- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
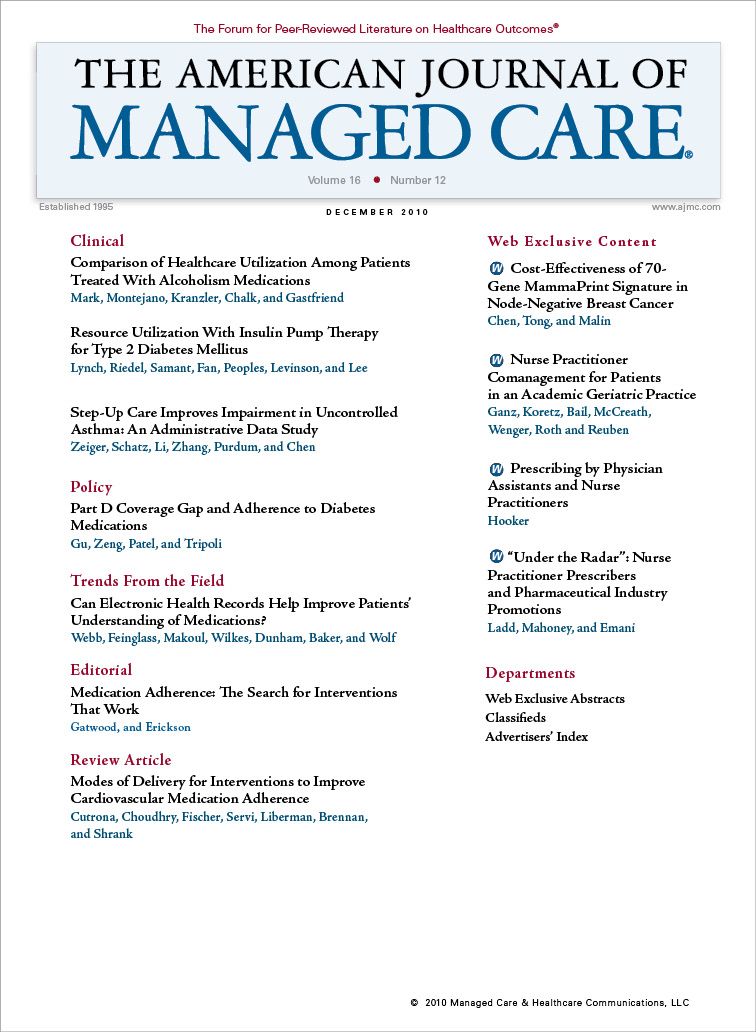
Nurse Practitioner Comanagement for Patients in an Academic Geriatric Practice
Nurse practitioner comanagment improved quality of care for 5 chronic conditions in an academic geriatrics practice.
Objective:
To determine whether nurse practitioner (NP) comanagement can improve the quality of care for 5 chronic conditions in an academic geriatrics practice.
Study Design and Methods:
From September 2006 to September 2007, 18 primary care geriatricians were divided into an intervention group that could refer patients to an NP for comanagement of dementia, depression, falls, heart failure, and/or urinary incontinence, or a control group that indicated which patients would have been referred to the NP for these conditions. The NP used structured visit notes to guide care delivery for the 5 conditions concordant with Assessing Care of Vulnerable Elders-3 (ACOVE-3) quality indicators. We reviewed charts to determine adherence to recommended processes of care.
Results:
A total of 200 patients (108 intervention, 92 control) were eligible for at least 1 process of care recommended by ACOVE-3 for the 5 conditions. Patients' mean (SD) age was 85 years (7 years), 67% were women, and patients were eligible for a mean (SD) of 6.9 (4.4) processes of care. Intervention patients were eligible for more care processes than controls (7.8 vs 5.9 processes per patient; P = .002). Quality of care was higher for patients in the intervention group compared with the control group (54% vs 34% of care processes completed; P <.001). The adjusted absolute difference between intervention and control groups in care processes completed was 20% (95% confidence interval = 13%, 27%).
Conclusion:
NP comanagement of 5 chronic conditions was associated with higher quality of care, even in a practice of geriatricians.
(Am J Manag Care. 2010;16(12):e343-e355)
A nurse practitioner markedly improved the quality of care for dementia, depression, falls, heart failure, and urinary incontinence in an academic geriatrics practice.
