- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
When Choosing Between Bispecifics and CAR T, the Best Therapy May Be What Is Accessible
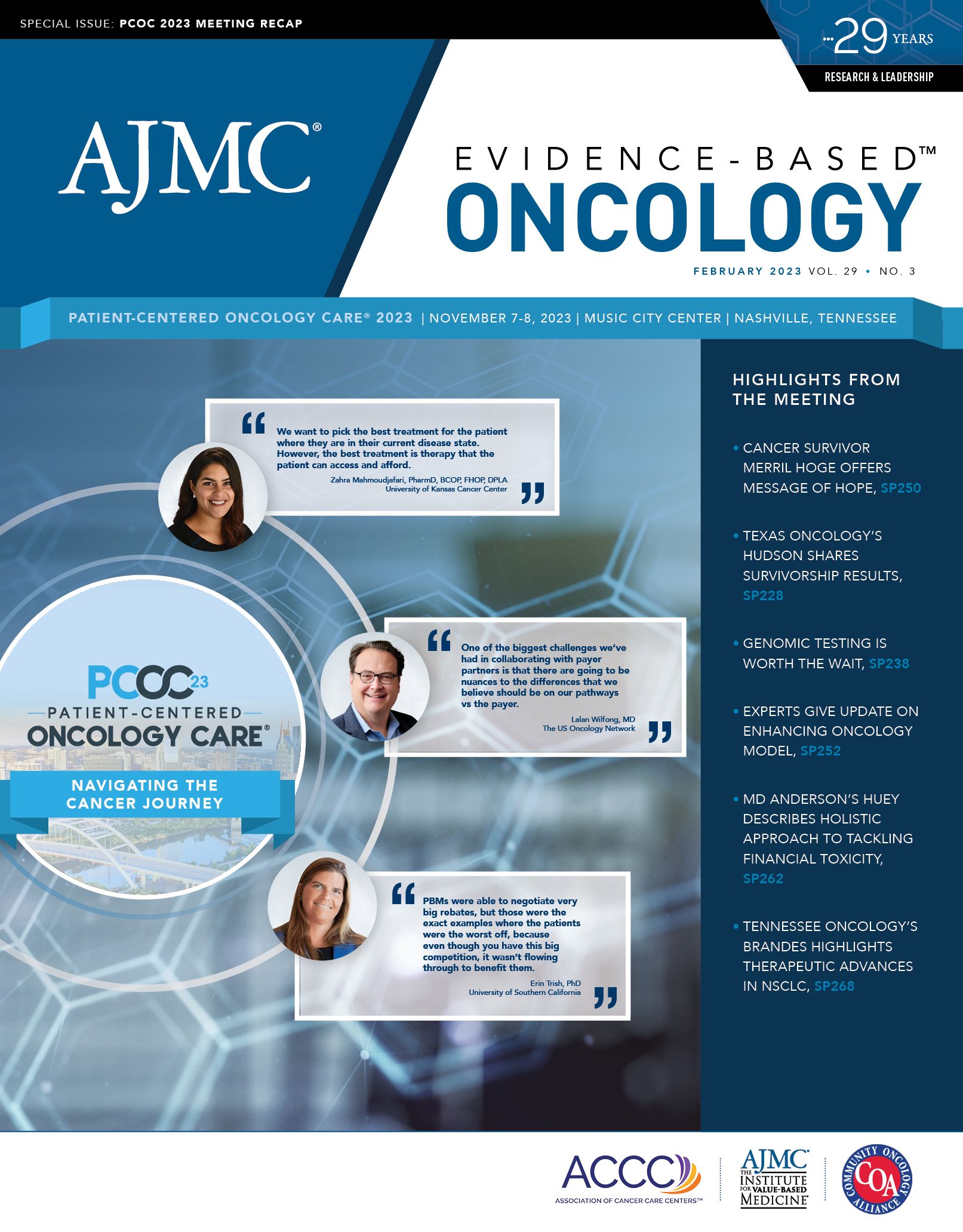
Coverage from the session, "Which Comes First? Bispecifics, CAR T-Cell Therapy, and Cost Consideration in Sequencing,” at Patient-Centered Oncology Care 2023.
