- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
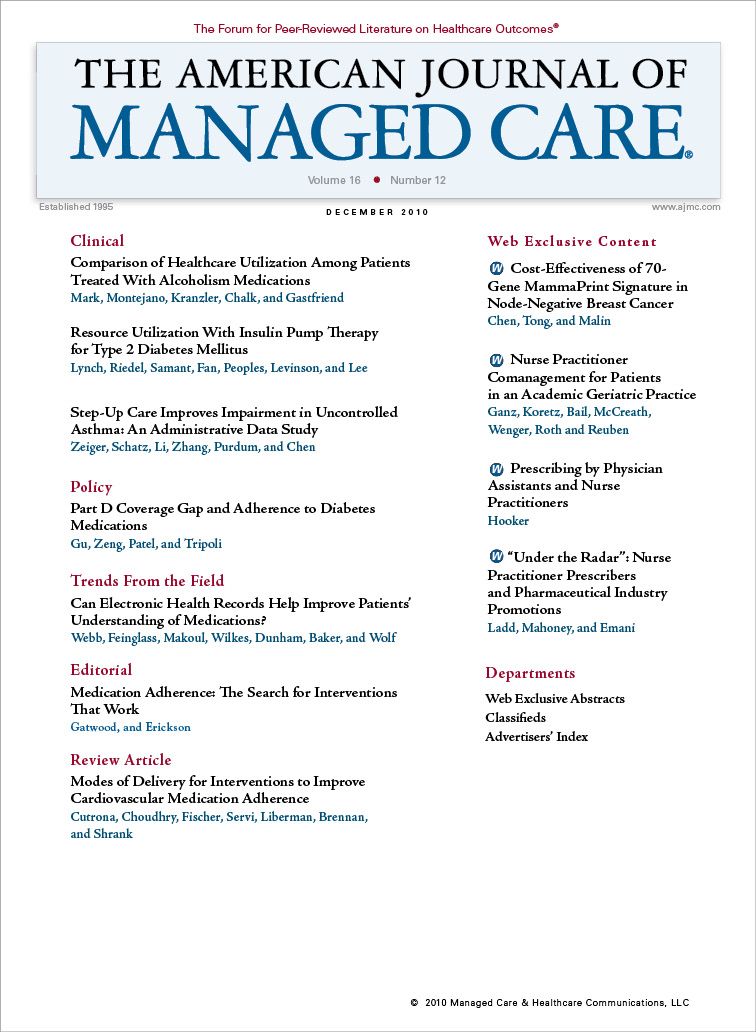
Resource Utilization With Insulin Pump Therapy for Type 2 Diabetes Mellitus
A retrospective claims analysis of managed care enrollees with type 2 diabetes mellitus showed that insulin pump therapy reduced antidiabetic drug and healthcare resource use.
Objectives:
To evaluate the effects of switching from multiple daily injection (MDI) therapy to insulin pump therapy, also called continuous subcutaneous insulin infusion (CSII), on antidiabetic drug and healthcare resource utilization.
Study Design:
This study was a retrospective analysis of administrative claims data from a large geographically diverse health plan in the United States from January 1, 2005, through April 30, 2008.
Methods:
Changes in antidiabetic drug use, antidiabetic drug switching and augmentation, and healthcare utilization during the baseline period and after CSII initiation were assessed using paired t test.
Results:
There were 3649 possible subjects, of whom 943 met the criteria for analysis. The mean number of antidiabetic drugs used decreased by 46% after CSII initiation, and the mean reduction in antidiabetic drug utilization was 0.67; both were statistically significant. More than one-third of subjects who were taking antidiabetic drugs before CSII initiation discontinued oral therapy after CSII initiation. The number of subjects using multiple antidiabetic drugs significantly decreased after CSII initiation by 58%, and rates of switching or augmenting significantly decreased from 42% at baseline to 25% after CSII initiation.The rates of emergency department visits and inpatient admissions significantly decreased, and the rate of ambulatory visits significantly increased.
