- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Why EOM Participation Was Extremely Low—and How to Fix It
In June 2022, the Center for Medicare and Medicaid Innovation (CMMI) announced the application period for the Enhancing Oncology Model (EOM),1 the successor value-based payment model for medical oncology that followed the conclusion of CMMI’s Oncology Care Model (OCM). During the application period there was skepticism about the model among potential participants, but also overwhelming optimism and interest in figuring out how to navigate several profound challenges in EOM design relative to OCM.2,3 The high number of EOM applicants represented clear evidence of such interest.4
However, by the time EOM launched on July 1, 2023, the challenges and skepticism had mostly won out, to a degree that can be easily quantified by considering the following figures:
- There were 190 OCM participants at the time that model launched in July 2016.5
- There were 122 OCM participants at the time the model concluded, with episodes ending in June 2022.6
- There were only 44 participants in EOM at the start of the model on July 1, 2023.7
Key insights from practices that participated in OCM were well publicized throughout the model, and these insights now are much more clearly understood throughout the field of oncology (both among participants in the model and nonparticipants) than they were in 2016. Understanding these key insights, and the extent to which the design of EOM rendered them less applicable to participants’ success in this new CMMI model, is critical to understanding the key drivers of the current state of participation in EOM and other value-based payment opportunities in oncology.
One of these foundational insights from OCM participation is how significantly Monthly Enhanced Oncology Services (MEOS) payments contributed to practice transformation. Practices utilized MEOS payments to implement the required practice redesign activities of OCM, build the data analytics and reporting capabilities needed to meet the requirements for participating in the model, and to execute best practices in controlling cost and other practice improvement activities.
Furthermore, the development of multifaceted strategies for the overall management of financial risk in value-based payment emerged as a core competency of practices that were successful in OCM, with the intention that those competencies would materially impact future success in other value-based payment models that exhibit downside financial risk. For many OCM participants, such strategy sets included a combination of cost savings initiatives, data analytics capabilities, and the emergence of stop-loss insurance products.
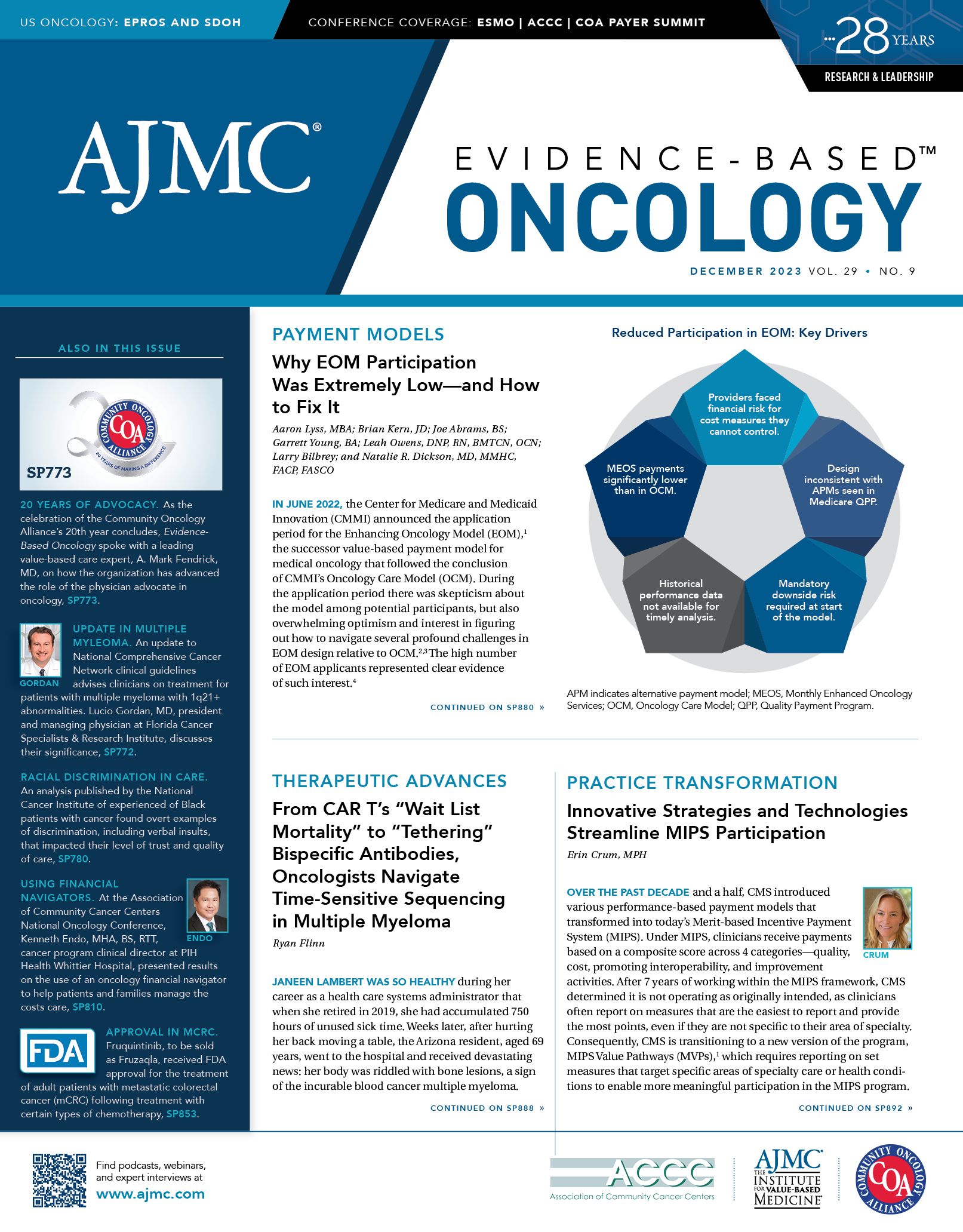
Over time, practices experienced the benefits of having made such investments, both through generating substantial savings in OCM and from taking their OCM practice transformation efforts and applying those initiatives to opportunities for similar commercial payer arrangements. However, due to the challenges that practices faced in CMMI’s rollout of EOM, this did not come to fruition for EOM to the extent needed for participation to be feasible for most of the practices that applied. Furthermore, the key drivers of this outcome can be thought of as intertwined with improvements to EOM (or any future value-based oncology model that involves financial risk) that would be necessary to increase participation:
