- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Implementing ePROs Is the Lift Worth Taking, Basch Says
Coverage from The US Oncology Network Payer Transformation Summit, held September 27-29, 2023, in Atlanta, Georgia.
To hear oncologist Ethan Basch, MD, MSc, tell it, there have been many arguments against the use of electronic patient-reported outcomes (ePROs) in cancer care, but none have held up. The trouble is the evidence keeps getting in the way.1-3
“Patient-centered care should be at the center of how we think about care transformation in oncology,” Basch said. “Like anything, there are naysayers, and there are naysayers about patient-reported outcomes. There are naysayers who feel that we [physicians] know better than our patients do about their symptoms and how to manage them, who feel that patients shouldn’t be doing this. And I think that the evidence is overwhelmingly compelling that not only do patients appreciate doing this, but it’s feasible to roll out in systems.”
Basch

Hudson

Basch, chief of the Division of Oncology and physician-in-chief at North Carolina Cancer Hospital within the University of North Carolina School of Medicine in Chapel Hill, has spent decades studying a simple idea: It makes more sense for patients with cancer to tell us something is wrong at the first sign of trouble. They might avoid a hospital stay, and they might even live longer. Both have turned out to be true.
“Despite our best efforts, as oncologists and as practices, we miss about half of the symptoms that our patients are experiencing,” he said during an interview September 28, 2023, at The US Oncology Network’s Payer Transformation Summit. “People with cancer who are getting treatment experience a lot of symptoms. They are frequently hospitalized for those symptoms, they miss treatment for those symptoms, they have impairments in function and quality of life because of their symptoms. So, the idea of the program is to allow patients to self-report their symptoms—to catch things early, before they become very challenging, and to intervene.”
The arrival of digital tools revolutionized this process. Today, with studies from multiple countries showing the idea is a winner, CMS has embedded the concept in the Enhancing Oncology Model (EOM), the successor to the Oncology Care Model (OCM) that was the leading alternative payment model for cancer practices from 2016 until 2022.4
“I think this is a very exciting opportunity—for practices, for providers, and for patients. And I applaud CMS for including this in the EOM. It’s true—it is a lift—but many things that we do to better our practices or the lives of our patients are a lift.” He offered examples such as clinical pathways, patient portals, and advanced care planning.
The major argument against ePROs has involved the start-up costs: Navigation systems, care enhancements, and triage systems that are needed to make these systems work require money and redeployment of staff, Basch said. “They require investment, they require effort, but we consider these things to be worth it because they benefit our patients,” he said. “When new treatments come out, it is left to practices to figure out the logistics of how to educate patients for infusion therapies. There is a lot of infrastructure that needs to be developed around these therapies, but we do those things because they benefit our patients.”
Implementing ePROs is no different, he said. “These approaches improve the lives of our patients. They improve their quality of life and physical function, drive down hospitalizations, even improved survival in some cases, so I think it’s certainly worth the lift.”