- Adding a nurse practitioner focused on managing these 5 chronic conditions improved adherence to recommended geriatric care by 20% in a setting where all physician providers were geriatricians.
- Improved quality of care came at the expense of 2.6 additional visits to the nurse practitioner per patient during a 13-month period.
The United States needs a more robust primary care system, yet fewer medical students are pursuing careers in primary care.1,2 This quandary, coupled with the need for interprofessional collaboration to care effectively for older adults,3 has renewed interest in care models that maintain the primary care physician (PCP) as the key decision maker with patients, but involve others in care implementation, including registered nurses with additional training (eg, nurse practitioners [NPs]), social workers, and physician assistants.4,5 Data suggest that NPs focused on a particular condition can provide at least comparable quality of care for that condition and sometimes achieve better patient outcomes.6,7 However, informationis sparse regarding the effectiveness of NP comanagement of complex older patients in outpatient settings. An NP/social worker team collaborating with PCPs and a geriatrician-led interdisciplinary team improved the quality of medical care for low-income seniors,8 and a trial of a registered nurse working with teams of PCPs to improve care for older adults with multimorbidity has shown an early beneficial effect on quality.9 In addition, specialized nurses, NPs, or psychologists have successfully comanaged patients with depression or dementia in primary care.10,11
Available studies do not, however, address whether NP comanagement can improve quality in a primary care practice staffed by geriatricians. By virtue of their training, interest, and patient population served, geriatricians are likely to be expert in managing geriatric conditions. Yet many of the barriers to providing recommended care that affect all PCPs (eg, lack of time during the office visit, inability to overcome existing practice habits)12 also confront geriatricians. This study’s goal was to evaluate a quality improvement program that compared usual primary care by academic geriatricians with care comanaged by an NP for 5 chronic conditions: dementia, depression, falls, heart failure, and urinary incontinence.
METHODS
Table 1
The quality improvement project ran from July 1, 2006, to September 30, 2007. Subsequently, University of California, Los Angeles Institutional Review Board approval was obtained to examine de-identified data. contains a description of the project setting.
Intervention
The project consisted of run-in (July 1, 2006 to August 30, 2006) and intervention (September 1, 2006 to September 30, 2007) periods. For these periods, an experienced, gerontology-certified NP (JKB), who was hired specifically for the comanagement role, was supported by a grant from the John A. Hartford Foundation. The NP was colocated with the geriatricians at the large outpatient clinic (see Table 1 for details on practice locations).
During the run-in period, the NP customized condition-specific structured visit notes based on previous versions13 to address the Assessing Care of Vulnerable Elders-3 (ACOVE-3) quality indicators for the 5 chronic conditions14-18 and American College of Cardiology/American Heart Association heart failure guidelines.19 These note templates were designed to support Medicare documentation requirements and could be used for both initial and follow-up visits. The run-in period also allowed time for the NP to develop her practice style, familiarize herself with clinic operations, and build trust among the referring physicians while seeing patients together with her supervisor (BKK). The practice also developed condition-specific patient education handouts (based on published materials20 and other materials21) and referrals to local community resources, most of which were available to both intervention and control physicians.
Before the intervention period, physicians were first paired by patient volume; then 1 physician from each pair was selected by coin toss to be able to refer to the NP. Intervention physicians could refer only their primary care patients, not other physicians’ patients whom they might have seen while covering. Control physicians could not refer patients to the NP but were requested to indicate which patients they would have referred.
During the intervention period, the night before a physician’s scheduled clinic, practice staff clipped an additional sheet to each patient’s chart. Control physicians were asked to note which (if any) of the 5 conditions would have prompted referral of the patient for NP comanagement and the priority level for each “referred” condition (more than 1 condition could have the same priority level). Intervention physicians were asked to note whether they would like the patient to see the NP for any of the 5 conditions and the priority level for each referred condition. The clinic scheduler received completed forms and, in the case of intervention patients, arranged an appointment with the NP. The NP could order tests and treatments without approval from the patient’s geriatrician, but could obtain guidance if needed. The NP delegated certain tasks to clinic nurses, including orthostatic vital signs, urinalyses, bladder scans, and visual acuity measurement. Patient follow-up visits were scheduled by the NP as needed. After each visit, the NP e-mailed or faxed geriatricians a written assessment and plan; she handled more urgent issues via phone or pager.
