- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
CAR T-Cell Therapies, Bispecific Antibodies Usher in New Era in R/R MCL
Chimeric antigen receptor T-cell therapies, along with bispecific antibodies, have changed the treatment paradigm for patients with relapsed or refractory mantle cell lymphoma.
Both chimeric antigen receptor (CAR) T-cell therapies and bispecific antibodies (BsAbs) have important—and complementary—roles to play in the treatment of relapsed or refractory (R/R) mantle cell lymphoma (MCL), according to a new review article. The challenge, the authors say, is figuring out best to leverage the new therapeutic options to provide optimal personalized care.
The report was published in the European Journal of Hematology.1
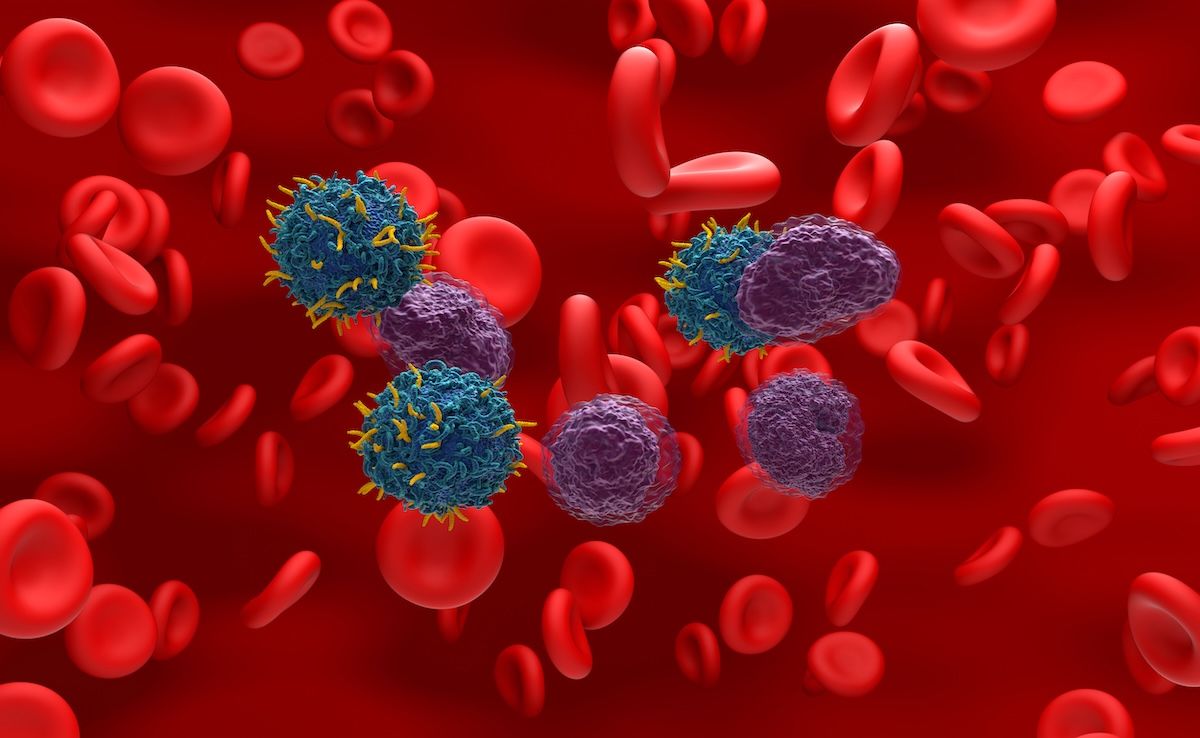
Sequencing decisions must be highly individualized in the era of immunotherapy for MCL. | Image credit: LASZLO - stock.adobe.com
Corresponding author Massimo Gentile, MD, of Italy’s University of Calabria, and colleagues, noted that MCL was historically considered incurable, and thus for a long time the goals of treatment were symptom control and prolonging survival.
