- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
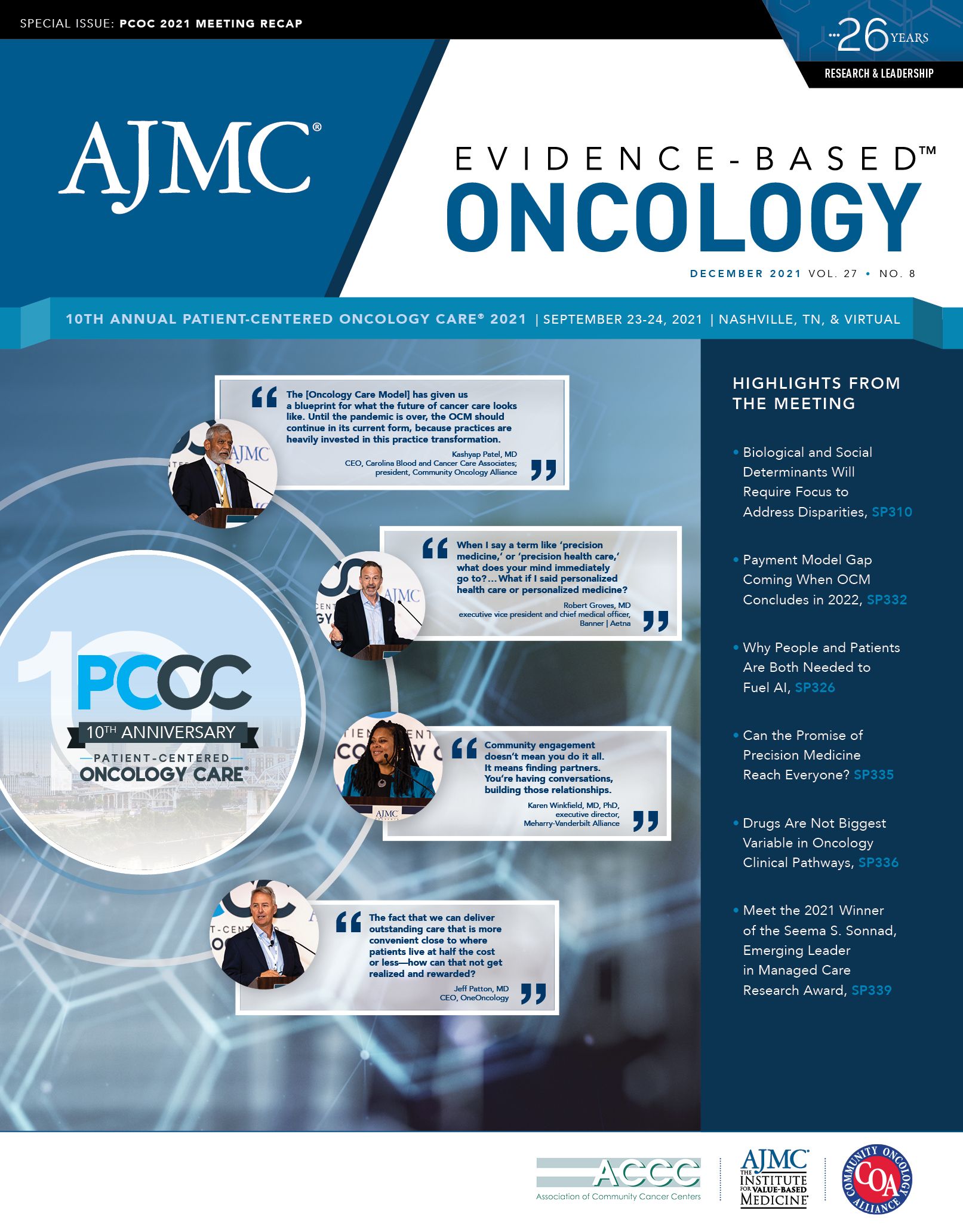
Precision Medicine Can Close Oncology Gaps—and Lead to “Doing Less”
Physicians said it is in payers’ interest to use artificial intelligence to address social determinants of health, to cover tests, and to gather data. Doing so could let them stratify who needs certain screenings and diagnostic procedures and who doesn’t, which could lead to less consumption of health care.
