- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
BET Inhibition Reduces CLL Burden, Boosts Immune Function
BET inhibition in chronic lymphocytic leukemia (CLL) significantly reduces leukemic cell burden and restores T-cell function by modulating the immune microenvironment and reversing T-cell exhaustion.
Findings from a new study, published in JCI Insight, demonstrate that inhibiting bromodomain and extra-terminal (BET) protein OPN-51107 (OPN5) in chronic lymphocytic leukemia (CLL) reduces leukemic cell burden and restores T-cell functions by decreasing immune inhibitory receptor (IR) expression and enhancing cytokine production. The research also suggests a reversal of T-cell exhaustion, indicated by changes in gene expression and chromatin accessibility.1
The study findings demonstrate that OPN5 treatment significantly reduces the presence of leukemic cells in the peripheral blood of CLL models. Mice treated with OPN5 for 21 days showed a decrease in CD19+/CD5+ peripheral blood lymphocytes (PBLs) from 71.8% in the control group to just 11.2% in the OPN5-treated group.
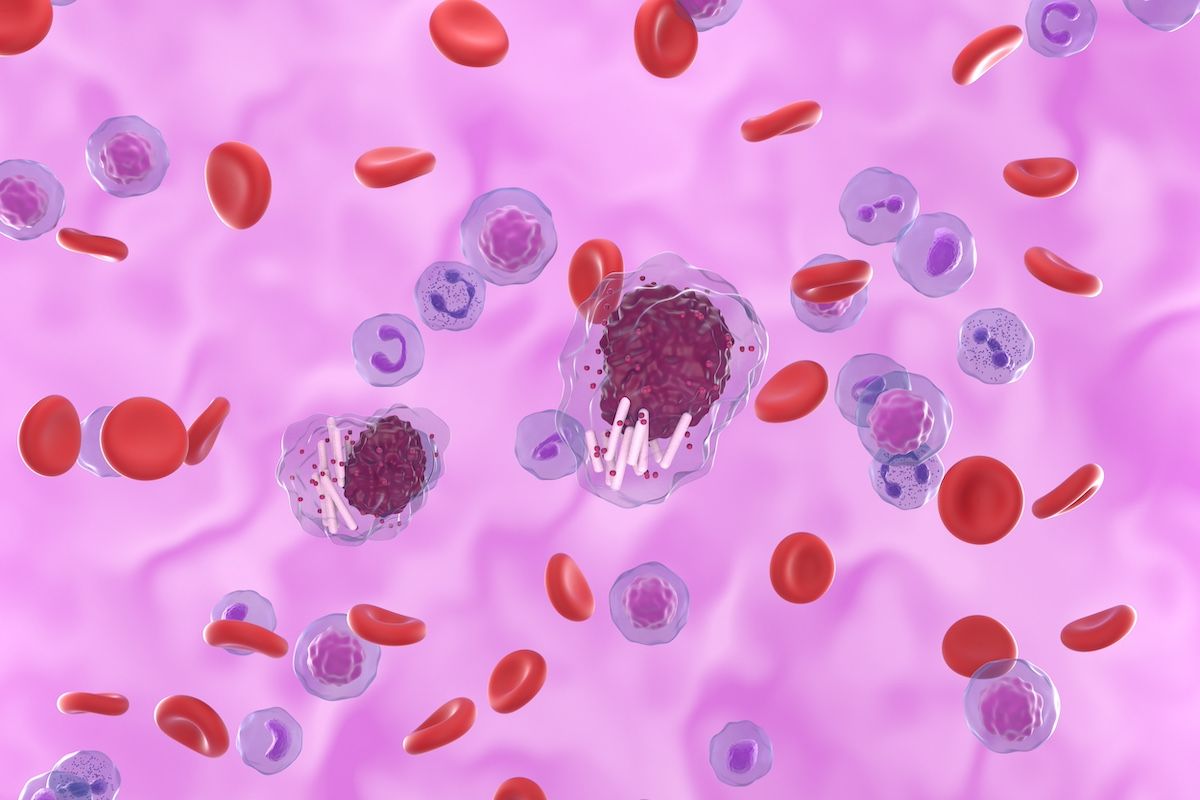
The authors of this analysis concluded that BET inhibition may be most effective as part of a treatment combination | Image Credit: LASZLO - stock.adobe.com
The study involved 2 key adoptive transfer (AT) experiments using the Eμ-TCL1 mouse model of CLL. These experiments aimed to investigate the effects of BET inhibition on the CLL redundant tumor microenvironment and immune dysfunction. In the first AT study, conducted over 21 days, OPN5-treated mice exhibited a significant reduction in disease burden in the peripheral blood, with leukemic cells (CD19+/CD5+ PBLs) decreasing from 71.8% in the vehicle-treated group to 11.2% in the OPN5-treated group. Analysis of splenic tissue and peripheral blood mononuclear cells revealed differentially expressed genes (DEGs). Notably, the splenic B-cell score decreased, while the relative scores for cytotoxic, natural killer, and type 1 T helper cells increased. Gene set enrichment analysis showed modulation of immune signatures, including interleukin (IL)-2, IL-2RB, interferon-γ, T-cell receptor (TCR) signaling, CD8+ TCR, T-cell activation, and transcriptional regulation by RUNX3 pathways.
