- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
The Untapped Potential of Principal Care Management in Oncology: Strategies to Drive Improved Performance and Outcomes
The author discusses how Principal Care Management (PCM) enhances oncology care, improves patient outcomes, and boosts reimbursement opportunities for providers, yet remains underutilized.
The cancer care journey is like an iceberg. For patients, providers, and caregivers alike, just a small portion of the entire process is visible from the surface. Hidden below the waterline is an enormous amount of invisible physical, cognitive, and emotional labor.
Patients and caregivers are tasked with navigating a fragmented, complex health system, enduring complicated procedures, and managing the mental health implications of a serious diagnosis. They do this while still juggling their daily responsibilities and relationships outside of their health care concerns.
Pallav Mehta, MD | Image: Reimagine Care

Meanwhile, providers are continually asked to do more with less. This includes assisting patients with their care navigation challenges and socioeconomic barriers to keeping up with the latest treatment protocols in a field where the science is evolving more rapidly than ever.
It is fair to say that none of these groups receives adequate compensation, monetary or otherwise, for the effort they put in to the cancer treatment process. For providers in particular, especially independent practices with staff to pay and businesses to maintain, the basic mechanisms for fee-for-service reimbursement around oncology care are insufficient to support the proactive, holistic, and person-centered services that clinicians are driven to deliver.
Value-based care models, including the former Oncology Care Model (OCM) and its successor, the Enhancing Oncology Model (EOM), as well as Principal Care Management (PCM), have been designed to help change the equation.1-3
By offering additional reimbursement for the clinical and nonclinical services that surround high-quality cancer care, these models aim to make it more viable to break down silos and engage with patients more comprehensively.
Although these programs have produced positive momentum toward the health system’s shared goals of better outcomes, better experiences, and lower costs,4-6 more work remains before providers have enough resources to fully meet their patients’ needs. The first step is understanding all the opportunities to take advantage of existing incentive programs and how to leverage a combination of technology, cultural change, partnership, and workflow optimization to maximize these initiatives’ financial and clinical impact.
PCM is a prime example of an underutilized option for oncology providers. Introduced in 2020 and revised in 2022,7 this model of care now includes 4 Current Procedural Terminology (CPT) codes that enable physicians and other approved clinicians to bill for the wide array of miscellaneous care management services involved in caring for eligible patients with cancer, such as follow-up phone calls or telehealth interactions, chart reviews, arranging referrals for additional services, or overseeing transitions of care.
With a rising number of patients with cancer and a shrinking number of providers available to care for them,8,9 it is crucial for oncology organizations to learn how to make the most of all the reimbursement opportunities available to them, both for their own financial sustainability and for the benefits that comprehensive care management activities can bring to patients.
What Is the Principal Care Management Model?
The PCM model builds on established chronic care management (CCM) scaffolding to enable specialists to engage in care management for patients with a single high-risk chronic condition or multiple chronic conditions but with a focus on a single high-risk condition, such as cancer.10
The qualifying period of illness must be expected to last more than 3 months (and up to a year), require frequent adjustment of medications or care planning, and present an acute risk of decompensation, functional decline, hospitalization, or mortality.
Although other CCM codes are intended to help providers orchestrate care for individuals with multiple chronic conditions that need concurrent care, PCM recognizes that sometimes a single condition becomes the primary focus that requires immediate, intensive action.
The specific goal of PCM is to assist specialty providers with stabilizing patients as quickly as possible. A focused, disease-specific care plan considers the patient’s comorbidities, but this doesn’t always require equal attention to all of them at once. After the episode of care has been addressed, the specialty provider should transfer the patient’s management back to their primary care provider (PCP) and associated care team.
As such, PCM’s 4 CPT codes enable specialty physicians and their staff to document and bill for certain care management services that fall outside the typical clinical care provided to patients (Table10).