They noted that patient prognosis is based upon several factors, including age, performance status, serum LDH, and leukocyte count. In younger, fit patients, the treatment paradigm traditionally consisted of intensive chemoimmunotherapy followed by autologous stem cell transplantation (ASCT) consolidation and sometimes rituximab (Rituxan) maintenance, they said. However, the investigators said the TRIANGLE study found that the integration of Bruton tyrosine kinase (BTK) inhibitors in the initial treatment algorithm can make it possible to achieve durable remissions without the need for ASCT.2
“Additionally, early exposure to BTK inhibitors enables prompt identification of patients who are refractory or relapse rapidly, facilitating timely transition to alternative therapies or enrolment in clinical trials,” they wrote.1
BTK inhibitors have also become the preferred second-line option for patients with relapsed or refractory disease, they noted.
Still, they said the only potentially curative option for MCL is allogeneic hematopoietic stem cell transplantation (allo-HSCT), though its use is usually reserved for younger, fit patients.
However, Gentile and colleagues said T-cell-redirecting immunotherapies have the potential to lead to important shifts in treatment. They said CAR T-cell therapies have led to high overall response rates (ORRs) and durable remissions, even in patients who are heavily pretreated or BTK inhibitor-refractory. For instance, brexucabtagene autoleucel (Tecartus), the first CAR-T therapy approved for R/R MCL, achieved an ORR of 93% and a complete response (CR) rate of 67% in a primary efficacy analysis, Genitle and colleagues said.
Yet, the investigators added that CAR T is also associated with a significant risk of severe toxicities like cytokine release syndrome (CRS) and immune effector cell-associated neurotoxicity syndrome (ICANS). Beyond that, the individualized therapy has a highly complex and costly manufacturing process, often necessitating the need for bridging therapy.
BsAbs, which can be engineered to target CD20 on lymphoma cells and CD3 on T lymphocytes, do not have the same logistical challenges as CAR T-cell therapies, the authors noted, and their toxicities are generally manageable with the use of strategies such as step-up dosing, corticosteroids and anti-interleukin 6 therapy, along with careful patient monitoring.
“Clinical data indicate that BsAbs are active in both CAR T–naive and post–CAR T settings, providing disease control in patients ineligible for immediate CAR-T therapy,” they explained.
All of this, however, creates an urgent need to better understand the best sequence and combination of therapies, the authors said.
“BsAbs can induce meaningful responses in patients relapsing after CAR T-cell therapy, and conversely, CAR-T can be effective following BsAb exposure, although prior CAR-T may impact T-cell fitness and the depth of subsequent response,” they noted.
Gentile and colleagues also noted, however, that preclinical studies suggest continuous stimulation of T cells with BsAbs can induce T-cell exhaustion, a finding they said underscores the importance of thoughtful immunotherapy sequencing.
They said possible future sequencing strategies could potentially involve using CAR T-cell therapy as consolidation following BsAb-induced remission or using BsAbs after a patient relapses from CAR T-cell therapy. However, they said any sequencing decisions need to be highly individualized.
“Optimal sequencing and combinatorial strategies, individualized to disease biology and patient characteristics, represent the next frontier for improving outcomes in this historically challenging disease,” they concluded.
References
- Caserta S, Martino EA, Vigna E, et al. T-cell-redirecting immunotherapies in relapsed/refractory mantle cell lymphoma: current evidence, sequencing, and future directions. Eur J Haematol. Published online November 9, 2025. doi:10.1111/ejh.70063
- Dreyling M, Doorduijn J, Giné E, et al. Ibrutinib combined with immunochemotherapy with or without autologous stem-cell transplantation versus immunochemotherapy and autologous stem-cell transplantation in previously untreated patients with mantle cell lymphoma (TRIANGLE): a three-arm, randomised, open-label, phase 3 superiority trial of the European Mantle Cell Lymphoma Network. Lancet. 2024;403(10441):2293-2306. doi:10.1016/S0140-6736(24)00184-3
Specialty and Operator Status Influence Electronic Health Record Use Variation
January 22nd 2026Operators demonstrated specialty-specific differences in electronic health record efficiency, timeliness, and after-hours use, highlighting how workflow and training shape documentation behaviors across medical disciplines.
Read More