The second AT study, conducted over 28 days, assessed the function and differentiation status of splenic T cells from OPN5-treated mice. After 28 days, OPN5-treated mice displayed significantly less disease in the peripheral blood, with leukemic cells (CD19+/CD5+ PBLs) decreasing from 38.3% in the vehicle-treated group to 11.6% in the OPN5-treated group. Spleens from OPN5-treated mice harbored markedly smaller proportions of CLL B cells and greater proportions of T cells. In addition, CD8+ T cells from OPN5-treated mice showed enhanced T-cell proliferation indices and increased cytokine production, including elevated levels of IL-2 and dual expression of IFN-γ and tumor necrosis factor-α.
Leukemic B cells from OPN5-treated mice were less proliferative and showed reduced expression of PD-L1 and V-domain Ig suppressor of T-cell activation (VISTA). Both CD4+ and CD8+ T cells from OPN5-treated mice demonstrated greater ex vivo proliferative capacity and increased cytokine production.
T cells from OPN5-treated mice expressed significantly fewer IRs, including PD-1, CD160, CD244, LAG3, and VISTA. This reduction was observed across various T-cell subsets,
The study identified 244 DEGs in the spleens of OPN5-treated mice. Findings include the upregulation of genes associated with T-cell activation, such as Cd3e, Cd8a, and inducible T-cell costimulator ligand (ICOSL). Conversely, genes involved in T-cell suppression, like Ctla4 and Cd274 (PD-L1), were downregulated.
BET proteins are known to influence chromatin structure.2 Chromatin accessibility analysis using ATAC sequencing revealed that OPN5 treatment also led to changes in chromatin accessibility. Genes involved in T-cell activation, such as TCF7 and CXCR5, showed increased accessibility, while those associated with terminal exhaustion, including CD101 and BATF3, displayed reduced accessibility.
The authors point out that although both OPN5 and chemotherapy treatments, such as fludarabine, reduce leukemic B-cell burden, only BET inhibition with OPN5 alleviated T-cell dysfunction in vivo, enriched for naïve CD5+ T cells, reduced IR expression, and altered the transcription factor profile of splenic CD8+ cells.
"Despite impressive single-agent activity in CLL, BET [inhibition] may be most effective in combinatory treatment regimens. Preclinical studies have shown that BET [inhibition] synergizes with other small molecule inhibitors, such as venetoclax and [ibrutinib], in B-cell non-Hodgkin lymphoma," the authors concluded.
References
1. Smith AL, Skupa SA, Eiken AP, et al. BET inhibition reforms the immune microenvironment and alleviates T cell dysfunction in chronic lymphocytic leukemia. JCI Insight. Published online May 22, 2024. doi:10.1172/jci.insight.177054
2. Cheung KL, Kim C, Zhou MM. The functions of BET proteins in gene transcription of biology and diseases. Front Mol Biosci. Published online September 3, 2021. doi:10.3389/fmolb.2021.728777