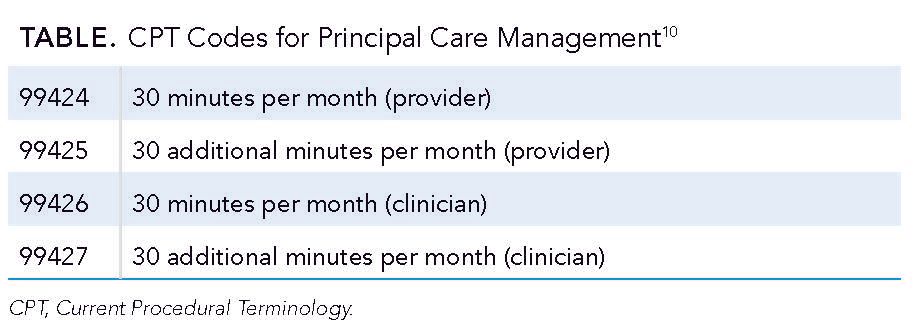
The average reimbursement rate for code 99424 is $80.87, according to the 2025 Physician Fee Schedule, whereas the average rate for 99426 is $61.78. These rates vary according to geographic region and facility.11
Providers can bill these primary codes once a month, as long as they have documented a full 30 minutes of care management activities and add codes 99425 or 99427 as appropriate for additional well-documented services provided under direct physician or qualified health care provider (QHCP) supervision. PCM and CCM codes cannot both be billed in the same calendar month by the same provider.
Why PCM Adoption Lags Despite Clear Benefits
In an uncertain financial environment where razor-thin margins are the norm for many organizations, providers might jump at the chance to enhance their revenue streams with activities that simultaneously improve patient care. Yet the use of CCM codes and complementary transitional care management codes appears to remain below expected levels. Current and comprehensive data are hard to find, but evidence from studies from the years after the initial introduction of these codes in 2015 reveals a relatively slow initial uptake among the physician community.
For example, data from a 2018 study from Brown University showed that in the year after the introduction of CCM, these codes were present in the claims of only 6.47 per 1000 eligible patients in the New England region.12 Finding from a separate study showed that in 2018, a mere 2% to 7% of physicians and 0.3% to 1.3% of nurse practitioners and/or physician assistants billed for CCM.13
CMS has not released specific data on PCM code use. However, it would not be unreasonable to assume that similar trends hold true, especially in a postpandemic era marred by staffing shortages, continuous regulatory changes, and competing priorities.
It is a clearly missed opportunity, especially as many providers have already become adept at performing the type of holistic, proactive care that can be financially rewarded by PCM codes. For example, during the height of the pandemic, the lack of in-person contact reaffirmed the importance of proactive, consistent communication with patients outside of the traditional office visit.
For many providers, it was impossible to simply reschedule a missed office visit to another day. Instead, they were forced to rely on virtual connections and asynchronous communication via video chat platforms and messaging tools. They learned to use these tools out of necessity but continue to use them because they make sense.
At the time, most did not focus on documenting the extra hours devoted to using these methodologies. Oncologists’ only concern was how to continue providing services in a deeply challenging situation. However, certain aspects of this crash course in high-touch care have improved the patient-provider relationship. The fact that providers can get reimbursed for some of these services is just icing on the cake—if they can take advantage of it appropriately.
So why aren’t providers engaging more with these codes? A multitude of barriers exist to PCM uptake, but 3 chief ones are lack of awareness, operational challenges, and financial viability:
- Lack of awareness and skepticism of new models. Value-based care models are evolving rapidly, and programs tend to come and go as the CMS Innovation Center iterates on its learnings. Oncology, in particular, has been a hotbed for pilots and test programs, not all of which have succeeded. Some oncologists may be unable to keep up with all the latest options, or they may feel skeptical that new initiatives will benefit their practices if they have been less than satisfied with their previous attempts to engage in value-driven models.
- Operational complexity and staffing shortages. PCM requires extensive documentation of highly complex care management processes, which takes time and resources that many practices do not have. Providers have also expressed confusion about which clinicians are eligible to bill for which codes, and billing incorrectly could mean having to eat the costs of providing care that will not be adequately reimbursed.
- Concerns over financial viability of participation. Providers may be concerned about an imbalance between the effort required to bill for PCM and the actual reimbursement provided. In addition, research has revealed relatively high denial rates for CCM codes, with approximately 5.4% of all CCM claims denied in 2018,14 which could impact a practice’s decision to adopt care management activities, including those that may be eligible for PCM. Without a perceived return on investment, uptake could remain slow for the foreseeable future.
To overcome these potential issues and take advantage of the opportunity to secure additional revenue, oncology providers must find a way to balance investment and results in their favor.
Some innovative independent oncology practices are finding a way around perceived barriers by integrating PCM billing into their larger practice transformation efforts. For example, one senior leader at a large managed services organization (MSO) shared that targeted training, clear workflows, and ongoing education helped staff get through the learning curve quickly.