The project was introduced at a faculty meeting in September 2006, with follow-up by BKK (the clinical champion) to reinforce the importance of referrals. In February 2007, one pair of high-volume physicians switched roles, with the intervention physician switching to the control group and vice versa, because the physician originally assigned to the intervention group was not referring patients to the NP. This switch was made to increase the number of NP referrals.
For participating intervention and control physicians who were internists, the practice successfully applied to the American Board of Internal Medicine to receive credit for the Practice Improvement Module of the Maintenance of Certification program on the basis of this project. After the project period, all geriatricians could make referrals to the NP.
Data
Appendix A
After project completion, 2 abstractors, who had worked as physicians outside the United States, were trained by a nurse researcher with extensive experience in chart abstraction (CPR). Abstractors reviewed both the paper and electronic medical record using structured forms. All intervention and a sample of control group records were reviewed (see for details on control group selection).
Appendix B
The chart abstraction focused on determining eligibility for, and completion of, care processes specified by relevant ACOVE-3 quality indicators for vulnerable elders, the population served by the practice (see for indicator list). The quality indicators specify a time window during which relevant care should be completed; if this window extended beyond the end of the project period for a particular indicator, the patient was considered ineligible for that indicator. The abstractors’ decision about completion of recommended processes of care was based on the entire chart, regardless of who completed the care process or for which conditions the patient was referred to the NP. Thus, the care reviewed for patients in the intervention group was a compriorbination of both physician and NP care, and included project conditions that physicians had chosen not to refer to the NP. Abstractors were not blind to intervention versus control group status (because structured visit notes appeared only in intervention patients’ records) but were blind to which conditions patients were referred for.
Fifteen charts were reabstracted (8 for test-retest reliability and 7 for inter-rater reliability), demonstrating a pooled kappa22 of 0.64 for agreement on eligibility for care processes and (where agreement existed on eligibility) 0.31 for completion of care processes. Data from the paper abstraction forms were entered electronically (with more than 99% accuracy). Abstractors also reviewed encounter data in the electronic health record to determine the number of geriatrician and NP office visits in the intervention and control groups.
Data Analysis
Appendix C
Patient demographics were limited to information in the chart, which included age and sex. Patients were assigned to the intervention or control group based on the group status of their primary geriatrician. For the 2 physicians who switched intervention/control group status during the project, analysis was based on actual referrals (intervention or control) at the time of referral rather than intention to treat. Adherence to each recommended care process was scored dichotomously (process completed/not completed). The percent adherence was computed for the intervention and control groups, both in aggregate and stratified by condition. The primary analysis included all of the patient’s conditions. In a sensitivity analysis, we included only those conditions designated as “top priority” for referral to the NP on the referral sheets. Details on statistical analyses may be found in .
RESULTS
Charts from 275 patients (139 intervention, 136 control) were reviewed. For 2 patients, no record was found of any geriatric outpatient care; these patients were excluded. Of the remaining 273 patients, 200 (73%, 108 intervention, 92 control) were eligible for at least 1 ACOVE-3 process of care; these patients were eligible for a total of 1384 care processes (mean of 6.9 processes per patient [SD 4.4 processes]). Patients’ mean age was 85 years (SD 7 years); 67% were women. Age and sex did not differ by intervention versus control group assignment (P = .35 and P = .51, respectively). Intervention patients were eligible for more processes of care than controls (7.8 vs 5.9 processes per patient; P = .002).
Table 2
Quality of care was higher for the intervention group than for the control group (54% vs 34% of care processes completed; P <.001). The adjusted difference in quality of care between intervention and control groups remained significant (P <.001), and the bootstrapped quality of care difference between groups was 20% favoring the intervention group (95% confidence interval = 13%, 27%). Quality of care was higher in the intervention group for all 5 conditions, and the improvement was statistically significant for dementia, falls, and incontinence (). When we restricted quality-of-care data to those conditions designated by physicians as top prior ity for referral to the NP (found in 148 patients, 74% of the sample eligible for at least 1 care process), quality of care was 60% in the intervention group and 38% in controls (P <.001). The intervention group had higher quality of care across all 5 conditions, and the improvement was statistically significant for dementia, falls, and heart failure (Table 2).