At one point in the discussion, “Precision Medicine: Innovation in Testing and Technology,” moderator Joseph Alvarnas, MD, noted that the 2 most recent American Cancer Society reports on survival had shown the largest drops in mortality ever recorded.1 This was due to the rise of genomic-informed targeted therapeutics, particularly in non–small cell lung cancer, which accounts for the largest share of cancer deaths.
The question, said Alvarnas, a cochair for Patient-Centered Oncology Care®, is whether the benefits of precision medicine can be distributed evenly across all racial, ethnic, and geographic groups; recent data show that is not the case. Patients who rely on Medicaid, and in some cases Medicare, may lack access to the tests that are essential for identifying patients who should receive therapies in certain genomic-driven ovarian, prostate, or lung cancers.2,3
“In some ways, the advances in precision medicine have far outpaced our systems to deliver this kind of care and our systems for figuring out how best to pay for it,” Alvarnas said.
Panelists agreed that closing these gaps requires broadening the concept of “precision medicine” to include social determinants of health—those factors that can affect access to care, including clinical trials, or the ability to stick with a treatment regimen.
Ultimately, the physicians on the panel pointed out, it is in payers’ interest to use artificial intelligence to address these factors, cover tests, and gather data. Doing so could let them stratify who needs certain screenings and diagnostic procedures and who doesn’t, which could lead to less consumption of health care.
Joining Alvarnas, a hematologist-oncologist and vice president for government affairs at City of Hope in Duarte, California, were:
• EDMONDO ROBINSON, MD, MBA, MS, FACP, senior vice president and chief digital officer, H. Lee Moffitt Cancer and Research Institute, Tampa, Florida;
• PRASANTH REDDY, MD, MPH, FACP, senior vice president and enterprise oncology head, Labcorp, Mission, Kansas; and
• ELIZABETH KWO, MD, MBA, MPH, deputy chief clinical officer, Anthem Blue Cross Blue Shield, Boston, Massachusetts.
Alvarnas asked how different institutions were “grappling with this amazing domain of care.”
Robinson said that Moffitt, as Florida’s only National Cancer Institute Comprehensive Center, brings information technology, health data services, digital innovation, and clinical pathways together under its Center for Digital Health, which he oversees.
This setup allows Moffitt to accelerate its research efforts and fold in consumer digital elements as well, Robinson noted.
At Labcorp, Reddy said his mission is “to unlock the power of precision diagnostics.” Multipanel testing, increased access to clinical trials, and a data strategy that includes clinical decision support are all key.
“If we do broad panel testing, perhaps 20% to 30% of the results across all cancer subtypes are going to lead to a standard-of-care alteration. How do we make that 70% to 80%?” Reddy asked.
Making clinical trials a treatment option is one way, although “it’s been a struggle,” he said. “We’re very deeply committed to ensuring that when there are alterations, [we] have a viable therapeutic associated with them. How do we accelerate the ability of those patients to access those therapeutics?”
Today, Reddy said, there is “an incredible pipeline” of oncology treatments undergoing trials. The challenge is to connect patients with trials “to advance the standard of care.”
Alvarnas asked Kwo how payers view the changes in precision medicine and what is being done to capitalize on the possibilities with risk stratification and therapy selection. According to Kwo, the abundance of available data has already allowed payers to reduce costs, for avoidable emergency department admissions for postchemotherapy dehydration, for example.
Opportunities exist in the precision diagnostics area, she said, but as others had noted throughout the PCOC discussions, “this is something where payers are really inclined to only see the value if there is something that you can extract from it.” Payers tend to put their dollars into testing when it involves the highestrisk patients and distinguishing when the highest cost
therapies should be used.
“If there’s a change in diagnosis, once a [testing] decision supports a physician and/or a nurse, it can really make a difference,” Kwo said. “When it’s just [broad-based] screening, I think payers tend to be a little bit shy.”
Alvarnas then asked for comment on an area of controversy: Does the lack of genomic diversity in data sets—the ones clinicians rely upon when deciding if a patient has a given mutation—lead to their lack of generalizability?
“It’s a critical, critical question,” Reddy responded. “To me, this represents something that’s [essential] to understanding the biology of cancer itself; it’s a population health question.”
As an example, he said, “EGFR rates in 2001 weren’t what they are today.” For communities of color that aren’t taking part in clinical trials, due to social determinants of health or other factors, it’s important to understand that not only are they missing out for themselves, but the data are not being collected.
