- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
“End-to-End” Strategies Achieve Better Enrollment, Diversity, and Data Collection in Clinical Trials
The revolution in cancer drug development has a caveat: Only a fraction of eligible patients take part in clinical trials. Historically, findings from studies estimate that the share of eligible patients taking part in trials is 5% or less, although findings from a study published in April 2024 put the figure at 7%.1
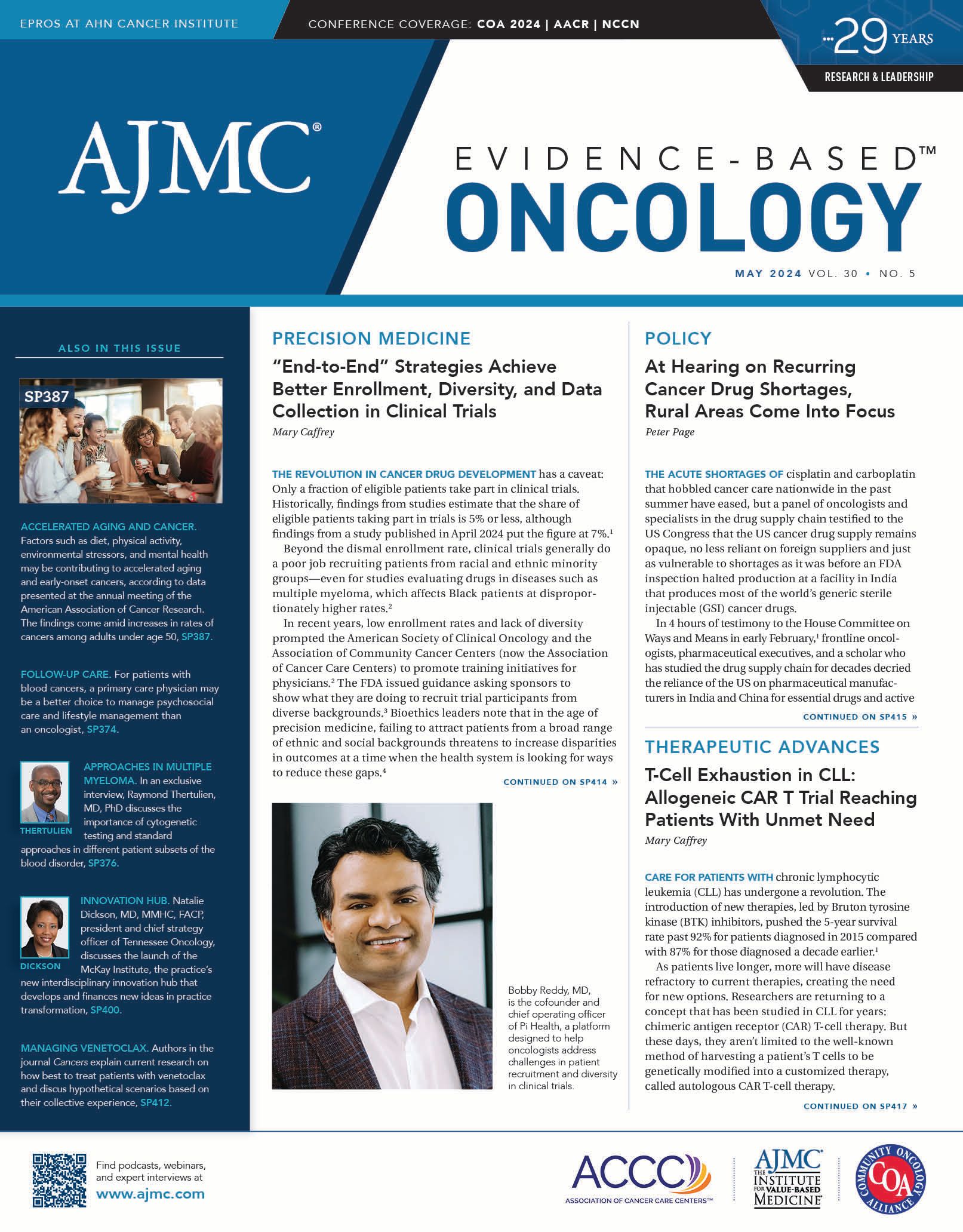
Bobby Reddy, MD | Image credit: Keri Tan

Beyond the dismal enrollment rate, clinical trials generally do a poor job recruiting patients from racial and ethnic minority groups—even for studies evaluating drugs in diseases such as multiple myeloma, which affects Black patients at disproportionately higher rates.2
In recent years, low enrollment rates and lack of diversity prompted the American Society of Clinical Oncology and the Association of Community Cancer Centers (now the Association of Cancer Care Centers) to promote training initiatives for physicians.2 The FDA issued guidance asking sponsors to show what they are doing to recruit trial participants from diverse backgrounds.3 Bioethics leaders note that in the age of precision medicine, failing to attract patients from a broad range of ethnic and social backgrounds threatens to increase disparities in outcomes at a time when the health system is looking for ways to reduce these gaps.4
Can AI Improve Trial Enrollment?