Conclusions:
CSII was associated with significant decreases in antidiabetic drug and healthcare resource utilization, contributing to stability of care. The evidence from this study indicates that CSII should be considered as an option for patients with type 2 diabetes mellitus who are using MDI and are experiencing a high degree of antidiabetic drug and healthcare resource utilization.
(Am J Manag Care. 2010;16(12):892-896)
A retrospective analysis of a large sample of managed care enrollees with type 2 diabetes mellitus was performed to examine the effect on antidiabetic drug and healthcare resource utilization of switching from multiple daily injections to insulin pump therapy, also called continuous subcutaneous insulin infusion.
- After initiation of continuous subcutaneous insulin infusion, antidiabetic drug utilization was reduced by 0.67 drug (a change of 46%), and more than one-third of subjects discontinued antidiabetic drugs altogether.
- Inpatient admissions and emergency department visits decreased significantly. Ambulatory visits increased significantly.
- Continuous subcutaneous insulin infusion should be considered an alternative to continued use of multiple daily injections after the latter therapy has failed.
A major challenge of managing type 2 diabetes mellitus (T2D) is the escalation of therapies in the response to treatment regimen failure. Indeed, this treatment escalation is now the standard of care for this disease. Antidiabetic drugs are added to therapy regimens if hyperglycemia and elevated glycosylated hemoglobin (A1C) values persist after the first stage of lifestyle and pharmacologic interventions.1 Intensive insulin therapy is often not added until multiple antidiabetic drugs fail to maintain euglycemia. However, even with the addition of insulin, many patients continue using multiple antidiabetic drugs. Moreover, as the disease progresses, patients with T2D have increased healthcare resource utilization, including emergency department (ED) visits and inpatient admissions for diabetesrelated complications and comorbidities.2-4 Insulin pump therapy, also called continuous subcutaneous insulin infusion (CSII), is not usually initiated in most T2D treatment regimens until multiple daily injection (MDI) therapy has failed. A few studies5-9 have examined whether switching from antidiabetic drugs or conventional insulin therapy to CSII offers a clinical benefit over switching to MDI. Such studies have focused on change in A1C level and have had mixed results. These studies did not examine whether CSII reduces utilization of antidiabetic drugs or other healthcare resources.
A plausible area for investigation drawn from the sparse literature about CSII in T2D is whether switching to this therapy after MDI has failed can reduce the number of antidiabetic drugs used and the amount of healthcare resource utilization needed to manage the disease. The present study investigates antidiabetic drug and healthcare resource utilization among a large real-world population of patients with T2D who switched from MDI to CSII.
METHODS
This study was a claims analysis using medical, pharmacy, enrollment, and laboratory data to assess the effects of switching from MDI to CSII. Subjects were enrollees in a large geographically diverse US managed care health plan with documentation of T2D. No identifiable protected health information was extracted or accessed during the course of the study. Pursuant to the Health Insurance Portability and Accountability Act of 1996,10 the use of deidenti-fied data does not require institutional review board approval or waiver of authorization. Clinical outcomes (change in A1C levels and A1C targets) of this population are published separately.11
Medical claims or encounter data were collected from all available points of service such as inpatient and outpatient hospital records, ED visits, physician’s office encounters, and surgery center data, including specialty, preventive, and office-based treatments. Medical claims and coding conformed to insurance industry standards. Included in the database were pharmacy claims representing all prescriptions filled at outpatient pharmacies and submitted to the insurance plan for reimbursement. A 12-month period before CSII initiation was used to examine baseline demographic and clinical characteristics. The follow-up period was a minimum of 6 months and a maximum of 40 months. Baseline and follow-up periods were measured from the date of CSII initiation. Data from January 1, 1998, through April 30, 2008, were included in the study.
