- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Mitigating Financial Toxicity in Cancer Care Requires Policy Reform, Rethinking Benefit Design
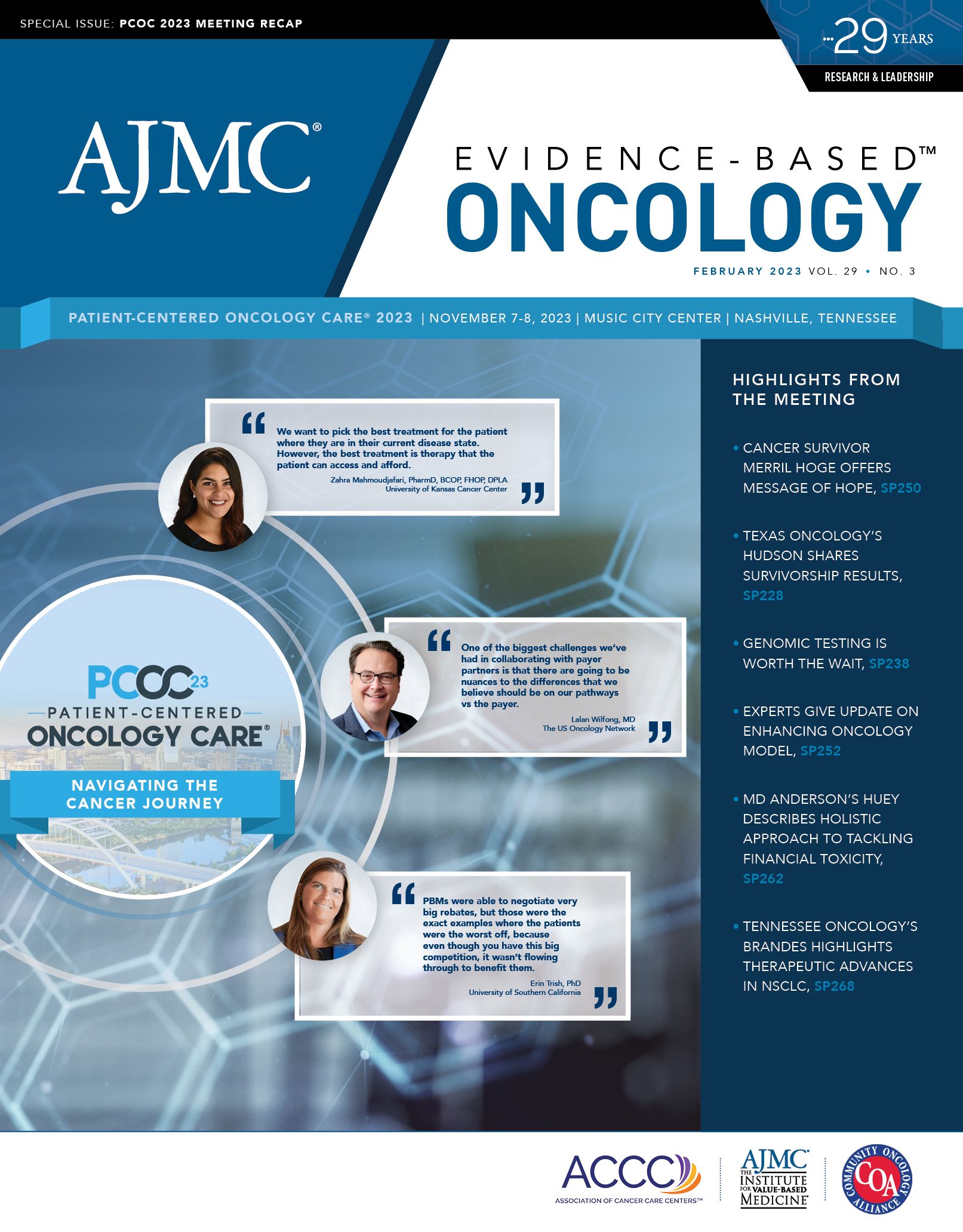
From the panel discussion, "The Burden They Carry," a discussion of the impact of financial toxicity over the duration of the cancer journey.
Payment reform is an ongoing topic of discussion in oncology, where treatments are costly and patients often face financial barriers to optimal care. Addressing the issues that fuel financial toxicity for patients can be challenging given the nuances of health insurance and treatment costs in the US, but it is a necessary endeavor to ensure that all patients who need cancer care can receive it without facing financial struggle.
