- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Genetics, Epigenetics, and Cancer: What Data Are We Missing?
During the discussion of disparities in cancer care, one panelist explained that the National Institutes of Health definition of precision medicine is broader than most people realize.
A flashpoint in the discussion of disparities in cancer care concerns data:
If most of the data collected on genetic mutations come from White Europeans, what insights might we have missed? Will approved therapies offer the same level of efficacy in patients of color?
More importantly, what data beyond a person’s genetics are not accounted for in today’s clinical trials that could affect cancer outcomes? And how can artificial intelligence (AI) enable these factors to be part of the care equation?
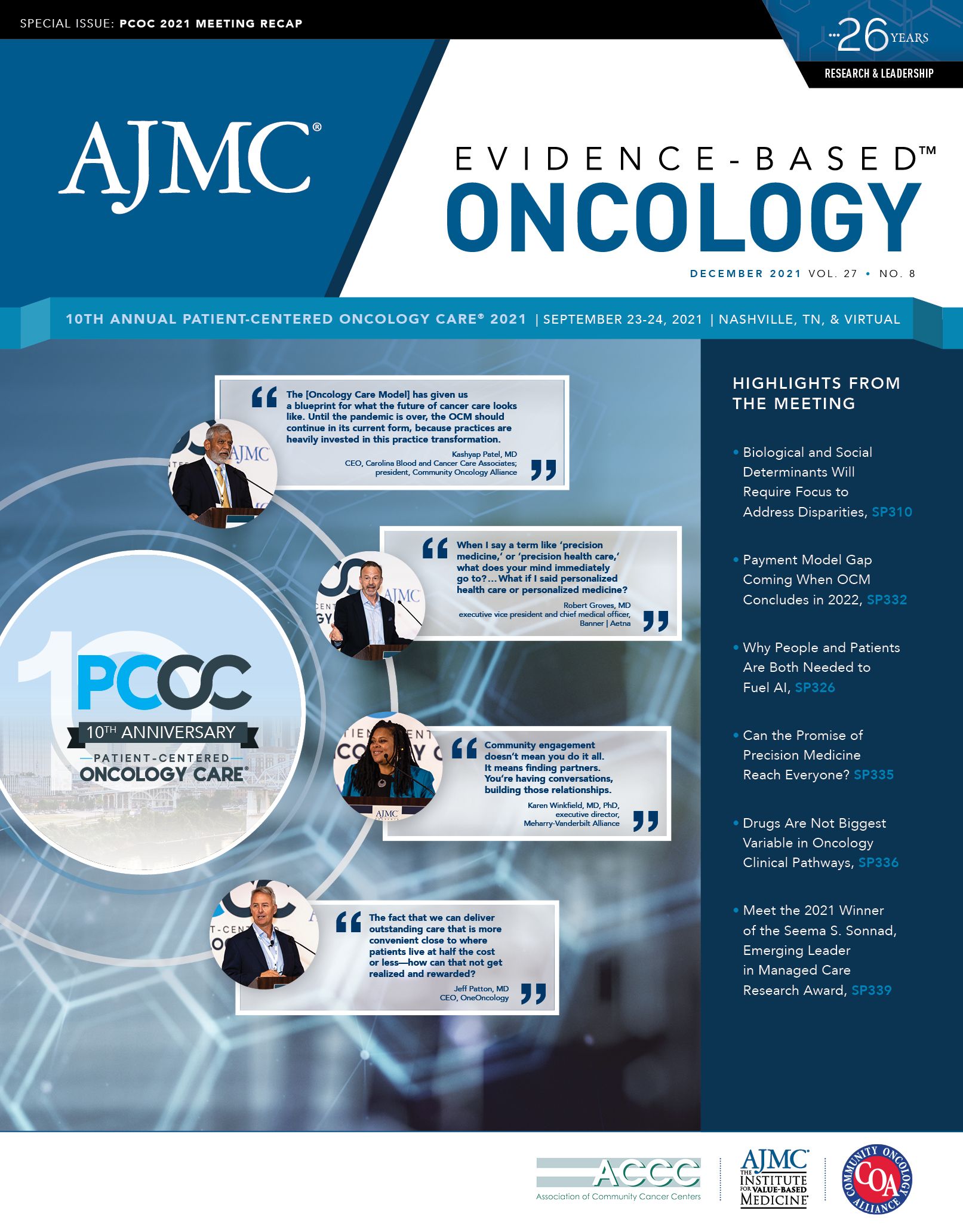
During the discussion on cancer care disparities at Patient-Centered Oncology Care®, Karen Winkfield, MD, PhD, executive director of the Meharry-Vanderbilt Alliance, asked John Carpten, PhD, of the Keck School
of Medicine at the University of Southern California Norris Comprehensive Cancer Center the following question: “If we are talking about getting the right treatment to the right patient at the right time, what are some of the
data points that we’re currently missing?
