- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Making Cancer Care Better by Measuring It in Real Time
Coverage from The US Oncology Network Payer Transformation Summit, held September 27-29, 2023, in Atlanta, Georgia.
As director of quality portfolio strategy for McKesson and The US Oncology Network, Erin Crum, MPH, has seen the evolution of quality
Crum

measurement. Crum works with The Network’s physicians and practices and McKesson’s technology team to create cancer quality measures that truly move the needle forward. The goal, as Crum describes it, is not participation in CMS programs such as the Merit-based Incentive Payment System (MIPS), as ends to themselves, but for a good score to be a “byproduct” of ongoing improvements in care. In addition, Crum told Evidence-Based Oncology (EBO), how McKesson has created dashboards that give oncologists and practice leaders real-time data on how they are faring in quality programs, so there are no year-end surprises. McKesson is also rolling out a new tool to allow practices to track patients’ social determinants of health (SDOH) data, based on the National Comprehensive Cancer Network (NCCN) Stress Thermometer.1
This interview has been condensed and edited for clarity.
EBO: How has the nature of quality measurement changed over time?
Crum: I’ve been with McKesson for almost 20 years, and I oversee our qualified clinical data registry, or QCDR. I work directly with clinicians in The US Oncology Network and with our technology team to design, develop, and implement custom QCDR measures that help our practices to really home in on how they performed on certain very specific cancer quality measures. The [Physician Quality Reporting System] started in 2007;2 that was the first time that practices needed to report for quality data to the government that was tied to reimbursement.
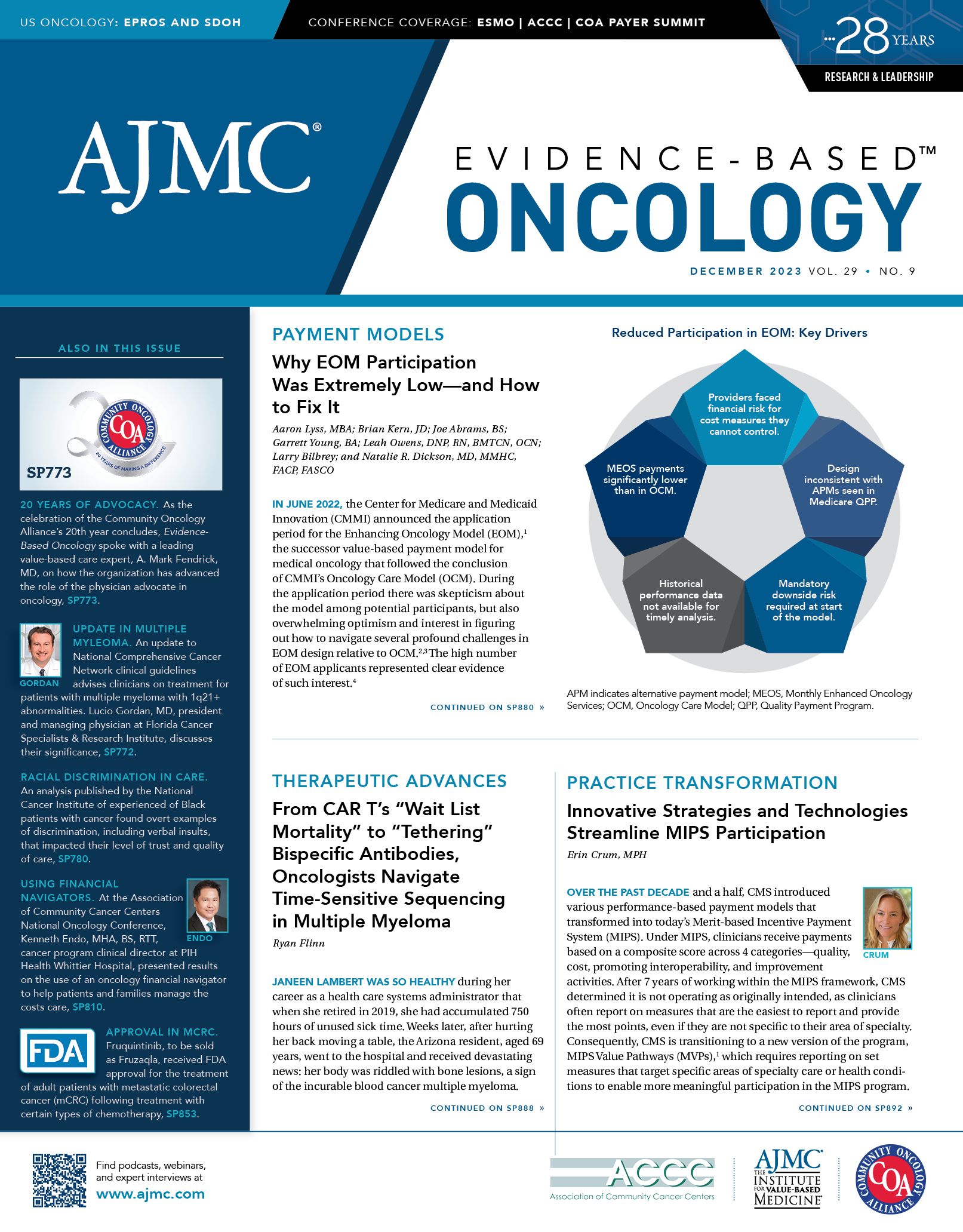
In 2017, that program evolved into what we know today as the MIPS program.3 And that’s when we decided as an organization that we really needed to ramp up our support for practices to be able to participate in regulatory programs in an efficient manner. We asked, how would we help them get beyond just participating to perform well, but to actually move the dial on quality patient care?