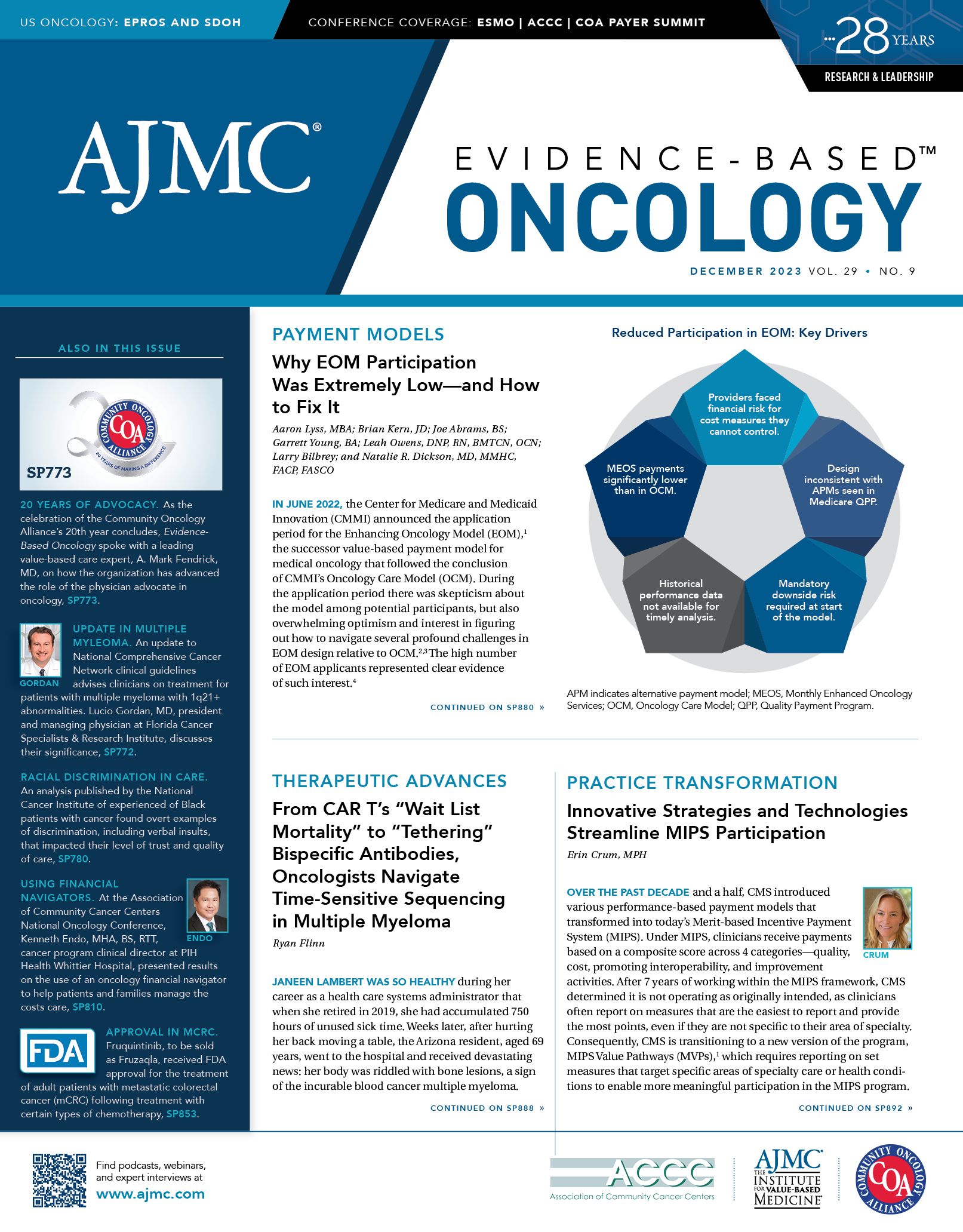
For many reasons (See Cover), EOM has not seen the same uptake as OCM. But Basch said because ePROs offer both Medicare and commercial plans the chance to improve survival and save money, reimbursement is warranted.
Both Basch and Kathryn Hudson, MD, a hematologist/oncologist who is director of survivorship at Texas Oncology, say there is significant front-end work involved in setting up ePROs, but this saves downstream staff time and costs. Patients are less likely to show up at the clinic with uncontrolled symptoms, and they are less likely to end up in the emergency department.
Covering the implementing costs of ePROs would remove one of the main barriers to adoption—which is the reluctance of practices to pay for the technology and staff redeployment needed to make these systems work. In time, he said, population-level analysis of patient data could yield insights for payers, telling them which patients need extra attention based on symptom profile, further driving down costs. This kind of work has already occurred in diabetes management but is just starting in oncology, Basch said.