Encounter data were available for 273 patients (99%, 138 intervention and 135 control). During the project period, intervention patients made a mean of 2.5 (SD 3.2) visits to the NP. There was no difference in the number of other visits to the practice by group (7.2 intervention, 6.7 control; P =.32). Among those patients (73%, 108 intervention and 92 control) who were eligible for at least 1 ACOVE-3 process of care, intervention patients made a mean of 2.6 (SD 3.3) visits to the NP. In this subsample, other visits to the practice did not differ (6.9 intervention, 6.7 control; P = .70).
DISCUSSION
When compared with usual care by academic geriatricians, NP comanagement of 5 chronic conditions with geriatricians correlated with an absolute 20% increase in adherence to recommended care. Care for all 5 conditions was better, and this improvement was statistically significant for dementia, falls, and incontinence. Thus, NP comanagement appears to augment the quality of geriatric care even with geriatricians. Comanagement improved quality with a mean of 2.6 NP office visits during a 13-month period.
These findings extend prior research. Among low-income seniors, one study found better quality of care for depression, urinary incontinence, and falls (among other conditions) using an NP and social worker who provided home-based care management, together with a geriatrics interdisciplinary team.8 Our project differed in that we provided a less intense intervention (the NP saw patients in the office and followed up with them by phone rather than making home visits), and our intervention did not target low-income patients. A test of primary care comanagement using specially trained registered nurses showed an early beneficial effect on quality; more definitive results will be reported in the future.
Strikingly, the quality of care for chronic conditions received by control patients in this project was similar to that received by patients in previous studies who were cared for primarily by nongeriatricians, as measured by ACOVE-3 indicators.23,24 Differences from previous studies in the methods used to identify conditions and to abstract medical records, as well as the evolution of quality indicators over time, are potential explanations. Alternatively, the results may indicate that physicians face similar barriers to providing high technical quality of care for older adults, regardless of specialty.
This analysis has limitations. First, intervention group patients were eligible for more quality indicators than controls, suggesting nonequivalence of the 2 groups. Because sicker patients may receive better quality of care25,26 and because being eligible for more quality indicators may indicate a higher level of disease burden, results may be biased in favor of the intervention group. However, this potential bias is unlikely to account for the entire intervention effect. Second, 1 pair of physicians switched intervention/control group status during the project. We believe that the physician unwilling to refer patients to the NP felt total responsibility for patients and was unwilling to delegate care for this reason. Because the switch occurred to increase referrals to the NP, data were analyzed accounting for the switch rather than as intention to treat. Third, about 25% of patients were not eligible for ACOVE-3 quality indicators. This finding reflects the restricted scope of the ACOVE-3 quality indicators and potentially sparse clinical documentation that limited verification of patients’ eligibility for quality indicators.
Fourth, enhanced documentation by the NP in the intervention group may have facilitated abstractors noting completion of certain processes of care; however, prior work (not specifically including NPs) suggests that documentation is not the sole basis of poor quality of care.27 Fifth, reliability of chart reabstraction was only fair for completion/ noncompletion of recommended care processes. However, the resulting random misclassification would make estimates of between-group differences conservative. Finally, this project may be a best-case scenario because several of the study investigators, including the NP, also were clinicians in the improvement project and were motivated for the project to be properly implemented.
This study has significant strengths, however. First, external validity was improved by the quality improvement design, because all patients were eligible for participation as long as they had 1 of the 5 chronic conditions. Second, the intervention was relatively simple and can be replicated with an experienced, motivated NP using materials in the public domain.
In conclusion, a quality improvement project using an NP to manage 5 chronic conditions was associated with markedly higher technical quality of care for these conditions, suggesting that deploying NPs as chronic care clinicians may successfully complement physician practice and enhance care.
Acknowledgments
We acknowledge all the physicians and staff in the UCLA Division of Geriatrics who participated in this project. Weijuan Han, MSPH, provided programming support. Shakiba Mobaraki, MD, and Farzam Hariri, MD, MPH, did the chart abstraction. We thank the 2 anonymous peer reviewers for their comments.
Author Affiliations: From Division of Geriatric Medicine and Gerontology (DAG, JKB, HEM, DBR) and Division of General Internal Medicine (NSW), University of California, Los Angeles; Health Services Research & Development Center of Excellence (DAG), Veterans Affairs Greater Los Angeles Healthcare System, Los Angeles, CA; and RAND (CPR), Santa Monica, CA.