“That is our challenge. That is also our opportunity,” he explained. “So it’s critical that we increase access of testing so that we know who’s going to benefit from these therapies.”
According to Reddy, this is not just an issue for the United States, it’s a global issue.
On the flip side, how do we ensure that the data collected are used in a meaningful way and that nothing in the huge amount of information gathered is overlooked?
Robinson believes this is a major issue. The phenomenon of “alert fatigue” is real, and the top complaint is that electronic health records (EHRs) are cumbersome and time-consuming to use. At Moffitt, the clinical informatics and user interface/user experience teams spend a lot of time thinking about exactly which data sets are presented to clinicians—and how—so that the most important insights from clinical data, diagnostic tests, social determinants of health, and other information are presented in a holistic way.
“We’re all thinking about how we actually operationalize these concepts,” Robinson said, something that is essential if remote patient monitoring or hospital in the home will be added to the mix, he noted.
Alvarnas asked Kwo to comment on the issue of access to precision medicine, especially with the promise of liquid biopsies, given that they are less invasive and could be performed at different points in the course of care. Kwo said payers are definitely interested in exploring different options, and that Anthem is working with Medicare and Medicaid “to figure out what is appropriate.”
“If we’re able to catch a patient earlier, of course, there’s a benefit for the quality side and patient satisfaction and life, longevity. But there’s also an
interest in catching the patient earlier so that you can reduce medical costs down the line,” Kwo said. The challenge is justifying the screening methodologies to reduce medical cost within a 12- to 18-month time frame, which is what most payers consider, she continued.
This brought Alvarnas to a key point: precision medicine isn’t just about picking a particular therapy—it could be about picking no therapy or no screening. Population-wide screenings of every patient when they hit a certain age might be stratified based on additional risk factors; perhaps high-risk patients could get a colonoscopy in their 40s, whereas others might wait until their 60s.
Robinson agreed. “We haven’t spent enough time exploring when we can do less,” he said.
Alvarnas asked the group which approach their institutions take: whole genome sequencing or RNA sequencing. “How do you choose?” he asked. “Are you looking to control costs by limiting the number of tests up front? Or do you look more broadly at panel testing to be able to find both high-risk and low-risk populations by expanding upfront costs and expanding the upfront knowledge and information?”
Robinson noted that it’s important to look at individual patient needs, including social determinants of health. “We love our genomics, right? But what about [asking ourselves] ‘who is this human being?’ They’re not just a set of genes….What’s their social structure? What’s their family support structure?” These things matter greatly to treatment outcomes, he said.
Kwo pointed out that payers are increasingly interested in these questions. She also noted that there are many questions about how to collect the data needed to understand these issues, as well as how to reimburse providers for helping collect the data. To get to the point of using tools such as liquid biopsy to reduce medical care consumption, she said, “is music to so many payers.”
Can innovation bend the cost curve, Alvarnas asked, in a way that offers better stewardship of care?
“It’s a complex question,” Reddy replied. “I do believe that we are at the nexus of a unique time in oncology. I’ve been practicing for close to 20 years,
and we are sitting in an uncharted place where we can make a difference,” he said. We have the diagnostic tools, we have amazing therapeutic pipelines, and we have the ability to access vast amounts of data, he noted. Most of our understanding of drugs, 95% to 97%, really comes from clinical practice, not from clinical trials.
“How do we look at that data? How do we use that information to design better clinical trials?” he continued. “How do we look at the data and make sure that we’re not [omitting] groups of folks that are being left out of good health care and making sure they get the benefits of the tools that we have at our disposal?”
“For me,” Reddy concluded, “it’s [a matter of] alignment, it’s communication, and it’s education.”
References
1. Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer Statistics, 2021. CA Cancer J Clin. 2021;71(1):7-33. doi:10.3322/caac.21654
2. Gamble CR, Huang Y, Wright JD, Hou JY. Precision medicine testing in ovarian cancer: the growing inequity between patients with commercial vs Medicaid insurance. Gynecol Oncol. 2021;162(1):18-23. doi:10.1016/j.
ygyno.2021.04.025
3. Larson KL, Huang B, Chen Q, et al. EGFR testing and erlotinib use in non-small cell lung cancer patients in Kentucky. PLoS One. 2020;15(8):e0237790. doi:10.1371/journal.pone.0237790