Driver 1: EOM puts providers at financial risk for cost measures they cannot control.
For oncology providers to accept downside risk in any Medicare or commercial payer arrangement, the incentives of the model must be built on measures of quality and cost that accurately reflect the “value” of provider adherence to consensus standards of care. For example, provider organizations with a track record of adherence to clinical pathways are likely to participate in alternative payment models when downside financial risk is tied to high-value drug utilization. By contrast, to the extent that the financial incentives of any payment model have a potential to penalize providers for adherence to consensus standards for high-quality treatment, oncology practices are unlikely to participate.
These concerns were paramount in practices’ decisions to participate in EOM. Financial risk in EOM is principally tied to whether the actual cost of care for a practice’s patient population is above or below Medicare’s predicted expenditures. The methodology that EOM utilizes to set the expected cost of a practice’s EOM episodes is derived primarily from correlations between the total cost of care for each of the 7 cancer types and factors that can be analyzed in claims data for each episode. Therefore, the cost of care that Medicare predicts for individual episodes can be insensitive to the clinical characteristics of patients on which treatment decisions are based.
To be clear, these concerns were also applicable to OCM payment methodology8; however, additional differences between OCM and EOM that are noted below exponentially amplified these concerns among potential participants in EOM and therefore significantly reduced model participation.
Driver 2: EOM’s design is almost completely inconsistent with the Advanced APM incentives available through Medicare’s Quality Payment Program (QPP).
OCM design, and specifically the scope of the included cancer types and thereby the size of the included patient population, allowed practices that took downside risk to benefit from the QPP incentives associated with Advanced Alternative Payment Model (APM) participation.9 It is difficult to overstate how important those incentives were to OCM downside risk participation for those practices. Such incentives fell into 2 categories:
- Financial incentives
- Nonfinancial incentives in the form of avoidable QPP reporting burden
In contrast, the design of EOM (mainly by virtue of the limited diseases and thereby a smaller patient population included in the model) was largely incongruent with Medicare QPP criteria for qualifying for the incentives for Advanced APM participation.
In any future Medicare APM for oncology, CMMI’s design and implementation of these programs should be carefully coordinated with QPP and other US Department of Health and Human Services initiatives to maximize the incentives for model participants that take downside financial risk. Such incentives should include financial incentives and regulatory burden relief.
It would be unrealistic for participants in EOM to think that such incentives would be as favorable as they were in OCM. However, because these incentives were a significant factor for practices that elected downside risk in OCM, it is also unrealistic to think that removing these incentives entirely would allow practices to view downside risk in EOM as a viable option.
Driver 3: EOM featured mandatory downside risk immediately upon the start of the model.