Funding Source: This project was supported by a grant from the John A. Hartford Foundation to Dr Reuben and a supplementary grant from the Donald W. Reynolds Foundation to Dr Koretz. Dr Ganz was supported by the US Department of Veterans Affairs, Veterans Health Administration, VA Health Services Research & Development (HSR&D) Service through the VA Greater Los Angeles HSR&D Center of Excellence (Project #VA CD2 08-012-1), and the VA/Robert Wood Johnson Foundation Physician Faculty Scholars Program. Data collection and analysis were supported in part by the UCLA Claude Pepper Older Americans Independence Center funded by the National Institute on Aging (5P30AG028748). None of the funders played a role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Author Disclosures: The authors (DAG, BKK, JKB, HEM, NSW, CPR, DBR) report no relationship or financial interest with any entity that would pose a conflict of interest with the subject matter of this article.
Authorship Information: Concept and design (DAG, JKB, NSW, CPR, DBR); acquisition of data (BKK, JKB, HEM, CPR, DBR); analysis and interpretation of data (DAG, JKB, HEM, NSW, CPR, DBR); drafting of the manuscript (DAG, HEM, CPR, DBR); critical revision of the manuscript for important intellectual content (DAG, NSW, DBR); statistical analysis (DAG, HEM); provision of study materials or patients (BKK, JKB, CPR); obtaining funding (DBR); administrative, technical, or logistic support (BKK, HEM); and supervision (BKK, DBR).
Address correspondence to: David A. Ganz, MD, PhD, Division of Geriatric Medicine and Gerontology, University of California, Los Angeles, 11301 Wilshire Blvd, Bldg 220, Rm 313 (11G), Los Angeles, CA 90073. E-mail: dganz@mednet.ucla.edu.
1. Hauer KE, Durning SJ, Kernan WN, et al. Factors associated with medical students' career choices regarding internal medicine. JAMA. 2008;300(10):1154-1164.
2. Steinbrook R. Easing the shortage in adult primary care-is it all about money? N Engl J Med. 2009;360(26):2696-2699.
3. Committee on the Future Health Care Workforce for Older Americans, Institute of Medicine. Retooling for an Aging America: Building the Health Care Workforce. Washington, DC: National Academies Press; 2008.
4. Goroll AH, Berenson RA, Schoenbaum SC, Gardner LB. Fundamental reform of payment for adult primary care: comprehensive payment for comprehensive care. J Gen Intern Med. 2007;22(3):410-415.
5. Ganz DA, Fung CH, Sinsky CA, Wu S, Reuben DB. Key elements of high-quality primary care for vulnerable elders. J Gen Intern Med. 2008;23(12):2018-2023.
6. Laurant M, Reeves D, Hermens R, Braspenning J, Grol R, Sibbald B. Substitution of doctors by nurses in primary care. Cochrane Database Syst Rev. 2005(2):CD001271.
7. Litaker D, Mion L, Planavsky L, Kippes C, Mehta N, Frolkis J. Physician-nurse practitioner teams in chronic disease management: the impact on costs, clinical effectiveness, and patients' perception of care. J Interprof Care. 2003;17(3):223-237.
8. Counsell SR, Callahan CM, Clark DO, et al. Geriatric care management for low-income seniors: a randomized controlled trial. JAMA. 2007;298(22):2623-2633.
9. Boult C, Reider L, Frey K, et al. Early effects of "Guided Care" on the quality of health care for multimorbid older persons: a cluster-randomized controlled trial. J Gerontol A Biol Sci Med Sci. 2008;63(3):321-327.
10. Unutzer J, Katon W, Callahan CM, et al; IMPACT Investigators. Improving Mood-Promoting Access to Collaborative Treatment. Collaborative care management of late-life depression in the primary care setting: a randomized controlled trial. JAMA. 2002;288(22):2836-2845.
11. Callahan CM, Boustani MA, Unverzagt FW, et al. Effectiveness of collaborative care for older adults with Alzheimer disease in primary care: a randomized controlled trial. JAMA. 2006;295(18):2148-2157.
12. Cabana MD, Rand CS, Powe NR, et al. Why don't physicians follow clinical practice guidelines? A framework for improvement. JAMA. 1999;282(15):1458-1465.