Patients were included if they initiated CSII during the subject identification period (January 1, 2005, through October 31, 2007) and had evidence of T2D. Evidence of T2D was determined by the presence of International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes for T2D (a fifth digit of 0 or 2) in the medical record or by the use of any oral antidiabetic drug or exenatide in the claims history. Exclusion criteria included age younger than 18 years, missing information on sex, evidence of CSII use during the baseline period, lack of continuous enrollment in the health plan for a 12-month baseline period or less than a 6-month follow-up period, and type 1 diabetes mellitus—related ICD-9-CM codes without evidence of oral antidiabetic drug or exenatide use.
Claims were analyzed at the baseline period and after CSII initiation for changes in antidiabetic drug (defined as any oral antidiabetic drug or exenatide) and healthcare resource utilization. Change in antidiabetic drug utilization was calculated as the number of antidiabetic drugs used after CSII initiation minus the number of antidiabetic drugs used during the baseline period. Healthcare resource utilization was calculated as the rate of ED visits, inpatient admissions, and ambulatory visits per subject per month (PSPM) during the baseline period and after CSII initiation. The number of ambulatory visits represented all visits for outpatient services that generated costs for care and not just physician office visits for the care and management of diabetes.
All study variables were analyzed descriptively. Numbers and percentages were provided for dichotomous and polychotomous variables. Means, medians, standard deviations,and percentiles were calculated for continuous variables. Univariate analysis using paired t test was performed on the changes in antidiabetic drug and healthcare resource utilization. P <.05 was considered statistically significant.
RESULTS
Antidiabetic Drug Utilization
Figure 1
Table 1
Of 3649 enrollees identified as having T2D and using CSII, 943 met criteria for inclusion in the study (). Their mean age was 48 years, and they were followed up for a mean of 17 months (range, 6-39 months) (). Commonly reported comorbid conditions included lipid metabolism disorders, hypertension, and diseases of the heart, thyroid, and eye.
Table 2
The mean (SD) number of antidiabetic drugs used per subject decreased from 1.45 (1.16) during the baseline period to 0.78 (1.01) after CSII initiation (a change of 46%, P<.001), which represented a mean (SD) reduction in antidiabetic drug utilization of 0.67 (1.26) (P < .001). Among 4 commonly used antidiabetic drugs (exenatide, metformin, sulfonylurea, and thiazolidine-dione), the reductions in utilization after CSII initiation ranged from 27% to 59% ().
Figure 2
There was a statistically significant increase in the number of subjects taking zero antidiabetic drugs and a statistically significant decrease in the number of subjects taking 2 or 3 or more antidiabetic drugs (). The number of subjects using multiple antidiabetic drugs decreased from 380 (40%) during the baseline period to 161 (17%) after CSII initiation, a statistically significant reduction of 58% (P <.001). More than onethird of subjects (270 of 755 [36%]) taking antidiabetic drugs during the baseline period discontinued antidiabetic drugs after CSII initiation.
Significantly fewer subjects added antidiabetic drugs to their therapy regimen after CSII initiation (236 subjects [25%]) than during the baseline period (396 subjects [42%]) (P <.001). More subjects discontinued and switched antidiabetic drugs after CSII initiation than during the baseline period, but the difference was not statistically significant (62 [7%] to 82 [9%] for discontinuation [P = .09]; 21 [2%] to 12 [1%] for switching [P = .12]).
Healthcare Resource Utilization
Table 3
From the baseline period to after CSII initiation, there was a statistically significant decrease in ED visits and inpatient admissions (0.03 PSPM [P = .001] and 0.02 PSPM [P <.001], respectively) and a statistically significant increase in ambulatory visits (0.21 PSPM [P <.001]). When the change in PSPM rate was projected over 4 years, the resultant healthcare resource utilization was 1.4 fewer ED visits and 1 fewer inpatient admission by using CSII rather than MDI. When the change in PSPM rate was projected over 1 year, the result was 0.4 less ED visit and 0.2 less inpatient admission ().