The rise of artificial intelligence (AI) has brought a host of companies offering solutions to these problems—some help physicians find trials that match their patients’ conditions, whereas others offer support from the patient side in finding a trial match.5
Pi Health, which secured $30 million in financing this spring following years of incubation within the pharmaceutical company BeiGene,6 purports to integrate functions that have been offered separately, addressing challenges of patient recruitment, diversity in enrollment, and integrity of data collection while also providing training for community investigators.
“At the very simple level, it’s a technology platform that can support drug development,” Bobby Reddy, MD, Pi Health cofounder and chief operating officer, said. In an interview with Evidence-Based Oncology, he said what differentiates the company is its position as an “end-to-end” solution for both drug sponsors and for health systems or oncology practices that want to take part in clinical trials.
Brenton Fargnoli, MD | Image credit: AlleyCorp

The company’s most immediate plans involve expanding its footprint in the United States and overseas, Reddy said. Pi Health’s lead investors were AlleyCorp and Obvious Ventures,7 and AlleyCorp’s Brenton Fargnoli, MD, a leader at Flatiron Health before its acquisition by Roche, offered an endorsement for the March 14, 2024, funding6 on “Pi Day.”
“Today’s clinical trials infrastructure is a maze of Excel spreadsheets, paper binders, and manual data entry into various point solutions,” Fargnoli said. “Many companies have tried to solve this clinical trials conundrum. None has taken the bold, comprehensive, and global approach that Pi Health has.”6
Access Is Key to Enrollment Diversity
Although giving sponsors the technology they need to complete a trial matters, Reddy said, “What happens at the health system setting is very important, because that is where we believe you can redefine how access works.”
Geoff Kim, MD | Image credit: Pi Health

Reddy’s inspiration for starting the company stems from his training as a physician-scientist in dermatologic oncology and his tenure as an attending physician at Massachusetts General Hospital in Boston. He witnessed the rapid development of new treatments for melanoma that made a clear impact on patient survival. Pi Health cofounder and CEO Geoff Kim, MD, helped approve many of those treatments as a division director in the Office of Hematology Oncology Products at the FDA.
However, Reddy said, “There was another problem that I thought was very significant. In spite of this incredible innovation, access wasn’t being addressed at the same pace.”
Patients could receive the latest treatments if they went “to Massachusetts General [Hospital] or [Memorial] Sloan Kettering [Cancer Center in New York, New York] or the other great academic and tertiary care centers in the world,” he said. “But if you go to community centers that can be 40 miles from here or if you go to other countries, you have a drastically different reality in what’s available, both in terms of innovative medicines and in clinical trials that are offering innovative medicines as part of clinical research.”
To address these gaps, Reddy explained, the platform offered by Pi Health focuses on barriers that can keep clinical trials from reaching community oncology locations:
Bringing efficiency to data collection. Pi Health’s software, known as Front-end Interoperable Capture System (FICS), captures and consolidates quality data at the beginning of the patient’s journey, which means drug sponsors won’t waste time later trying to fill in missing information (there are systems for sponsors and trial sites). As described by Fargnoli, FICS is designed to overcome processes that leave data spread across multiple systems or spreadsheets, with some held in written logs. In addition, Pi Health invests in educating community clinic personnel in data capture.
Reducing administrative burden. Health systems or community clinics outside academic centers may be reluctant to take on clinical trials because they lack the staff or knowledge to activate a trial or manage requirements. Pi Health offers online document management and training and invests in educating research coordinators. Asked how many hours this process takes, Reddy said it varies, depending on the existing level of integration of a clinic’s electronic health record and other factors.