The arrival of new therapies to treat patients with lymphoma and multiple myeloma prompts new questions: how should clinicians—and patients—decide which should be used first, or in cases of relapse, which should be next? What are the clinical considerations? Should cost matter?
Ryan Haumschild, PharmD, MS, MBA | LinkedIn photo

Panelists at Patient-Centered Oncology Care (PCOC) 2023 in November took on these topics in the discussion, “Which Comes First? Bispecifics, CAR T-Cell Therapy, and Cost Consideration in Sequencing,” moderated by Ryan Haumschild, PharmD, MS, MBA, director of pharmacy services at Winship Cancer Institute of Emory University in Atlanta, Georgia. Joining Haumschild were as follows:
- Beth Faiman, PhD, MSN, APN-BC, BMTCN, AOCN, FAAN, FAPO, nurse practitioner for the multiple myeloma program, Cleveland Clinic, in Ohio;
- Amitkumar Mehta, MD, associate professor, University of Alabama at Birmingham, director of the lymphoma program and immune effector/CAR T program and medical director, clinical trial office; and
- Zahra Mahmoudjafari, PharmD, MBA, BCOP, FHOPA, DPLA, clinical pharmacy manager, Hematology/BMT/Cellular Therapies, at the University of Kansas Cancer Center in Kansas City.
Haumschild launched the discussion around clinical considerations for therapy selection, but he noted that when it comes to chimeric antigen receptor (CAR) T-cell therapy, “You can’t talk about half-million dollar therapies without talking about cost.” Fellow panelists agreed that cost should not be the first consideration, but it shouldn’t be ignored.
Zahra Mahmoudjafari, PharmD, MBA, BCOP, FHOPA, DPLA | LinkedIn photo

“We want our providers to not have to think about costs [but to instead] focus on efficacy and safety,” Mahmoudjafari said. “We want to pick the best treatment for the patient where they are in their current disease state. However, the best treatment is therapy that the patient can access and afford.”
Amitkumar Mehta, MD | LinkedIn photo

Cost is not the first thing that comes to mind when treating a patient, Mehta said. He explained that the sticker shock at the price of a CAR T-cell infusion overlooks the fact that it’s a single infusion. Other options might require ongoing treatment until a patient progresses, and this can lead to adverse events.
Beth Faiman, PhD, MSN, APN-BC, BMTCN, AOCN, FAAN, FAPO | LinkedIn photo

The bottom line? Cancer is expensive. “There is no doubt there,” Mehta said. “My prime focus is whether the therapy is curative.”
More Therapies, More Innovation
A patient’s disease state and prior treatments are the top factors that drive decisions to use CAR T-cell therapy, a bispecific antibody, or some other treatment, panelists agreed. In diffuse large B-cell lymphoma, CAR T-cell therapy can now be offered in the second line, but in multiple myeloma, Faiman noted, it’s approved for fourth-line treatment. Aggressive myeloma may call for using a bispecific antibody because some patients cannot wait for one of the limited leukapheresis or manufacturing slots each institution receives for CAR T-cell therapy. Patients and caregivers must be educated about managing cytokine release syndrome (CRS) or immune effector cell-associated neurotoxicity syndrome (ICANS).
Mehta said the field has “exploded” with options, which changes the calculation for what’s possible. Today, a clinician may try an antibody-drug conjugate (ADC) if a patient’s disease progresses after CAR T. With ADCs, “we took it to the next level,” Mehta said. “They’re climbing rapidly in the old paradigm of treatment.”
Multiple myeloma now has 2 CAR T-cell therapies, Faiman said, and in 2022 and 2023, the FDA approved 3 bispecific antibodies to treat the disease.1 “The interesting thing about these drugs is that they are all very effective. You’re looking at response rates of about 60% in these heavily pretreated patients,” she said. “Now, we have data that suggest these drugs can be moved earlier in the lines of therapy.”
She added, “I’m trying to refer [patients] with aggressive disease a little bit earlier on in therapy, especially in the context of a well-designed clinical trial because they might have earlier access to those therapies.”