In a discussion at the 2023 Patient-Centered Oncology Care conference in Nashville, Tennessee, panelists touched on a few of the many aspects of addressing financial toxicity in oncology, both at the payer level and the policy level.
Rajini Katipamula-Malisetti, MD, executive vice president at Minnesota Oncology, moderated the panel, which included the following members:
- Stacie B. Dusetzina, PhD, professor of health policy at Vanderbilt University Medical Center
- Alti Rahman, MHA, MBA, chief strategy and innovation officer for American Oncology Network
- Brian O’Sullivan, a mantle cell lymphoma survivor from Cinnaminson, New Jersey
Rajini Katipamula-Malisetti, MD | Image: Minnesota Oncology

Katipamula-Malisetti began by listing some of the roots of financial toxicity in cancer care, including prior authorization, out-of-pocket requirements, and the many recent oncology drug approvals. While pharmaceutical innovation has provided more options for patients and improved outcomes across cancer types, novel drugs often come with hefty price tags along with the potential for more lines of therapy.
Stacie B. Dusetzina, PhD | Image: Commonwealth Fund

“The amount of spending that we’ve seen has just ballooned,” Dusetzina said. “We do have many more new treatments—those come at a substantial cost to the health care system and to patients themselves. And over time, financial toxicity has evolved to recognize more of the indirect costs. It’s easier to just add up the direct costs of the medical care that people are receiving, and I think there have been better attempts to take into account family and caregiver costs as well.”
Still, there is a lag in considering the costs that are not observable in data being assessed, such as patients who refuse care because they cannot afford to be treated, or those who never pursue treatment or find out about the options available to them, Dusetzina explained. With prescriptions, for example, analyzing data only from those who spent money at the pharmacy in the first place excludes patients who may not have filled a prescription to begin with due to financial concerns.
“[These are] very hard problems to solve, but I think these groups are really important for thinking about the overall financial effect that our system is having on patients,” Dusetzina said.
Alti Rahman, MBA, MHA | Image: AON

Rahman explained that thinking around engagement with the payer ecosystem is one way his team addresses financial toxicity, which often stems from issues related to insurance benefit design and whether patients have insurance. Even those with insurance typically experience fragmented care journeys and various technologies, he added.
“The payer discussions are starting to change in terms of asking questions around, ‘What does primary care look like in your ecosystem?’ I’ve found markets where there is just poor primary care,” Rahman said. “…What we’re seeing is you can have markets where primary care is essentially reduced down to a referral system and not really providing what they need to be.”
From the payer standpoint, it is important to understand the primary care ecosystem and the provider system and how payers fit into the narrative. Factoring in unique quality variables, including mitigation of financial toxicity, is important in negotiations with payers, Rahman noted. In his experience, payers are eager to discuss how quality variables can be factored in because although patients with cancer are the minority, care for this population is notoriously costly.
The Patient Perspective on Financial Toxicity
Brian O'Sullivan | Image: LinkedIn

When Brian O’Sullivan was diagnosed with mantle cell lymphoma in 2021, his specialist recommended treatment with a Bruton tyrosine kinase (BTK) inhibitor. His insurance company would not cover those treatments despite providers appealing the denials over the course of months, all while his blood counts worsened. His third oncologist informed him that the insurance company would cover the treatments only in the second line after O’Sullivan was treated with chemotherapy, which biomarker tests showed would inevitably fail.
“I said, ‘When it fails? So they’re paying twice?’ And he said, ‘Well, in their mind, not everyone makes it past the first round.’ And it just became a number at that point—I wasn’t a name, I was just a number. And I just thought I was going to die.”
He was referred to yet another oncologist, at Memorial Sloan Kettering Cancer Center in Basking Ridge, New Jersey, who was working on a clinical trial of a regimen that included the BTK inhibitor zanubrutinib. When O’Sullivan learned that he qualified for the trial, he put his head down and cried, overcome with newfound hope for healing.
The clinical trial gave him an opportunity to receive the appropriate treatment for his cancer at the right time when his insurance would not have provided coverage. Now, he aims to spread awareness of such options with other patients who may be struggling as he was. While he still faces challenges with the financial aspect of cancer care, he presses on optimistically because his health is what matters most, he said.
O’Sullivan’s story is powerful and it illustrates the challenges that many patients face in the wake of cancer diagnosis. Even for patients on clinical trials, the indirect costs of participation—including lodging, transportation, and time commitments—can quickly add up.
