- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
SPOTLIGHT: Redefining Patient-Provider Relationships: Cancer Survivor Matthew Zachary
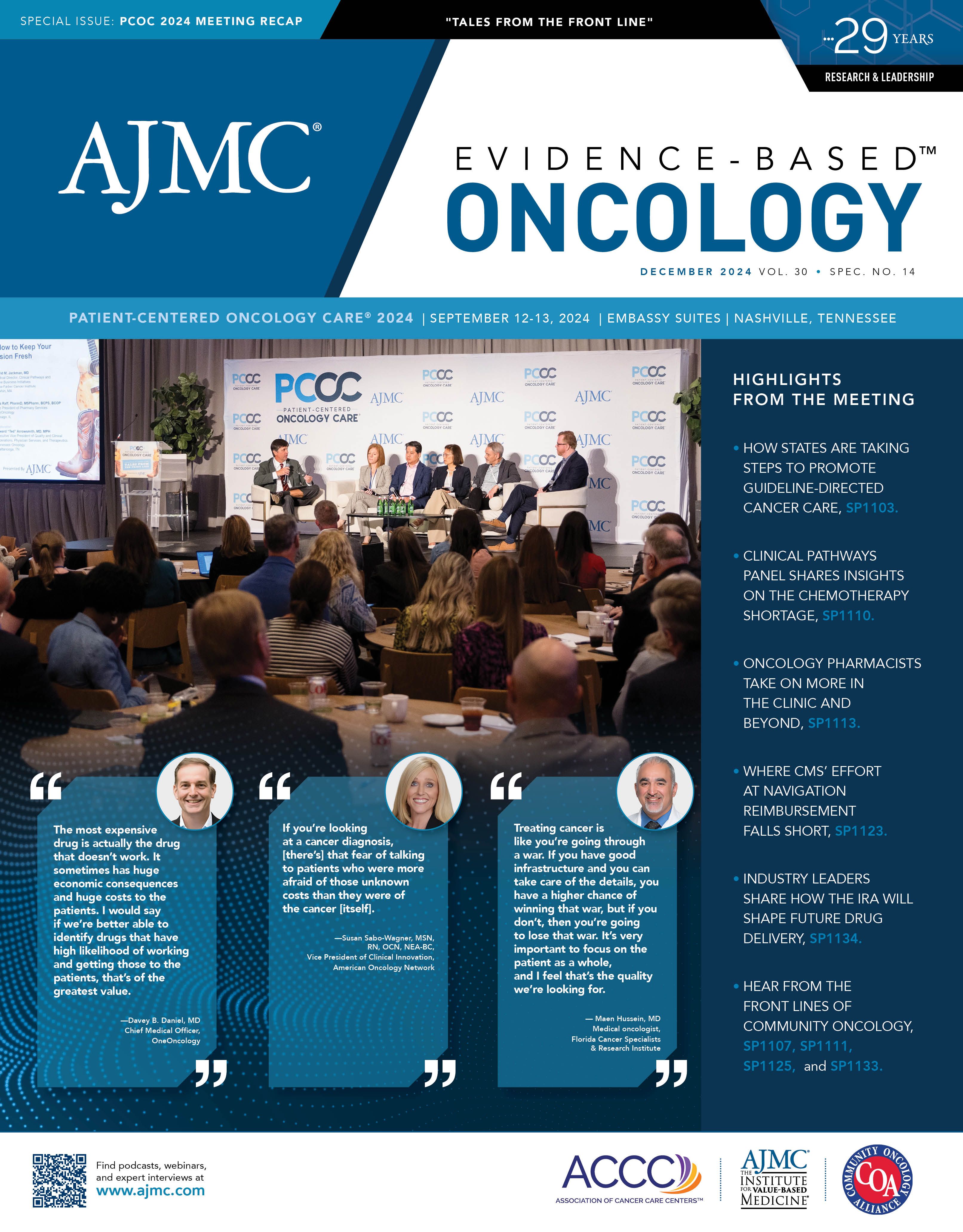
Matthew Zachary, founder of the nonprofit organization Stupid Cancer, was the keynote speaker at The American Journal of Managed Care’s (AJMC’s) 2024 Patient-Centered Oncology Care (PCOC) meeting.
This transcript was lightly edited for clarity.
AJMC: How has your perspective on patient-centered care evolved over the years as both a survivor of cancer and an advocate, particularly as you have witnessed the advancements in cancer treatment and technology?
Zachary: I am one of the oldest cancer survivors in the country from the ’90s to have worked in health care policy, nonprofit [organizations], all the rigamarole. The progress I see is vastly different, because when I was diagnosed, there was no internet, no one cared about you, [and] there was no such thing as mental health. It was a sort of walk-it-off therapy and many people died.
From that perspective, things are better now, but now it’s more complicated. There are better drugs, there are new drugs, [and] things are more expensive. The economy tanks, does great things, and then tanks again. There’s no certainty that people will get what they deserve, what they need; instead, they’re being told, “just go do this.”
AJMC: How has the concept of putting the patient at the center of every conversation influenced your organization?
Zachary: I was talking about consumer oncology 20 years ago. Patients, yes, that’s a word. But patients are still people who need to buy things and think things and do things. If you start to treat patients like humans and consumers with empathy, understanding who they are, what they need, [and] what’s important to them first, then people will save money, people will make better decisions, and at the end of the day, more people will survive with the dignity and quality of life that they need.
It’s important to understand, yes, that, ideally, is the customer, even though the doctor is the customer of health care. When you start to think about the role the patient plays as a consumer in their own decisions, being more empowered, more aware, [and] more fed up, it’s time to take that seriously. Because if you don’t meet them where they’re at, your business will fail.
AJMC: How can care providers and organizations continue to improve efforts to put patients at the center of every conversation?
Zachary: I’m going to flip that [question]. How can patients help providers to be better? We have to have empathy for them, as well. I’m digging into this sort of ulterior conversation on mental health and burnout and fatigue. We’re looking at a system where providers are trying to practice [the Hippocratic Oath] every day, and they’re being crushed by a system they hate being in. How does that affect the way they manage patient relationships?
You could say you are patient-centered, but at the end of the day if you’re crying at night, you can’t see your kids, you’re not being supported, your union isn’t working, that’s not helping anything right now. As much as patients can deride and ridicule and pander [providers with] “you’re not really patient-centric,” “[you have a] lack of empathy,” these are human beings too, who I’m on the side of defending because without them at their best, we are not at our best as patients.