DISCUSSION
This large real-world population experienced significant and meaningful benefits by switching from MDI to CSII. We found statistically significant reductions in antidiabetic drug utilization, ED visits, and inpatient admissions. The results from our study suggest that CSII may allow patients with T2D to reduce their antidiabetic drug use. The number of subjects using multiple antidiabetic drugs decreased after CSII initiation, while the number of subjects taking zero antidiabetic drugs increased; these differences were statistically significant. When projected over 4 years of CSII use, the statistically significant reductions in healthcare resource utilization resulted in approximately 1 fewer inpatient admission and 1.4 fewer ED visits. Reduced ED visits and inpatient admissions may result from better glycemic control, although the study design restricted our making firm conclusions. Over time, we would expect that reductions in the rates of inpatient admissions and ED visits could decrease even more. As expected, there was a statistically significant increase in ambulatory visits from the baseline period to after CSII initiation. This increase likely resulted from additional training and therapy customization required to use an insulin pump. Indeed, the decreased antidiabetic drug utilization, ED visits, and inpatient admissions support the conclusion that the increase in ambulatory visits did not result from disease progression. Positive results in other areas of the subjects’ claims histories indicate that expertise reduced the need for concomitant medication and the incidence ofconditions requiring urgent care.
We note several limitations to our study. We could not capture all aspects of each subject’s medical history because the data were collected for payment and not for research. Such data help us to understand healthcare resource utilization but may be biased by coding errors, undercoding, and coding for the purpose of ruling out something other than the actual disease. Also, the design of our analysis did not allow us to control for treatment decisions. Inclusion in the study was determined by CSII initiation, thus negating the possibility of a control group. The 1-year and 4-year projections of healthcare resource utilization did not take disease progression into account, and ambulatory visits could not be projected owing to the many training visits immediately after CSII initiation. Finally, the high PSPM rate of ambulatory visits was influenced by the method of data extraction, which included all visits for outpatient services that generate costs for care. For example, the rate includes laboratory services at a freestanding laboratory and visits for diabetes education.
We did not include a control group but chose instead to analyze utilization before and after initiation of CSII. Both pre—post and treatment–control group designs are used in the assessment of observational data. The treatment–control group design, while perhaps controlling for temporal changes in diabetes management, suffers from inherent selection bias issues. That is, subjects who receive an insulin pump for management of their diabetes are likely in a different stage of disease compared with those who do not. We determined that the disadvantages of this type of selection effect outweighed the benefits of this design. The pre–post design (similar to a repeated-measures design in its handling of the data) offers the advantage of each subject serving as his or her own control, although it is not without limitations. Moreover, the limitation of not having a control group is somewhat mitigated by the use of real-world data, thus showing a possible treatment effect without a clinical study effect.
In conclusion, continuous subcutaneous insulin infusion was associated with significant decreases in antidiabetic drug and healthcare resource utilization, contributing to stability of care. The evidence from this study indicates that CSII should be considered as an option for patients with T2D who are using MDI and are experiencing a high degree of antidiabetic drug utilization and healthcare resource utilization.
Author Affiliations: From Medtronic, Inc (PML, TP, JL, SWL), Northridge, CA; i3 Innovus (AAR, NS, YF), Eden Prairie, MN.
Funding Source: The study was funded by Medtronic, Inc.
Author Disclosures: Mr Lynch, Mr Peoples, Ms Levinson, and Dr Lee report being employees and stockholders of Medtronic, Inc. Dr Riedel, Mr Samant, and Mr Fan are employees of i3 Innovus, and their company received payment from Medtronic, Inc to complete this analysis. Authorship Information: Concept and design (PML, AAR, JL, SWL); acquisition of data (PML, AAR, YF); analysis and interpretation of data (PML, AAR, NS, YF, TP, JL, SWL); drafting of the manuscript (PML, AAR, NS, TP, SWL); critical revision of the manuscript for important intellectual content (PML, AAR, TP, JL); statistical analysis (PML, AAR, NS, YF); provision of study materials or patients (SWL); obtaining funding (PML); administrative, technical, or logistic support (TP); and supervision (PML, JL, SWL).
Address correspondence to: Peter M. Lynch, MPH, Medtronic, Inc, 18000 Devonshire St, Northridge, CA 91325. E-mail: peter.m.lynch@medtronic.com.
