- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Data Back Neoadjuvant Combo vs Chemo Alone for Early-Stage NSCLC
For patients with early-stage non–small cell lung cancer (NSCLC), combining neoadjuvant immune checkpoint inhibitors and platinum-based chemotherapy improves 2-year outcomes over chemotherapy alone, suggest findings of an extensive literature review and meta-analysis.
Treatment with neoadjuvant immune checkpoint inhibitors (ICIs) plus platinum-based chemotherapy has significant benefit vs chemotherapy alone in patients with early-stage non–small cell lung cancer (NSCLC), according to new study results published in JAMA Network Open.
A literature search from January 1, 2008, through November 1, 2023, resulted in 8 phase 2 or 3 RCTs with neoadjuvant ICI-chemotherapy (with or without adjuvant ICIs) vs neoadjuvant chemotherapy alone, with or without placebo or observation. This systematic review and meta-analysis covered 3387 patients, all of whom had untreated stage IB to IIIB NSCLC.
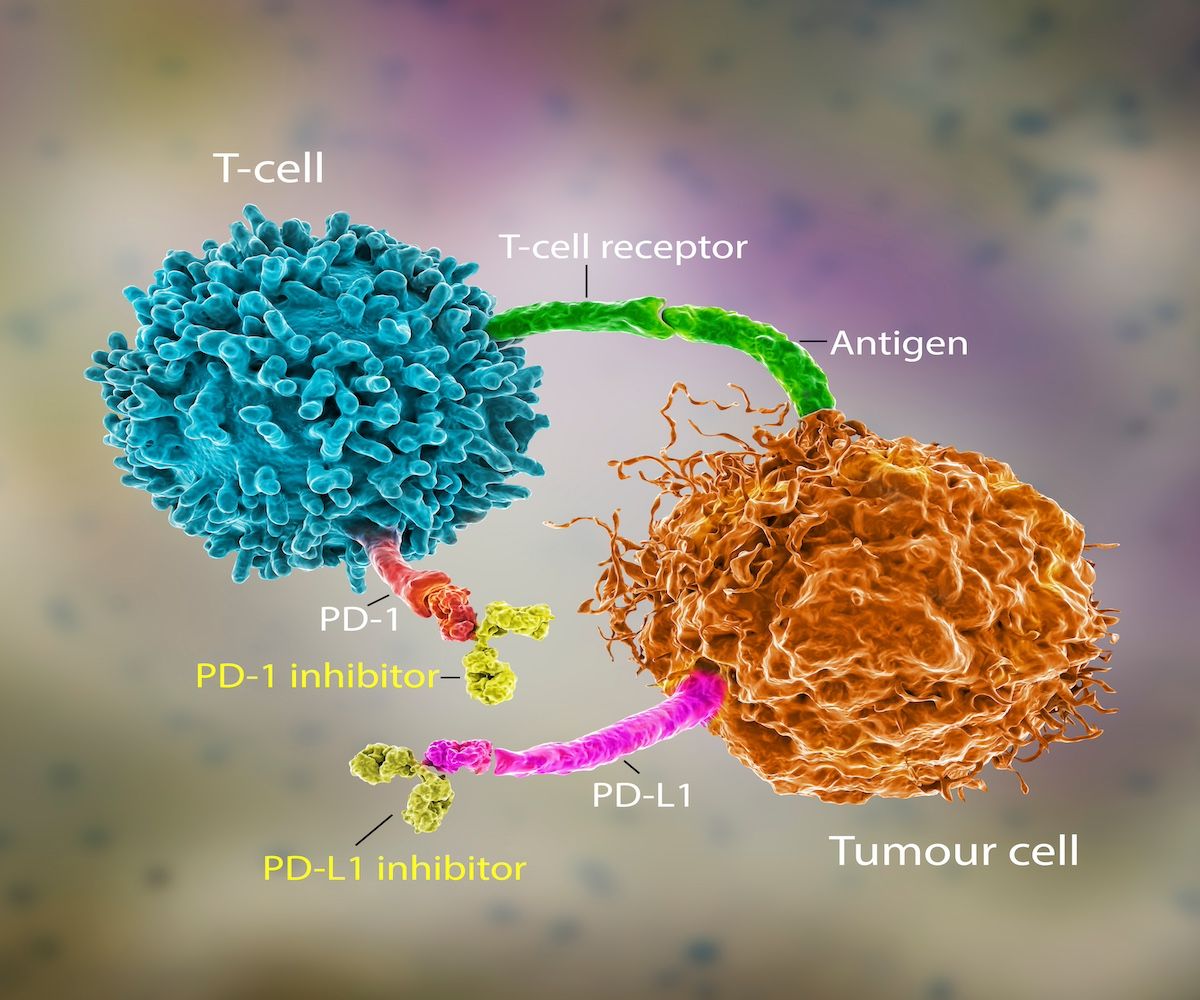
The combination improved both 2-year event-free survival (EFS) and pathologic complete response (pCR), the outcomes of interest, said the review’s authors. Also, the association between the combination’s use and these improved outcomes “was not significantly modified by the main patient characteristics or tumor- or treatment-related factors, including high or low tumor PD-L1 status.”