Besides the increased number of therapies, the field has advanced in knowledge of how to manage CRS and ICANS, Mahmoudjafari noted. When CAR T-cell therapy was first approved, she said, “We were all scared of the monster in the closet,” she said. But since then, she added, “We have learned a lot. We’ve adjusted, and we manage that toxicity fairly well,” allowing patients to be treated on an outpatient basis.
“It’s a new paradigm, and it’s exciting,” she said.
Increasingly, where treatment takes place also is a consideration. Haumschild said creating infrastructure (ie, regional care centers) to deliver bispecifics in community settings has been the major innovation for his institution. “At the end of the day, it’s important that more patients get access to these therapies, and the majority of these patients are actually being treated and seen in the community,” he said.
Faiman noted, “One key point I don’t want to forget is patient desire.” Community practice leaders who call the Cleveland Clinic for advice are more likely interested in a bispecific than CAR T-cell therapy. “We take into consideration the financial, the physical, and [whether] patients have caregiver support,” she said.
Therapies That Complement, Rather Than Compete
Mehta said when new therapies come into the market, he is most interested in learning how well they help patients stay in remission. Bringing CAR T-cell therapy into second-line treatment, for example, has helped patients stay in remission longer. In making sequencing decisions, he said, it’s important to understand that different therapies have different targets, and focusing on which target makes sense can guide decision-making. A patient may have had a therapy that targeted CD20, and following progression, targeting CD19 may make sense.
“I think sequencing will evolve,” he said of deciding whether a bispecific or CAR T-cell therapy is right for a patient. “I don’t see them as competing with each other; at the most, I would say they’re complementary to each other.”
In addition, the treatment paradigm is changing so much that a decision that makes sense today may shift as more data arrive—CAR T may move into frontline settings, and that will require different decisions.
Practical Considerations
Mahmoudjafari said her academic center has access to both myeloma CAR T-cell products, all lymphoma CAR T-cell products, and all approved bispecific antibodies. But other centers are less fortunate. “Sometimes your choice is limited to what you have access to,” she said, and creating a center that can deliver all options doesn’t happen overnight.
Patient factors such as tolerability come into play. “If the [adverse] effects are long term, and we’re learning more about the [adverse] effects and toxicity profile of bispecifics, then the way that we choose to sequence them is also a big question mark,” Mahmoudjafari said.
She added, “So many of the conversations that I’ve had with my team and my providers involve, ‘What are our goals? What are we looking to accomplish? And what are the data saying?’” she said. “And it really just boils down to, ‘What does our center have access to? Can [patients] wait long enough for their cells to be manufactured?’”
Haumschild said his academic center weighs the same considerations. Some patients need immediate treatment, and if a patient wants to be treated in the community, bispecifics are preferred. Mahmoudjafari said the ability to get through prior authorization drives decisions, too. “There’s no passing go until you have insurance,” she said.
For academic centers, some quality control is required. Faiman said when a community practice asks about a bispecific, she contacts the manufacturer to make sure the clinic is certified to administer it.
Keeping Patients Engaged
Haumschild said collaboration with community centers is a priority if health equity goals are to be met. This requires uncovering gaps and taking on patient concerns about toxicity, and the need to involve caregivers in treatment decisions. “Something that we’re still trying to understand is shared decision-making,” he said.
There’s been great progress in managing CRS and understanding that each therapy has nuances, Mahmoudjafari said. That said, there’s a lot required to educate patients and caregivers; the latter take on “the significant burden” of medical monitoring, which could be eased by more widespread remote monitoring, she said.
Maintaining relationships with patients and communities takes work, Faiman said. If a patient is referred for a stem cell transplant, receiving the procedure requires 4 to 6 cycles of induction therapy. Just getting to transplant requires keeping track of patients who have already been referred, she said.
“I’m working toward building a survivorship program for patients that would keep that relationship with the community referrals,” she said. “Maybe a Zoom visit or a telehealth visit or a phone call every 6 months to a year to make sure they aren’t falling through the cracks.”
Reference
Flinn R. From CAR T’s “wait list mortality” to “tethering” bispecific antibodies, oncologists navigate time-sensitive sequencing in multiple myeloma. Am J Manag Care. 2023;29(Spec 9);SP888-SP889.