Generating notes. Digitized document management includes automated notes, created with generative AI. “Physicians are relieved of the burden of having to spend time writing all the documents that are needed in both patient care and clinical research,” Reddy said. “Our motto has always been, ‘More face time, less waiting time.’ This means physicians and nurses can spend more time seeing patients rather than staring behind screens.”
“Community medical centers have challenges,” Reddy said. “They’re trying to provide care in a very rapidly changing treatment landscape. Often, this is too significant a barrier to get involved in clinical trials. What our technology does is simplify that process for these community settings; we make it easier to capture the kind of quality of data that regulatory agencies and pharmaceutical companies are looking for in drug development.”
Investing in Investigators
Beyond offering a user-friendly platform, Reddy said educating investigators in community settings makes a difference when these physicians engage patients in whether to take part in a clinical trial.
“We’ve created a scientific affairs capability in the company to help the physicians and investigators get more publications and bolster their [curricula vitae],” Reddy said. This is important to show pharmaceutical companies how much knowledge exists at the community level and help these physicians win opportunities to conduct trials.
In one case, Reddy said, “We deployed our technology in a community medical center that’s been active for 40 years—they’re loved in the community, but they didn’t do clinical trials.” There was interest in research among the center’s physicians, “but there was this perception [about] the administrative challenges and the lack of opportunities from the companies,” which kept the center from actively pursuing trials.
Pi Health worked with a nurse who spearheaded the effort to deploy their technology, and now the center is a clinical trial site. Patients in the area previously had to travel long distances to take part in trials, Reddy said, and now many will not have to do that.
If the FDA is asking sponsors to improve diversity in trial enrollment, will they help fund the cost of training community staff?
“That’s what we’re hoping for—and then the sponsor benefits too, because they want more patients; they want better quality of data,” Reddy said. In the long run, he said, this is a comparatively small investment for drug sponsors to achieve greater diversity in trial enrollment and reach more patients outside the tertiary care centers.
The only way to change who enrolls in clinical trials, he said, is to follow the patients.
“Honestly, the infrastructure that we currently have is just insufficient. If you want to do diverse trials, you need to be able to have trials where diverse populations are,” Reddy said. “And that has been a challenge.”
“The resounding theme is people do trials in the same places,” he continued. “There is a monopoly of trials in academic centers and large tertiary care centers, and they can do their best to recruit given the diversity that they have within their patient population. But a large part of diversity comes in community settings. So unless we find a way to bring clinical trials where the diverse patients are—and globally—that problem is not going to be solved.”
References
1. Unger JM, Schulman LN, Facktor MA, Nelson H, Fleury ME. National estimates of the participation of patients with cancer in clinical research studies based on Commission on Cancer accreditation data. J Clin Oncol. Published online April 2, 2024. doi:10.1200/JCO.23.01030
2. Oyer RA, Hurley P, Boehmer L, et al. Increasing racial and ethnic diversity in cancer clinical trials: an American Society of Clinical Oncology and Association of Community Cancer Centers joint research statement. J Clin Oncol. 2022;40(19):2163-2171. doi:10.1200/JCO.22.00754
3. Enhancing the diversity of clinical trial populations —eligibility criteria, enrollment practices, and trial designs guidance for industry. FDA. November 2020. Updated April 4, 2024. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/enhancing-diversity-clinical-trial-populations-eligibility-criteria-enrollment-practices-and-trial
4. Lee SSJ, Fullerton SM, McMahon CE, et al. Targeting representation: interpreting calls for diversity in precision medicine research. Yale J Biol Med. 2022;95(3):317-326.
5. Fultinavičiūtė U. It’s a match! connecting patients to clinical trials with AI. Clinical Trials Arena. May 18, 2023. Accessed March 27, 2024. https://www.clinicaltrialsarena.com/features/clinical-trial-matching-ai/
6. Pi Health raises over $30M in series A to revolutionize cancer care and clinical trials. News release. Pi Health. March 14, 2024. Accessed March 27, 2024. https://finance.yahoo.com/news/pi-health-raises-over-30m-141200260.html
7. Rai S. Doctors raise $30 million for cancer treatment AI startup. Bloomberg. March 14, 2024. Accessed March 27, 2024. https://www.bloomberg.com/news/articles/2024-03-14/doctors-raise-30-million-for-cancer-treatment-ai-startup