In the interview, Basch hinted at results that would be presented weeks later at the American Society of Clinical Oncology Quality Symposium; it was the second phase of Texas Oncology’s “Texas Two-Step” study, in which the large practice showed how implementation of an ePRO initiative using Navigating Cancer’s platform produced a 39% reduction in hospitalizations and a $1146 per-patient, per-month average savings.5
“Will this be hard for small practices? I don’t think so,” he said. “There are now multiple technology companies out there that provide the software and the training to do this.”
Hudson, in a separate interview, said developing and implementing an ePRO program takes work. “It takes a lot of forethought, a lot of planning, a need to develop key stakeholders, and a need to develop your nurse triage workforce,” she said, adding that practices can expect to fine-tune their programs over time.
“It’s important to think of this as a quality improvement project, so that you continue to evaluate your progress and make adjustments, so you get the outcomes that you want,” Hudson said. For example, she said, practices want patients to be engaged, but they must seek the right level of engagement. Texas Oncology discovered that patients did not want to be contacted about fatigue, and did not want to be contacted every day for certain chronic symptoms they had learned to manage. As a result, the practice worked with Navigating Cancer to add a “decline-a-call” feature—the symptom was still reported, but there was no call. This increased patient satisfaction and decreased the nursing workload.
Sharing the value of the program—and showing nurses how this work is making a difference for patients—is essential to keeping everyone engaged, Hudson said. “What our nurses are telling us is that, yes, it’s increased their workload a little bit. But they do think it’s valuable, because they’re seeing the impact it’s making on patients firsthand,” she said. “That’s why I think it’s really important to publicize (data) amongst the team and also the patients—so that they have buy-in to stay engaged.”
Every practice must adjust based on its local features and workflow. Hudson said Texas Oncology has had to address the fact that many patients in the state do not have broadband. She also would like to better integrate the tool into the electronic health record. And, from her vantage point overseeing survivorship care, Hudson would like to see more support for mental health care.
“It’s very hard, even with our social workers, to help patients access mental health support,” she said. “We are partnering with different virtual mental health support companies throughout Texas to help support our patients, and we’re hoping to increase access for patients.”
References
1. van den Hurk CJG, Mols F, Eicher M, et al. A narrative review on the collection and use of electronic patient-reported outcomes in cancer survivorship care with emphasis on symptom monitoring. Curr Oncol. 2022;29(6):4370-4385. doi:10.3390/curroncol29060349
2. Basch E, Schrag D, Henson S, et al. Effect of electronic symptom monitoring on patient-reported outcomes among patients with metastatic cancer: a randomized clinical trial. JAMA. 2022;327(24):2413-2422. doi:10.1001/jama.2022.9265
3. Basch E, Deal AM, Dueck AC, et al. Overall survival results of a trial assessing patient-reported outcomes for symptom monitoring during routine cancer treatment. JAMA. 2017;318(2):197-198. doi:10.1001/jama.2017.7156
4. Enhancing Oncology Model. CMS. Accessed November 26, 2023.
https://www.cms.gov/priorities/innovation/innovation-models/enhancing-oncology-model
5. Patt DA, Patel AM, Bhardwaj A, et al. Impact of remote symptom monitoring (RSM) with electronic patient-reported outcomes (ePRO) on hospitalization, survival, and cost in community oncology practice: the Texas Two-Step study. JCO Oncol Pract. 2023;19(suppl 11):569. doi:10.1200/OP.2023.19.11_suppl.569
Evolving Treatment Paradigms for Hematologic Malignancies in Community Oncology Settings
January 11th 2026In an interview during ASH 2025, Ontada's Ira Zackon, MD explores the role of BTK inhibitors in chronic lymphocytic leukemia treatment, highlighting real-world challenges and emerging therapy strategies.
Read More
Exploring Medicare Advantage Prior Authorization Variations
March 26th 2024On this episode of Managed Care Cast, we're talking with the authors of a study published in the March 2024 issue of The American Journal of Managed Care® about their findings on variations in prior authorization use across Medicare Advantage plans.
Listen