After starting to bill for PCM, practices within the MSO were experiencing few denials and increased patient engagement. Once participating practices saw how PCM could benefit patients without overwhelming the workflow, they fully bought into enhancing the care delivery model while achieving improved financial sustainability.
Through technology tools, workflow adjustments, and improved administrative alignment, PCM could become a powerful asset for supporting enhanced care management services for people with cancer.
A Roadmap for Improved PCM Performance
Organizations that can hire additional staff to support care management activities may benefit from doing so. However, more person-hours alone won’t instill positive changes in the holistic and coordinated delivery of care management services. Instead, oncology providers must blend in-person resources with digital ones, including telehealth technologies, data analytics,
and artificial intelligence (AI), to maximize the revenue potential of the PCM model.
Whether building a more robust program internally or partnering with practice transformation experts to accelerate results, practices should consider the following essential elements for developing an effective approach to person-centered care management.
Engaging Patients in a Continuous, Seamless Manner
Identifying and engaging patients suitable for PCM participation starts with being able to stratify individuals by risk and quickly enrolling them in a structured yet flexible program.
Organizations will need data analytics capabilities to conduct systematic symptom monitoring and management, and the virtual and/or in-person capacity to conduct consistent and comprehensive outreach between clinical visits.
Risk stratification tools can be invaluable for identifying the patients most likely to benefit from PCM, including those with advanced-stage disease and multiple comorbidities. An example could be a patient with recurrent breast cancer and chronic obstructive pulmonary disease. Early identification through risk stratification technology can help prompt early enrollment in PCM. Along with regular check-ins and remote symptom tracking, care teams can catch signs of decompensation before they escalate. Swift action will allow the patient to avoid a hospital stay while remaining connected to their care team.
These data-driven approaches should create a frictionless experience for patients and their caregivers. They should include managed consent and enrollment processes, as well as in-demand features such as online scheduling, asynchronous communication with the care team, and educational resources and care plan documents presented in
accessible language.
Simplifying Documentation, Billing, and Other Administrative Tasks
Digital capabilities will also be essential for managing the administrative work in documenting and billing under PCM codes. Providers must ensure they fully understand which staff members can provide PCM services, how to document them appropriately, and how to manage potential denials and resubmissions.
For example, AI-enabled documentation tools are becoming an attractive option for providers who need to extract specific information to meet reimbursement criteria. By integrating AI into the electronic health record (EHR) to support PCM billing, providers can save nurses hours each week by automatically flagging patient symptoms and compiling documentation that meets billing criteria. This turns a burdensome task into a more streamlined, accurate process that improves billing consistency.
Integrating these tools into the EHR and any patient-facing communication platforms that may collect information about symptoms or care processes can provide critical support for coding and create a more complete and accurate portrait of a patient’s progress and needs.
Leveraging Insights to Foster Continuous Improvement
Employing data analytics tools to track actionable patient data and generate reports on the impact of various care management services can assist with making refinements to processes, trimming costly inefficiencies, and finding creative ways to make care teams more proactive and effective over time.
This may include identifying avoidable fragmentation in the care process or highlighting opportunities to offload specific tasks to external partners to ensure that in-house staff can engage patients in consistent, meaningful relationships.
After a few months of PCM, for example, a colleague noticed through their analytics dashboard that certain patients were missing follow-ups after virtual symptom checks. That insight allowed the colleague to rework their follow-up workflow and ensure every flagged symptom prompted a same-day response. Similar small changes have made a noticeable difference in patient satisfaction and helped avoid unnecessary emergency department (ED) visits.
Demonstrating Success With Measurable Outcomes
PCM participation can have many different benefits, both for providers and patients. To make the wisest and most impactful investments, oncology practices will need to identify which outcomes are most important to them and ensure that they are collecting the right data to accurately measure those key performance indicators. These key performance indicators could include a reduction in unplanned visits to the ED, an uptick in patient satisfaction scores, a reduction in staff hours devoted to manual tasks, or financial savings across one or more areas of the organization.
Those engaging with third-party partners to augment internal resources and conduct certain care management activities will also need a strong sense of how to measure the success of their relationships, whether via the financial incentives accrued, metrics around improved patient outcomes, or improvements in patient experience and satisfaction measures.
Conclusion
PCM presents a valuable opportunity for specialists such as oncology practices to improve their relationships with patients while securing additional financial support for the largely invisible labor of care management surrounding the cancer treatment journey.