“One of the things that strikes me is just how different a person’s experience can be because of the type of health insurance they have access to, the type of doctors they see, and who they see,” Dusetzina said. “You face the insurance company just saying no outright and you have to go through these older treatments before trying these new ones.”
Dusetzina noted that Medicare, for example, typically covers all cancer therapies and would not necessarily deny coverage of the drug entirely, but would have the patient pay thousands of dollars for the first prescription. The payer-specific, person-specific, and even state-specific difficulties with financial toxicity make it a tough issue to tackle, she said, emphasizing that many current solutions revolve around individual patients seeking assistance to mitigate financial toxicity. However, sweeping policy reform to address financial toxicity is still needed.
Anxiety around the financial aspects of care plagues patients, including O’Sullivan, who recounted receiving bills for costly services ahead of his clinical trial participation that were necessary to properly treat his disease. And whether insurance will cover such bills is not always clear, he said.
Financial toxicity also follows patients post treatment, as survivorship care is a key element of cancer management. Scans and other tests and checkups can be an ongoing financial burden, with maximum out-of-pocket costs and deductibles resetting on a regular basis. While this spending may be less than spending during active therapy, it is more than what an average person would spend and can weigh on patients depending on their insurance coverage and circumstances.
“We have so many people who can’t even access basic cancer care,” Dusetzina said. “…But we also have all of these other services that could help people have greater quality of life and improved outcomes that are also inaccessible right now. And I think we have a lot to do. The first gap is making sure everybody can get initial treatment, but we can’t ignore the fact that survivors have different needs and will have different challenges, and we have to figure out how to accommodate those, pay for those, and make it so there’s not this ongoing financial burden.”
Defining the many holes in the system and identifying potential big policy fixes is a crucial step, Dusetzina explained. One example she outlined is traditional Medicare, which about half of Medicare beneficiaries have. With this coverage, there is no out-of-pocket maximum and many patients have supplemental coverage that they must buy within a fixed amount of time of when they are first eligible. Making these benefits more like typical health insurance is necessary, she said, because paying 20% of cancer care with no out-of-pocket limit is not affordable for most patients.
Expanding Medicaid in states that have not taken this step under the Affordable Care Act is another sweeping policy solution that would mitigate financial toxicity and provide care access to many patients, Dusetzina said.
Looking at major federal payers and how the Inflation Reduction Act has reduced or eliminated out-of-pocket costs for certain high-value services, Rahman suggested that continuing to expand on this type of thinking at the federal payer level is one way to address financial toxicity for patients. He also reiterated the importance of looking at benefit design by region rather than globally.
In closing, O’Sullivan spoke to the need for all patients to receive the most cutting-edge treatments regardless of cost, and all patients should be informed about clinical trials that may give them access to those treatments as oncologists and patients wait for large-scale reform.
With the end goal being affordable access to cancer care for all who need it, the solution is far from simple in the US health care system. But as the panelists illustrated, there is a desire for reform and no shortage of discussion around this crucial issue in oncology.
Editor’s Note: Following the November 7-8, 2023, Patient-Centered Oncology Care meeting, patient Brian O’Sullivan learned that his cancer was in remission. On December 11, 2023, his physician, Anita Kumar, MD, presented results for the trial that enrolled O’Sullivan at the 65th American Society of Hematology Annual Meeting & Exposition. Results of the phase 2 BOVen study showed that the combination of zanubrutinib (Brukinsa), obinutuzumab (Gazyva), and venetoclax (Venclexta) achieved an overall response rate of 76%, with progression-free survival (PFS) of 72% and overall survival (OS) of 75% at 2 years. Median PFS and OS were not reached.1
Reference
Kumar A, Soumerai J, Abramson JS, et al. A multicenter phase 2 trial of zanubrutinib, obinutuzumab, and venetoclax (BOVen) in patients with treatment-naïve, TP53-mutant mantle cell lymphoma. Presented at: 65th American Society of Hematology Annual Meeting and Exposition; December 9-12, 2023; San Diego, CA. Abstract 0738. doi:10.1182/blood-2023-180069
Oncology Onward: A Conversation With Dr Debra Patt of Texas Oncology
August 1st 2023Debra Patt, MD, PhD, MBA, joins hosts Emeline Aviki, MD, MBA, and Stephen Schleicher, MD, MBA, for episode 2 of our newest podcast, "Oncology Onward: Conversations With Innovators and Changemakers in Cancer Care."
Listen