13. UCLA GeroNet. Patient care resources. ACOVE. http://www. geronet.ucla.edu/index.php?option=com_content&view=category&lay out=blog&id=111&Itemid=189. Accessed December 11, 2010.
14. Feil DG, MacLean C, Sultzer D. Quality indicators for the care of dementia in vulnerable elders. J Am Geriatr Soc. 2007;55(suppl 2): S293-S301.
15. Nakajima GA, Wenger NS. Quality indicators for the care of depression in vulnerable elders. J Am Geriatr Soc. 2007;55(suppl 2): S302-S311.
16. Chang JT, Ganz DA. Quality indicators for falls and mobility problems in vulnerable elders. J Am Geriatr Soc. 2007;55(suppl 2): S327-S334.
17. Heidenreich PA, Fonarow GC. Quality indicators for the care of heart failure in vulnerable elders. J Am Geriatr Soc. 2007;55(suppl 2):S340-S346.
18. Fung CH, Spencer B, Eslami M, Crandall C. Quality indicators for the screening and care of urinary incontinence in vulnerable elders. J Am Geriatr Soc. 2007;55(suppl 2):S443-S449.
19. Hunt SA; American College of Cardiology; American Heart Association Task Force on Practice Guidelines (Writing Committee to Update the 2001 Guidelines for the Evaluation and Management of Heart Failure). ACC/AHA 2005 guideline update for the diagnosis and management of chronic heart failure in the adult: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Update the 2001 Guidelines for the Evaluation and Management of Heart Failure) [published correction appears in J Am Coll Cardiol. 2006;47(7):1503-1505]. J Am Coll Cardiol. 2005;46(6):e1-e82.
20. Sodeman WA, Sodeman TC. Instructions for Geriatric Patients. Philadelphia, PA: Elsevier Saunders; 2005.
21. UCLA GeroNet. UCLA geriatric patient care. Patient education materials. http://www.geronet.ucla.edu/index.php?option=com_conten t&view=article&id=116&Itemid=172. Accessed December 11, 2010.
22. De Vries H, Elliott MN, Kanouse DE, Teleki SS. Using pooled kappa to summarize interrater agreement across many items. Field Methods. 2008;20(3):272-282.
23. Wenger NS, Solomon DH, Roth CP, et al. The quality of medical care provided to vulnerable community-dwelling older patients. Ann Intern Med. 2003;139(9):740-747.
24. Wenger NS, Roth CP, Shekelle PG, et al. A practice-based intervention to improve primary care for falls, urinary incontinence, and dementia. J Am Geriatr Soc. 2009;57(3):547-555.
25. Min LC, Wenger NS, Fung C, et al. Multimorbidity is associated with better quality of care among vulnerable elders. Med Care. 2007; 45(6): 480-488.
26. Higashi T, Wenger NS, Adams JL, et al. Relationship between number of medical conditions and quality of care. N Engl J Med. 2007;356 (24): 2496-2504.
27. Kahn KL, Rogers WH, Rubenstein LV, et al. Measuring quality of care with explicit process criteria before and after implementation of the DRG-based prospective payment system. JAMA. 1990; 264 (15): 1969-1973.
Quality of Life: The Pending Outcome in Idiopathic Pulmonary Fibrosis
February 6th 2026Because evidence gaps in idiopathic pulmonary fibrosis research hinder demonstration of antifibrotic therapies’ impact on patient quality of life (QOL), integrating validated health-related QOL measures into trials is urgently needed.
Read More
Building Trust: Public Priorities for Health Care AI Labeling
January 27th 2026A Michigan-based deliberative study found strong public support for patient-informed artificial intelligence (AI) labeling in health care, emphasizing transparency, privacy, equity, and safety to build trust.
Read More
Ambient AI Tool Adoption in US Hospitals and Associated Factors
January 27th 2026Nearly two-thirds of hospitals using Epic have adopted ambient artificial intelligence (AI), with higher uptake among larger, not-for-profit hospitals and those with higher workload and stronger financial performance.
Read More
Motivating and Enabling Factors Supporting Targeted Improvements to Hospital-SNF Transitions
January 26th 2026Skilled nursing facilities (SNFs) with a high volume of referred patients with Alzheimer disease and related dementias may work harder to manage care transitions with less availability of resources that enable high-quality handoffs.
Read More