At the time that OCM transitioned to downside risk, practices had several performance periods of Reconciliation Reports informing their cost performance, complete with all the adjustments noted in the section above. This enabled practices (and underwriters of stop-loss insurance products) to have much higher confidence in cost performance projections than was possible for EOM because key episode pricing adjustments were not included in the EOM Historical Period (HP) data set, and participants only had access to HP data for an extremely brief period prior to the start of the model. For this reason, one of the following changes would be needed to enable increased participation in future value-based payment models that feature downside risk:
- HP data provided to participants prior to the model start would have to be more suitable for developing cost performance projections by providing sufficient insight into episode cost adjustments and by providing practices adequate time to refine their projections based on future performance assumptions.
- The initial period of participation would have to include an upside-only option so that practices and stop-loss insurance underwriters could more confidently project future cost performance under a downside risk arrangement.
Driver 4: HP data available to practices prior to the start of the model and the timeline in which data were released to potential participants did not allow them to clearly define a road map for the financial viability of EOM participation.
Prior to the start of the model, participants who were accepted in EOM and submitted an EOM Participation Agreement (PA) were eligible to request practice-specific HP data spanning 2019-2021. However, the contents of that data set and the timeline in which it was provided imposed significant impediments on practices that hoped the data would help them understand which cost savings levers they could implement that would lead to positive performance in the model. Such impediments included the following:
- Practices did not receive the PA until April 2023. This critical step in the EOM rollout needed to occur earlier, several months prior to the start of the model, for practices to have adequate time to prepare for the start of the model based on substantial differences between the OCM and EOM PAs.
- Practices that signed the PA were not eligible to request HP data until May 2023.
- Practices that requested HP data did not receive those data until May 19, 2023.
- The HP data that practices received only allowed for estimates of several episode pricing adjustments that would be significant drivers of whether a practice would generate savings or would owe money to Medicare for cost target overages (e.g. Novel Therapies Adjustments, Clinical Data Adjustments, Experience Adjustments).
If Medicare or private payers neglect to give practices adequate access to data that practices need to develop performance projections—which are used to estimate the impact of their improvement efforts—practices likely will decline to participate in these models.
Specifically for EOM, the gaps in the HP data set noted above and the short time frame prior to the start of the model in which HP data were received created significant challenges for practices that planned to pursue stop-loss insurance options for EOM. As previously noted, stop-loss insurance was a key element of financial-risk mitigation for many OCM practices that participated in downside risk during OCM.
Driver 5: The MEOS payments available to practices were significantly lower than in OCM.
As noted above, OCM MEOS payments were critical to practice transformation in OCM and development and implementation of core competencies for the management of financial risk. Based on the conclusions articulated in the OCM Evaluation Report, which emphasized MEOS payments as a driver of the lack of savings in the model, it is not surprising that MEOS payments were lowered for EOM.10 However, there are 2 critical differences between OCM and EOM that would imply that higher MEOS payments in EOM would be warranted:
- The Participant Redesign Activities included in EOM are far more extensive than the OCM Practice Redesign Activities. Notable examples of these increased participation requirements include requirements to implement electronic patient-reported outcomes and the inclusion of health-related social need factors among practices’ data collection and documentation requirements.
- EOM exhibited downside risk at the outset of the model. If EOM included an upside-only participation option, lower MEOS payments would have been more reasonably expected given the findings of the OCM Evaluation Report.10
However, when payment models transition to include downside risk for total cost of care (in which MEOS payments are factored into a participant’s total cost) the value of these payments should be significantly increased because practices are at financial risk for generating excess savings beyond the MEOS payment amounts included in the total cost of the episode.
To be fair, perhaps it was unrealistic to think that practices seeking to participate in EOM would not encounter any of the challenges noted above. We will never know the extent to which participation in EOM would have been substantially higher if practices only faced 1, or 2, or 3, or 4 of these barriers to EOM participation. What we know conclusively at this point is the impact on participation of all 5 of these barriers combined. This aggregate effect has elucidated what is required for practices to participate in this model in the face of such challenges:
- Practices must have engrained commitments to a culture of value-based care.
- Practices must have confidence that their track record of success in value-based payment will allow them to enhance the financially stability of their practice.
- Practices must have a high degree of confidence that CMMI will make improvements to EOM over time.
As the Community Oncology Alliance very clearly stated in its June 2023 statement on the EOM, CMS has not provided any adequately concrete indications that substantial improvements to the model will be forthcoming.11 However, practices that participated in OCM had relevant experience on which to base assumptions that improvements to EOM could come to fruition. For example, at the initiation of OCM, the episode pricing methodology featured a single episode price for breast, prostate, and bladder cancers. Very quickly, CMMI pivoted to setting 2 separate prices for each of these cancer types. Furthermore, the high-risk vs low-risk cohorts driving the 2 different prices were defined by clinically relevant classes of therapies used in the treatment of each cohort. This was a critical pivot during OCM. For EOM to be financially viable for participating practices, CMMI likely will have to implement similar constructs for EOM episode prices throughout the model.
