- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
FROM THE EDITOR IN CHIEF: Days of Future Past
If I had been asked in 2013 to predict what cancer care would look like in 10 years, I would have been wrong on too many levels to count. Therefore, I have little idea of what care will look like in 2033. If the past
Alvarnas

10 years offer any guide, I suspect that over the next decade, new therapeutic technologies based upon targets identified by genomic, transcriptomic, and proteomic identification or continued innovations in immunotherapy will play a more expansive role and that the portfolio of anti-cancer therapeutics will become even more complex and diverse. I suspect that as this happens, the issue of escalating care costs will continue to create additional divisive pressures among payers, physicians, and health care systems. Sadly, I also fear that gaps in cancer care access and disparities in patient outcomes, including those experienced by patients living in rural areas, may remain unresolved tragedies.
But that future has yet to be written. As clinicians, systems leaders, payers, and other key cancer care stakeholders, we are the ones best positioned to ensure that our future is one that bends toward greater fairness, compassion, and equity in care delivery and patient outcomes. Toward that end, we need to go beyond science to ensure that what we build evolves in ways that better humanize the care experience, that center value upon the needs of the patient, and that ensure the primacy of getting care to people who need it, when and where they need it. While we should not undervalue technological advances, we also should not place our blind faith in them as the solution to all the ills of our current system. Technological advances do not guarantee progress. That is our responsibility.
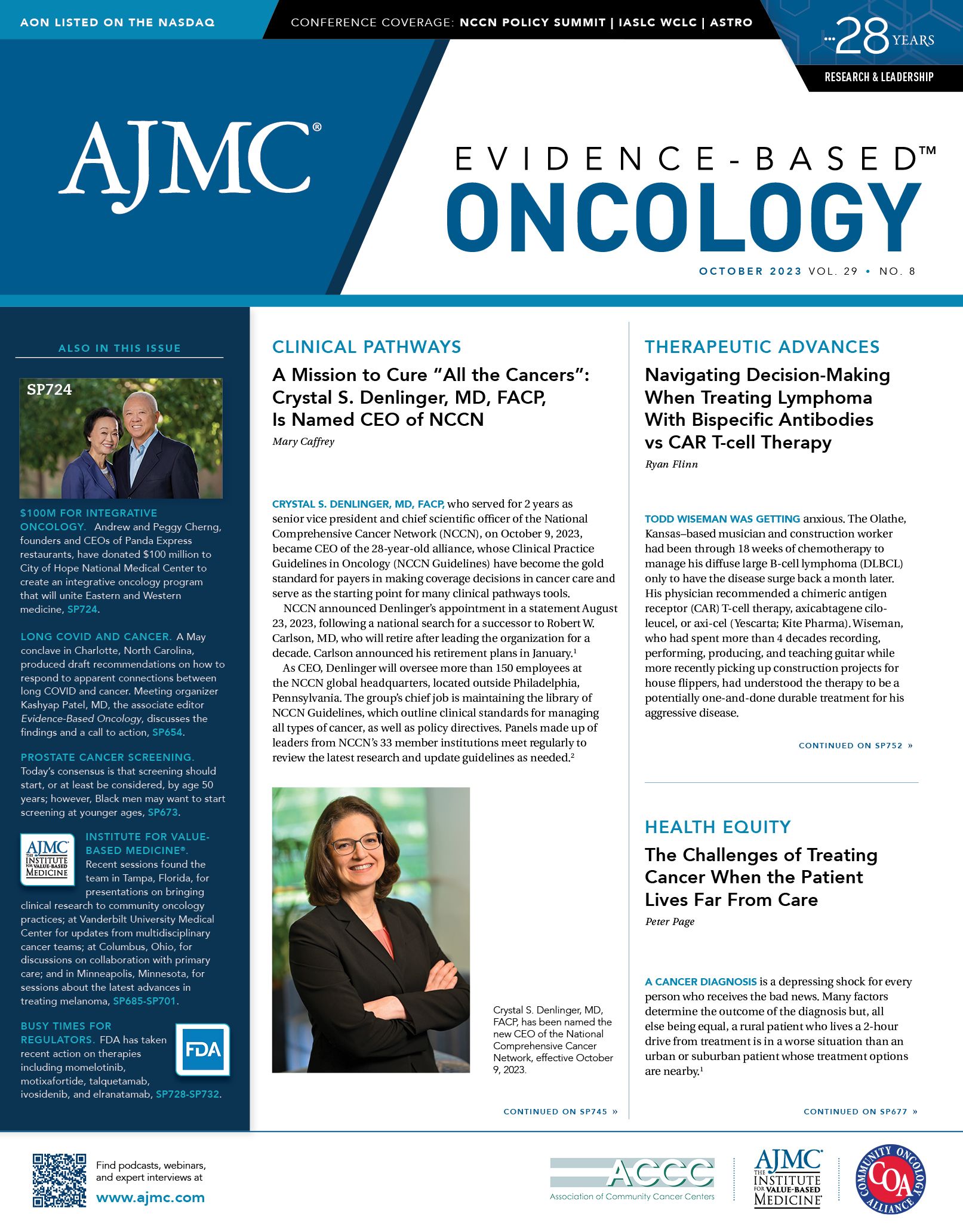
In this issue of Evidence-Based Oncology, we take a look at what this future and the path toward it could look like. Dale Porter, PhD, describes the advantages of the “fail fast/fail forward” model for drug discovery. In a perspective piece, the incoming CEO for the National Comprehensive Cancer Network, Crystal S. Denlinger, MD, FACP, charts out a mission to cure all cancers. In his coverage on the challenges of treating cancer when the patient lives far from care, Peter Page looks at some potential creative solutions for traversing the limits of geography when seeking the best care available.
Snoop Dogg noted, “You’ve got to always go back in time if you want to move forward.” While patients today benefit from a wealth of therapeutic possibilities that did not exist 10 years ago, there is still much need that cannot be met by just sticking to what worked in the past. Moreover, we need to embrace the idea that prior success does not absolve us of the need to actively shape our future. Our systems need to become better at enhancing the quality, effectiveness, and humanity of care. As we look at the failures of the past, we need to accept that technology alone will not fix problems that persist. I suspect that our best path forward entails working outside of our clinic rooms or hospitals in ways that culminate in the creation of more patient-centered care delivery models; in the development of public policy and legislation that puts the focus back upon patients and their families; and in the creation of deeper collaborations across the oncology stakeholder continuum to traverse barriers to care equity.
Impact of Amivantamab-Lazertinib on EGFR, MET Resistance Alterations in NSCLC: Danny Nguyen, MD
September 15th 2025The combination of amivantamab and lazertinib in first-line non–small cell lung cancer (NSCLC) significantly reduces resistance mechanisms with implications for second-line treatment, said Danny Nguyen, MD, of City of Hope.
Read More