Neoadjuvant ICIs can improve the surgical resectability of tumors and decrease the risk of distant relapse, the researchers reminded.
A magnified image of immune checkpoint inhibitors at work against cancer | Image Credit: Dr_microbe -stock.adobe.com
They used a random-effects model for the meta-analysis, which followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guideline. They then calculated aggregated pooled HRs for time-to-event outcomes (ie, 2-year EFS) and risk ratios (RRs) for dichotomous outcomes (ie, pCR) with their respective 95% CIs.
The authors’ findings were considered statistically significant. Neoadjuvant ICI-chemotherapy was associated with both improved 2-year EFS (HR, 0.57; 95% CI, 0.50-0.66;P < .001) and increased pCR rate (RR, 5.58; 95% CI, 4.27-7.29;P < .001) in the experimental vs control treatment arms.
Type of platinum-compound chemotherapy, the number of cycles of neoadjuvant ICI-chemotherapy, and the addition of adjuvant ICIs didn’t significantly affect the outcomes.
The HRs varied in some subgroups. For instance, patients with stage III disease had numerically better HRs and 95% CIs for 2-year EFS than those with stage IB-II disease. Also, patients whose tumor cells were negative for PD-L1 were at higher risk of relapse (HR, 0.75; 95% CI, 0.62-0.91) than were those with low (HR, 0.61; 95% CI, 0.37-0.71) or high PD-L1 (HR, 0.40; 95% CI, 0.27-0.58) (P = .005).
The authors noted there was variability in how 2-year EFS and pCR were assessed across the 8 RCTs included in their review. “[This] must be acknowledged, as it was [among] the main determinants of the concern for the risk of bias derived by the relative qualitative assessment, and should inform the design of future clinical trials in the perioperative setting,” they recommended.
Further, “when surgery is an expected outcome in tumors deemed resectable before the study treatment is given, EFS should specifically also include the time to the point when tumors are considered unresectable alongside disease progression or recurrence that prevents patients from receiving surgery.”
Research to improve patient outcomes needs to continue. For instance, “promising biomarkers for future escalation or de-escalation of therapy, such as quantitative and qualitative assessment of circulating tumor DNA, or trials of new combinations with neoadjuvant or perioperative ICIs, could be used to avoid unnecessary toxic effects and costs,” the authors noted.
In the meantime, patients could also be spared some potential overtreatment if 2 other study findings are considered by providers: Adjuvant ICIs with or without chemotherapy might not be necessary in unselected patients, and 3 cycles of neoadjuvant ICIs with or without chemotherapy may be preferable to 4 cycles.
Reference
Banna GL, Hassan MA, Signori A, et al. Neoadjuvant chemo-immunotherapy for early-stage non–small cell lung cancer:a systematic review and meta-analysis.JAMA Netw Open. 2024;7(4):e246837. doi:10.1001/jamanetworkopen.2024.6837