The answer, Carpten replied, starts with the basic concept of precision medicine itself. And this is broader than most people realize if one looks at the definition given by the National Institutes of Health (NIH), he said.
"I’m going to say this sensitively—it’s consistently dumbed down to performing a genetic assay and trying to understand how to manage disease based on the individual’s genetics," Carpten pointed out. "But if you
look at the NIH definition, it broadens it: it talks about lifestyle [and] environmental factors that can also [have] a significant impact on individual exposures."
These can include stresses, the built environment, and other factors that affect a person’s living condition, Carpten said, in addition to their genetic ancestry. This area, epigenetics, involves individual behaviors and external factors that can alter how genes work. Epigenetics plays a huge role in cancer because if these other factors are not taken into account, targeting a patient’s mutation won’t bring about the expected result.
"There are so many aspects of managing disease that go beyond just, 'There’s an alteration, it’s linked to this drug, so that drug should be effective in that setting.’ And we know that that’s not always the case because there are so many other things that can impact that individual’s response,' " Carpten said.
The future, he continued, should involve building cancer care models that would take both genetic and epigenetic factors into account. Winkfield used the example of smoking and how a mother’s smoking during pregnancy can affect multiple generations of a family.
“The more data we generate, the more we learn, and the more we can contribute to the model," Carpten said. "My hope is that it won’t be about one measurement, it will be about a model. And in order to develop those models, we have to perform the studies that generate the data."
An opportunity exists for trauma, poverty, and institutional racism, for example, to finally be factored into such a model. "I’m starting to be more vocal about the fact that racism is trauma, right? It’s generational trauma," said Winkfield.
According to Carpten, models are beginning to take structural racism into account, including how exposure to environmental and social stressors affected the rate of reactive oxygen species development. This, in turn, led to effects such as chronic inflammation that are known to increase cancer risk. For all his excitement over the possibilities of AI, Carpten offered a warning: disparities could be exacerbated if not everyone has access. We have to take it one step at a time," he said. "[but] I think we’ve made a lot
of progress."
ICYMI: Highlights From the 2022 American Academy of Dermatology Meeting
December 17th 2022This American Academy of Dermatology (AAD) Annual Meeting covered a breakthrough therapy for the management of vitiligo, clinical and epidemiological differences of certain dermatologic diseases, and the role of dietary triggers on patient outcomes.
Read More
Method of Tissue Acquisition May Determine Success of Gene Sequencing in Lung Cancer
July 7th 2022Successful comprehensive genomic profiling of tissue samples among patients with lung cancer was more likely to occur when samples were extracted via resections vs fluid cytology, biopsy, or fine-needle aspirations.
Read More
FOENIX Update: A New Era in Cholangiocarcinoma Precision Medicine
July 1st 2022Patients with iCCA, particularly those whose disease progresses following first-line chemotherapy, have limited overall treatment options. Data presented at the 2022 American Society of Clinical Oncology (ASCO) Annual Meeting show that patients may soon have a new agent to fight this rare cancer in futibatinib (Taiho Oncology), an FGFR inhibitor.
Read More
Lack of CGP Testing May Result in Missed Therapy Options in NSCLC
June 28th 2022A real-world analysis found that comprehensive genomic profiling (CGP) in patients with non–small cell lung cancer (NSCLC) increases their therapy options patients and CGP testing needs to be utilized more.
Read More
