20 patients with MCL (NCT03671018), including 40% with MIPI scores that indicated high-risk features, ORR and CR rates were 75% and 70%, respectively, with the authors stating, “These data are encouraging about this treatment combination in heavily pretreated and very high-risk MCL patients.”4
- Odronexatamab was also investigated in the R/R MCL setting. A phase 1 trial (NCT02290951) of patients with multiple NHL subtypes included 12 patients with MCL; this group had an ORR of 50% but higher rates of cytokine release syndrome than seen in other subtypes.4
Allogeneic Stem Cell Transplantation
The authors reviewed several studies involving allogeneic transplant (allo-SCT) after CAR T, noting there is limited prospective evidence. A retrospective study from Spain reported a 5-year event-free survival rate of 47% and OS of 50% for 135 patients. The chief concerns with allo-SCT are infections and graft vs host disease (GVHD).11
New Therapeutic Targets
Future MCL treatment will likely include new drug clases, including PI3K inhibitors, with copanlisib and linperlisib under study. Alisertib, a selective aurora A kinase inhibitor, avelumab, an anti-PD-L1 monoclonal antibody, and additional novel BTK inhibitor and BTK degraders are under study. Finally, new CAR T-cell therapies are in the pipeline, with various targets and some with allogeneic mechanisms.
Finally, trials are under way using well-known therapies, including carfilzomib (Kyprolis; Amgen), ixazomib (Ninlaro; Takeda), lenalidomide (Revlimid, Bristol Myers Squibb), nivolumab (Opdivo, Bristol-Myers Squibb), and blinatumomab (Blincyto; Amgen).
“In mantle cell lymphoma, the anticipation of BTK inhibitors in the first-line setting and the spreading of CAR-T-cells therapy completely changed the landscape,” the authors concluded. “However, many cases do not yet respond or relapse after CAR-T cells, and a subset of patients are not eligible for CAR-T in the first place. This setting of MCL patients still represents a challenge and an unmet clinical need.”4
The large number of studies involving many different drug classes, both old and news, promises a “meaningful impact,” they wrote, “firstly on relapsed/refractory (R/R) disease and subsequently also in earlier treatment lines.”
References
- FDA approves brexucabtagene autoleucel for relapsed or refractory mantle cell lymphoma. Published online July 27, 2020. Accessed July 17, 2025. https://www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-brexucabtagene-autoleucel-relapsed-or-refractory-mantle-cell-lymphoma
- Wang M, Munoz J, Goy A. KTE-X19 CAR T-cell therapy in relapsed or refractory mantle-cell lymphoma. N Engl J Med. 382(14):1331-1342. doi:10.1056/NEJMoa1914347
- Cencini E, Calomino N, Franceschini M. Survival outcomes of patients with mantle cell lymphoma: a retrospective, 15-year, real-life study. Hematol Rep. 16(1):50-62. doi:10.3390/hematolrep16010006
- Boccellato E, Comba L, Tavarozzi R. Next-generation therapies in mantle cell lymphoma (MCL): The evolving landscape in treatment of relapse/refractory after CAR-T cells. Cancers (Basel). 17(13):2239. doi:10.3390/cancers17132239.
- Duarte C, Major A. Treatment of TP53-mutated mantle cell lymphoma: Selecting the optimal regimen for specific patient populations. ASCO Daily News. April 23, 2025. Accessed July 17, 2025. https://dailynews.ascopubs.org/do/treatment-tp53-mutated-mantle-cell-lymphoma-selecting-optimal-regimen-specific-patient.
- Kumar A, Soumerai J, Abramson JS. Zanubrutinib, obinutuzumab, and venetoclax for first-line treatment of mantle cell lymphoma with a TP53 mutation. Blood. 145(5):497-507. doi:10.1182/blood.2024025563.
- Iacoboni G, Navarro V, Martin-Lopez AA. Recent bendamustine treatment before Apheresis has a negative impact on outcomes in patients with large B-cell lymphoma receiving chimeric antigen receptor T-cell therapy. J Clin Oncol. 2025;42(2). doi:10.1200/JCO.23.01097
- FDA grants accelerated approval to pirtobrutinib for chronic lymphocytic leukemia and small lymphocytic lymphoma. FDA. Published online December 7, 2023. Accessed July 17, 2025. https://www.fda.gov/drugs/resources-information-approved-drugs/fda-grants-accelerated-approval-pirtobrutinib-chronic-lymphocytic-leukemia-and-small-lymphocytic
- Gilmelius I, Kim WS. Zilovertamab vedotin monotherapy for patients with relapsed or refractory mantle cell lymphoma: cohort a of the multicenter, open-label, phase 2 Waveline-006 study. Blood. 2024;144((suppl 1)):4405. doi:10.1182/blood-2024-205897
- Phillips TJ, Carlo-Stella C, Morschhauser F. Glofitamab in relapsed/refractory mantle cell lymphoma: results from a phase I/II study. J Clin Oncol. 2024;43(3). doi:10.1200/JCO.23.02470
- DiBlasi R, LeGouill S, Bachy E. Outcomes of patients with aggressive B-cell lymphoma after failure of anti-CD19 CAR T-cell therapy: a DESCAR-T analysis. Blood. 2022;140(24):2584-2593. doi:10.1182/blood.2022016945
