- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
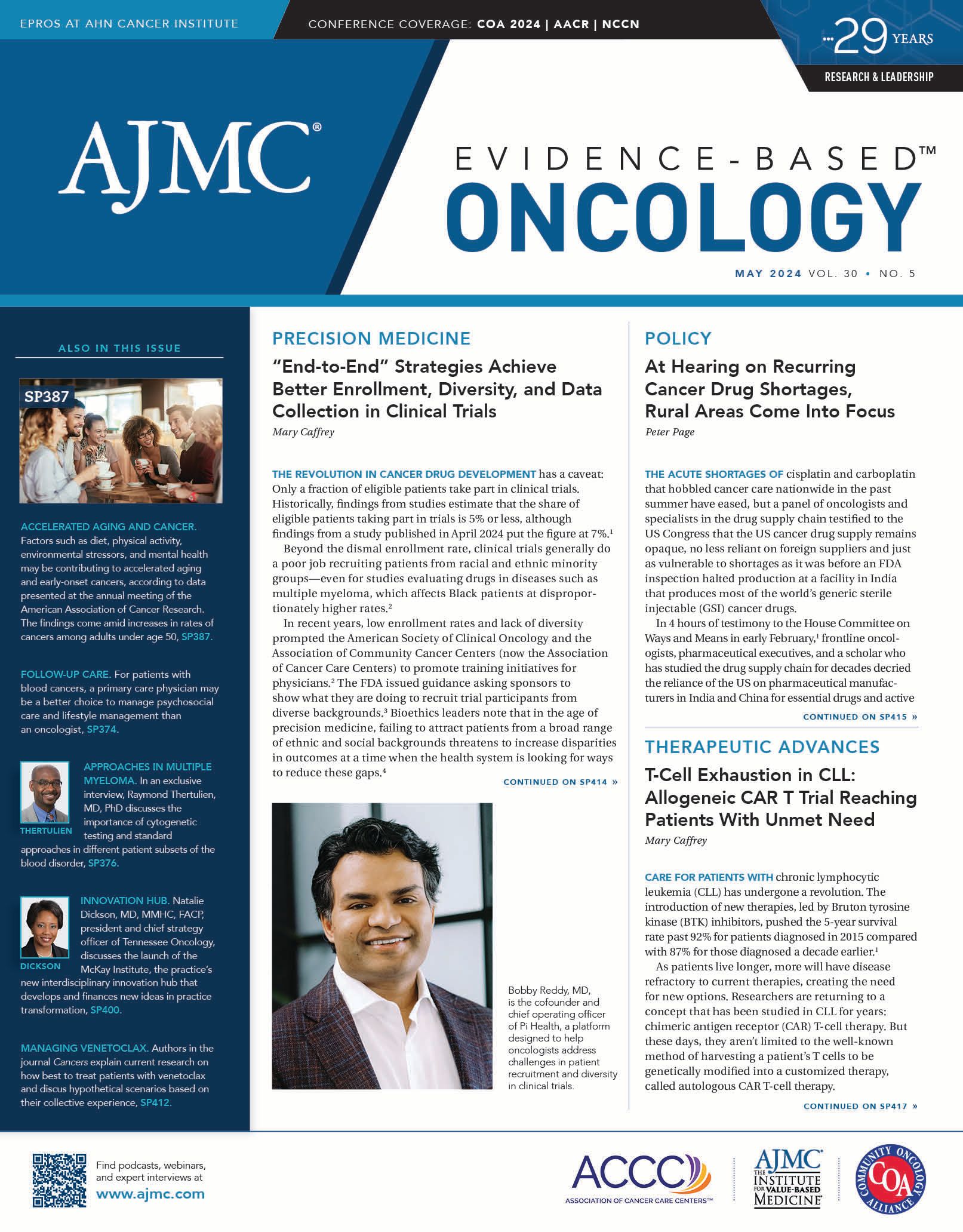
Kathy Oubre, MS, on Mitigating Challenges When Adopting New Payment Models
As oncology practices strive to deliver high-quality, cost-conscious care to patients, alternative payment models such as the CMS Innovation Center’s Enhancing Oncology Model (EOM) and models from commercial payers have been explored as avenues to encourage quality care.
Kathy Oubre, MS | Image credit: LinkedIn
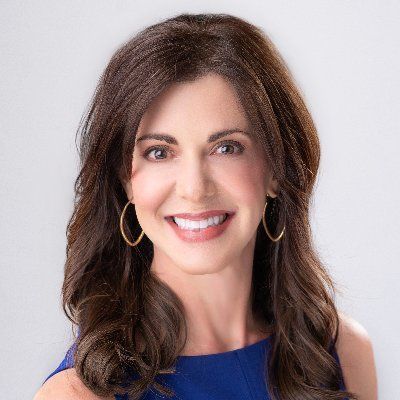
Although adopting new payment models can come with challenges, there are strategies that can help practices optimize their approaches, Kathy Oubre, MS, said in an interview with Evidence-Based Oncology (EBO). Oubre is CEO of Pontchartrain Cancer Center in Covington, Louisiana.
This interview is lightly edited for clarity.
EBO: What are some of the biggest challenges oncology practices face when adopting new payment models?
Oubre: I think the biggest challenge that practices face when bringing on a new payment model is getting everyone in the organization on board with that new model to understand the “why” and to understand the workflows and the value to the practice as well as the patients.
EBO: How are practices addressing the infrastructure and resource challenges associated with these new payment models?
Oubre: There are a lot of new strategies and innovations available in the cancer care space when thinking about value-based care. Practices need to think judiciously about that because there are small solutions for every facet of value-based care. But that’s a lot of technology to keep up with. We need to spend time figuring out what we can handle on a practice level with our resources and where we need to make partnerships so those facets of the value-based care model work better.
Some of the resource challenges [include] the finances behind all the different technologies that practices can take advantage of to help in value-based care. All of those things have a cost, which then eats into the overall cost, or margin, of a practice. So you have to be judicious in how you bring those things online. But there are some really good models out there.
For example, there’s some [well-designed] software that helps practices. We’ve been doing principal care management for the past year. We’ve been doing that within the EMR [electronic medical records], but it’s more of a paper process, or lack of an automated process. So we brought on a software vendor to help us automate it and make it more seamless within the organization. And we saw a tremendous uptake in our patients. We saw pretty good adoption as to the “why” and the understanding in our employees. And within probably a month of utilizing that vendor, we were able to turn that investment into a profit, which helps us, helps the patient, and helps the payer.
EBO: In your opinion, what roles do policy development and regulatory support play in ensuring the continued success and sustainability of alternative payment models?
Oubre: When we’re considering payment policies and regulatory issues around patients and patient care, we need to remember that 1 size does not fit all when we’re designing these models. We see that when looking at social determinants of health. We treat a wide variety of patients—we treat individuals with master’s degrees and those who have an eighth-grade education, those who are in the top 1% and those who need food bank assistance. So when we’re designing these models and how we think
things should work, be that OCM [Oncology Care Model] or EOM [Enhancing Oncology Model] or a commercial payer model, we need
to consider that there’s a large variability of patients we have to serve to fulfill our mission as a practice.