So, we went all in on it, and we designed a reporting platform called Practices Insights, which allows practices to view their MIPS data in one consolidated reporting platform; practices can take clinical data directly from the [electronic health record]. Since it’s fully integrated, we pull that data into the reporting platform, and we’re able to compute all of their MIPS quality measures. That means we’ve reduced the burden that required practices to use an outside third-party vendor.
We took that one step further. As I mentioned, we are designing and developing custom quality measures so that our practices are no longer tied to simply reporting the MIPS measures that are available to the regulatory program; we created meaningful, oncology-specific quality measures, such as assessing patients who have stage IV non-small cell lung cancer, and whether they’ve had mutation testing that can inform [the need for] targeted therapies. So, all of a sudden, we’re learning whether patients have had the appropriate mutation tests to guide therapy. Then, we’re ensuring that clinicians are connecting those dots and providing targeted therapy based on test results.
We’ve focused not just on helping practices participate in the MIPS program, but also on figuring out a way for them to do this as kind of a byproduct of ongoing improvements in care. We’re no longer just trying to figure out the program requirements, but we’re focused on things that matter in the policy space, so the practices actually get double credit for it, so to speak.
EBO: With the technology the practices have now, they have the opportunity to monitor almost in real time throughout the year how they’re performing on these quality measures. So, there are no big surprise at the end of the year.
Crum: Exactly. It’s not an afterthought, but it’s not their focus—their focus is on improving care throughout the year.
EBO: How are you tracking progress in addressing health equity?
Crum: We’ve recently released our NCCN Distress Dashboard.1 This enables practices to monitor different areas of social needs for patients and to document that within the medical record directly. In addition, we’re enabling practices to have greater insight into screening rates for patients. There’s a MIPS measure that is the screening rate for SDOH. And we’re planning to roll that out in the beginning of the year, which will tie in nicely with the NCCN Distress Thermometer. Practices can queue up a list of patients for practices to understand which patients have had distress screening and which patients have had positive results that required intervention. Practices will then be able to track and close the loop to connect with patients based on their areas of need.
EBO: Another area of focus is the MIPS Value Pathways (MVP). Can you tell us about this?
Crum: Another component of what I do on behalf of our practices is look for partnerships. A few years ago, we worked collaboratively with American Society of Clinical Oncology (ASCO) to develop and write the proposal for the Advancing Cancer Care MVP, to help identify which quality measures we felt were meaningful in the oncology space, which improvement activities made sense, and to help create the packet of measures that are included in the Advancing Cancer Care MVP. So, we collaborated on that proposal to CMS.
CMS actually said, “This is wonderful, we want to collaborate with you both. Can you help us figure this out?” And so, for a good period of time, we were having calls with CMS to help them bring the Advancing Cancer Care MVP to life. I think that’s a huge win for us to be able to partner with ASCO and have that voice to guide the direction of what we know now is the new regulatory program with the MVP.
In addition, we have worked with ASCO to be their trusted technology partner to bring some ASCO quality measures to life. ASCO had been working with other vendors to bring those measures to the MIPS program, but they were finding that no other registry had the same capabilities with an integrated EHR system that was oncology specific. So, they weren’t actually getting any data or any participants to actually submit those measures for MIPS. We were uniquely positioned with our item-menu EHR to be able to support those measures fully. We’ve partnered with ASCO in 2023 to have those measures available for the MIPS program and help them with their proposal to CMS for full measure endorsement. We’re looking forward to working with them more in the future on new quality measurement development by leveraging physicians in The US Oncology Network and their expertise on the ASCO side as well.
References
1. National Comprehensive Cancer Network. Distress Management. (Version 1.2024). NCCN Clinical Practice Guidelines in Oncology. Published October 27, 2023. Accessed November 26, 2023. https://bit.ly/3HSxLPA
2. Anumula N, Sanelli PC, Physician Quality Reporting System. ANJR Am J Neuroradiol. 2011;32(110:2000-2001. doi: 10.3174/ajnr.A2912
Quality Payment Program. Traditional MIPS overview. Accessed November 27, 2023. https://qpp.cms.gov/mips/traditional-mips