1. Nathan DM, Buse JB, David son MB, et al. Management of hyperglycemia in type 2 diabetes: a consensus algorithm for the initiation and adjustment of therapy: a consensus statement from the American Diabetes Association and the European Association for the Study of Diabetes [published correction appears in: Diabetes Care. 2006;29(11):2816-2818]. Diabetes Care. 2006;29(8):1963-1972.
2. Huang ES, Gleason S, Gaudette R, et al. Health care resource utilization associated with a diabetes center and a general medicine clinic. J Gen Intern Med. 2004;19(1):28-35.
3. Pelletier EM, Smith PJ, Boye KS, Misurski DA, Tunis SL, Minshall ME. Direct medical costs for type 2 diabetes mellitus complications in the US commercial payer setting: a resource for economic research. Appl Health Econ Health Policy. 2008;6(2-3):103-112.
4. Brandle M, Zhou H, Smith BR, et al. The direct medical cost of type 2 diabetes. Diabetes Care. 2003;26(8):2300-2304.
5. Berthe E, Lireux B, Coffin C, et al. Effectiveness of intensive insulin therapy by multiple daily injections and continuous subcutaneous infusion: a comparison study in type 2 diabetes with conventional insulin regimen failure. Horm Metab Res. 2007;39(3):224-229.
6. Herman WH, Ilag LL, Johnson SL, et al. A clinical trial of continuous subcutaneous insulin infusion versus multiple daily injections in older adults with type 2 diabetes. Diabetes Care. 2005;28(7):1568-1573.
7. Monami M, Lamanna C, Marchionni N, Mannucci E. Continuous subcutaneous insulin infusion versus multiple daily insulin injections in type 2 diabetes: a meta-analysis. Exp Clin Endocrinol Diabetes. 2009;117(5):220-222.
8. Raskin P, Bode BW, Marks JB, et al. Continuous subcutaneous insulin infusion and multiple daily injection therapy are equally effective in type 2 diabetes: a randomized, parallel-group, 24-week study. Diabetes Care.2003;26(9):2598-2603.
9. Wainstein J, Metzger M, Boaz M, et al. Insulin pump therapy vs. multiple daily injections in obese type 2 diabetic patients. Diabet Med. 2005;22(8):1037-1046.
10. Centers for Medicare and Medicaid Services. Health Insurance Portability and Accountability Act of 1996. Public Law 104-191, 104th Congress. http://www.cms.hhs.gov/HIPAAGenInfo/Downloads/HIPAALaw. pdf. Accessed May 4, 2010.
11. Lynch P, Riedel AA, Samant N, Fan Y, Peoples T, Lee SW. Improved A1C by switching to continuous subcutaneous insulin infusion from injection insulin therapy in type 2 diabetes: a retrospective claims analysis [published online ahead of print September 8, 2010]. Prim Care Diabetes. doi:10.1016/j.pcd.2010.07.004. Medline:20832374.
Building Trust: Public Priorities for Health Care AI Labeling
January 27th 2026A Michigan-based deliberative study found strong public support for patient-informed artificial intelligence (AI) labeling in health care, emphasizing transparency, privacy, equity, and safety to build trust.
Read More
Ambient AI Tool Adoption in US Hospitals and Associated Factors
January 27th 2026Nearly two-thirds of hospitals using Epic have adopted ambient artificial intelligence (AI), with higher uptake among larger, not-for-profit hospitals and those with higher workload and stronger financial performance.
Read More
Motivating and Enabling Factors Supporting Targeted Improvements to Hospital-SNF Transitions
January 26th 2026Skilled nursing facilities (SNFs) with a high volume of referred patients with Alzheimer disease and related dementias may work harder to manage care transitions with less availability of resources that enable high-quality handoffs.
Read More
Specialty and Operator Status Influence Electronic Health Record Use Variation
January 22nd 2026Operators demonstrated specialty-specific differences in electronic health record efficiency, timeliness, and after-hours use, highlighting how workflow and training shape documentation behaviors across medical disciplines.
Read More