Although uptake may be slower than desired due to perceived limitations on resources and previous poor experiences with value-based care, new technologies and innovative care strategies have emerged that can help to write a new chapter in patient-centered cancer treatment.
With digital tools and intelligent workflows, oncologists can see meaningful results for their practices and patients through better care coordination, improved outcomes, and enhanced financial sustainability.
Author Information
Pallav Mehta, MD, is a medical oncologist/hematologist with expertise and interest in breast cancer and integrative oncology and is board certified in medical oncology, hematology, and integrative medicine with previous board certification in internal medicine. He is an assistant professor of medicine at Cooper Medical School of Rowan University, and director of integrative oncology and practice development at MD Anderson Cancer Center at Cooper in Camden, New Jersey. Mehta, medical director of Reimagine Care, was also chief of the Division of Hematology/Oncology and director, Medical Oncology for Redeemer Health in partnership with MD Anderson Cancer
Center at Cooper.
References
1. Oncology Care Model. CMS. Accessed July 22, 2025. https://www.cms.gov/priorities/innovation/innovation-models/oncology-care
2. Enhancing Oncology Model. CMS. Accessed July 22, 2025. https://www.cms.gov/priorities/innovation/innovation-models/enhancing-oncology-model
3. Medicare Learning Network. Chronic Care Management Services. CMS. June 2025. Accessed July 22, 2025. https://www.cms.gov/files/document/chroniccaremanagement.pdf
4. Mullangi S, Ukert B, Devries A, et al. Association of participation in Medicare’s Oncology Care Model with spending, utilization, and quality outcomes among commercially insured and Medicare Advantage members. J Clin Oncol. 2025;43(2):133-142. doi:10.1200/JCO.24.00502
5. Caffrey M. With Thyme Care partnership, AON achieves $6M in savings in EOM’s first performance period. Am J Manag Care. 2025;31(5):SP249.
6. Raths D. Why Memorial Herman is expanding a cancer care partnership. Healthcare Innovation. September 4, 2024. Accessed July 22, 2025. https://www.hcinnovationgroup.com/population-health-management/care-management/article/55137680/why-memorial-hermann-is-expanding-a-cancer-care-partnership
7. Principal Care Management (PCM) CPT code billing summary. HealthSnap. Accessed July 22, 2025. https://healthsnap.io/resources/pcm-billing-overview/
8. Collins S. 2024—First year the US expects more than 2M new cases of cancer. American Cancer Society. January 17, 2024. Accessed July 22, 2025. https://www.cancer.org/research/acs-research-news/facts-and-figures-2024.html
9. Cavallo J. Tackling the challenges of oncology workforce strategies, increased patient demand, and rising costs of care: a conversation with Barbara L. McAneny, MD, FASCO, MACP. The ASCO Post. January 25, 2024. Accessed July 22, 2025. https://ascopost.com/issues/january-25-2024/tackling-the-challenges-of-oncology-workforce-shortages-increased-patient-demand-and-rising-costs-of-care/
10. Change reporting habits for Principal Care Management. Codify by AACP. September 17, 2021. Accessed July 22, 2025. https://www.aapc.com/codes/coding-newsletters/my-general-surgery-coding-alert/cpt-2022-change-reporting-habits-for-principal-care-management-170217-article
11. Search the Physician Fee Schedule. CMS. Updated October 17, 2024. Accessed July 22, 2025. https://www.cms.gov/medicare/physician-fee-schedule/search
12. Gardner RL, Youssef R, Morphis B, DaCunha A, Pelland K, Cooper E. Use of chronic care management codes for Medicare beneficiaries: a missed opportunity? J Gen Intern Med. 2018;33(11):1892-1898. doi:10.1007/s11606-018-4562-z
13.Annis A, Hong HG. Utilization of Medicare’s chronic care management services by primary care providers. Nurs Outlook. 2023;71(1):101905. doi:10.1016/j.outlook.2022.12.001
14. Reddy A, Marcotte LM, Zhou L, Fihn SD, Liao JM. Use of chronic care management among primary care physicians. Ann Fam Med. 2020;18(5):455-457. doi:10.1370/afm.2573
Exploring Medicare Advantage Prior Authorization Variations
March 26th 2024On this episode of Managed Care Cast, we're talking with the authors of a study published in the March 2024 issue of The American Journal of Managed Care® about their findings on variations in prior authorization use across Medicare Advantage plans.
Listen