If CMMI were to make substantial improvements to EOM or any future oncology model consistent with these suggestions, model participation would commensurately increase. As a field, it is important that we clearly articulate the basis on which practices will make these decisions for future Medicare and commercial value-based payment to adapt to what went right for practices that participated in OCM, and why the barriers to participation in EOM ultimately proved insurmountable for the vast majority of those practices that sought to participate in that model.
Author Information
Aaron Lyss, MBA, is director, strategic payer relations, OneOncology. Brian Kern, JD, is CEO, Deep Risk Management, a value-based financial risk brokerage and consulting firm. Joe Abrams, BS, is senior manager, strategic analytics, OneOncology. Garrett Young, BA, is vice president, clinical and strategic analytics, OneOncology. Leah Owens, DNP, RN, BMTCN, OCN, is executive director, care transformation, Tennessee Oncology. Larry Bilbrey, BBA, is program director, data and analytics, Tennessee Oncology. Natalie R. Dickson, MD, MMHC, FACP, FASCO, is president and chief strategy officer, Tennessee Oncology.
References
- Enhancing Oncology Model. CMS. Accessed November 5, 2023.
https://go.cms.gov/3Qp1Ppt - Caffrey M. Amid concerns, will practices take part in the Enhancing Oncology Model? Am J Manag Care. 2023;29(4):SP328.
- Mullangi S, Parikh RB, Schleicher SM. Next-generation alternative payment models in oncology—will precision preclude participation? JAMA Oncol. 2023;9(4):457-458. doi:10.1001/jamaoncol.2022.7179
- Hoffman E. All 14 OneOncology partner practices apply to participate in EOM. News release. OneOncology. October 3, 2022. Accessed November 5, 2023. https://bit.ly/3SnLUKI
- Evaluation of the Oncology Care Model: performance period one. CMS. Accessed November 5, 2023. https://bit.ly/461yG9q
- Oncology Care Model. CMS. Accessed November 5, 2023. https://bit.ly/3SvdHsQ
- Caffrey M. Final EOM list favors larger practices; AON strategy helps smaller groups. Am J Manag Care. 2023;29(7):SP633-SP635. doi:10.37765/ajmc.2023.89421
- Lyss AJ, Supalla SN, Schleicher SM. The Oncology Care Model—why it works and why it could work better: accounting for novel therapies in value-based payment. JAMA Oncol. 2020;6(8):1161-1162. doi:10.1001/jamaoncol.2019.4385
- Quality Payment Program. CMS. Accessed November 5, 2023.
https://qpp.cms.gov/ - Trombley M, McClellan S, Hassol A, et al for Abt Associates; Simon C, Shen Y, Kappes A, et al for The Lewin Group; Keating NL, Landrum MB, Riedel L, Liu MPH, Lii J for Harvard Medical School; Brooks GA, Kapadia NS for Geisel School of Medicine at Dartmouth; Kummet C, Hsu VD, Shao S for General Dynamics Information Technology. Evaluation of the Oncology Care Model, executive summary: performance periods 1-9. CMS. June 2023. Accessed November 5, 2023. https://bit.ly/46ZoZtE
- COA: extremely disappointed in CMMI decision to launch flawed Medicare oncology model. News release. Community Oncology Alliance. June 29, 2023. Accessed November 5, 2023. https://bit.ly/45Vxapy
Building Trust: Public Priorities for Health Care AI Labeling
January 27th 2026A Michigan-based deliberative study found strong public support for patient-informed artificial intelligence (AI) labeling in health care, emphasizing transparency, privacy, equity, and safety to build trust.
Read More
Ambient AI Tool Adoption in US Hospitals and Associated Factors
January 27th 2026Nearly two-thirds of hospitals using Epic have adopted ambient artificial intelligence (AI), with higher uptake among larger, not-for-profit hospitals and those with higher workload and stronger financial performance.
Read More
Motivating and Enabling Factors Supporting Targeted Improvements to Hospital-SNF Transitions
January 26th 2026Skilled nursing facilities (SNFs) with a high volume of referred patients with Alzheimer disease and related dementias may work harder to manage care transitions with less availability of resources that enable high-quality handoffs.
Read More
Specialty and Operator Status Influence Electronic Health Record Use Variation
January 22nd 2026Operators demonstrated specialty-specific differences in electronic health record efficiency, timeliness, and after-hours use, highlighting how workflow and training shape documentation behaviors across medical disciplines.
Read More
