- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
The Struggle Between Oncology Care Cost and Value
While cost is an important component of value, it tells only a small part of the cancer care story. By focusing on issues of payment and cost alone, we miss our opportunity to engage cancer care stakeholders in the process of creating a more effective system of care.
Since the passage of the Affordable Care Act (ACA), there has been a push by numerous stakeholders to reduce healthcare costs while enhancing value delivery to patients. In many areas of medicine, both goals can be achieved by reducing inter-physician variability in care delivery and giving providers incentives to consistently apply best practices on a population basis. The cancer care model, however, is different and far less amenable to this approach. For many patients with advanced- stage or high-risk cancers, there is no clear standard of care. For others, the emergence of genetic and molecular testing has shown that what was previously believed to be one type of cancer may represent dozens of molecular subtypes, each requiring a profoundly different therapeutic approach.
Additional factors that contribute to rising cancer care costs include the aging population, astronomical increases in pharmaceutical costs, increasingly complex multimodality care, and advances in surgical and radiotherapeutic technology. Costs are further inflated through non—value-added care delivery mismatches, and increasingly expensive end-of-life care. As a result, the National Cancer Institute projects that cancer care costs will increase by 27% between 2010 and 2020, rising to an estimated $158 billion annually.1 The implications of these rising costs are beyond societal—they have an increasingly personal impact on patients. The rising burden of cancer care costs shouldered by patients and their families has led to the coining of the term “patient financial toxicity.”2
The tension between controlling rapidly-growing cancer care costs and the need to enhance oncology valuedelivery has, therefore, been escalating. Numerous stakeholders, including patients, families, physicians, payers, managed care plans, pharmacy benefits managers, employers, and the government, are deeply invested in trying to navigate this conundrum. Each has a unique perspective that may not be fully informed by that of the other stakeholders, and the task is rendered all the more difficult by 3 key factors:
- The standard of care for treating patients with cancer is a rapidly moving target.
- There is no clear consensus on what constitutes value in cancer care.
- Information is siloed and frequently inaccessible; as such existing metrics for cancer care performance and patient outcomes are very poor indicators of actual value delivery.
While most stakeholders are willing to accept that cost is not the sole determinant of value delivery, both our language and tools for fully defining what constitutes value-based cancer care are in their infancy. This process is further challenged by the fact that data collection by billing codes provides vanishing little information regarding the appropriateness, effectiveness, or patient-centeredness of care. Electronic medical records have also been of limited use in accessing essential care data, because much of that data remains trapped within paper records that can only be mined at enormous cost and inconvenience. The way out of this conundrum begins with robust, multi-stakeholder deliberations on ways to contain costs and promote healthcare innovations while creating a system that allows for the economically sustainable practice of personalized medicine.
A number of stakeholders have made important forays toward addressing these complex issues. These include the National Comprehensive Cancer Network (NCCN), whose Evidence Blocks provide a formulation for comparing the relative effectiveness and value of differing therapeutic regimens,3 and the American Society of Clinic Oncology’s (ASCO) Value Framework, which includes an important acknowledgment of a patient’s financial toxicity as a risk of cancer care.4 On the data side of the equation, Flatiron is one of several companies attempting to convert all of the data contained in healthcare records into information that can effectively inform stakeholder discussions.5
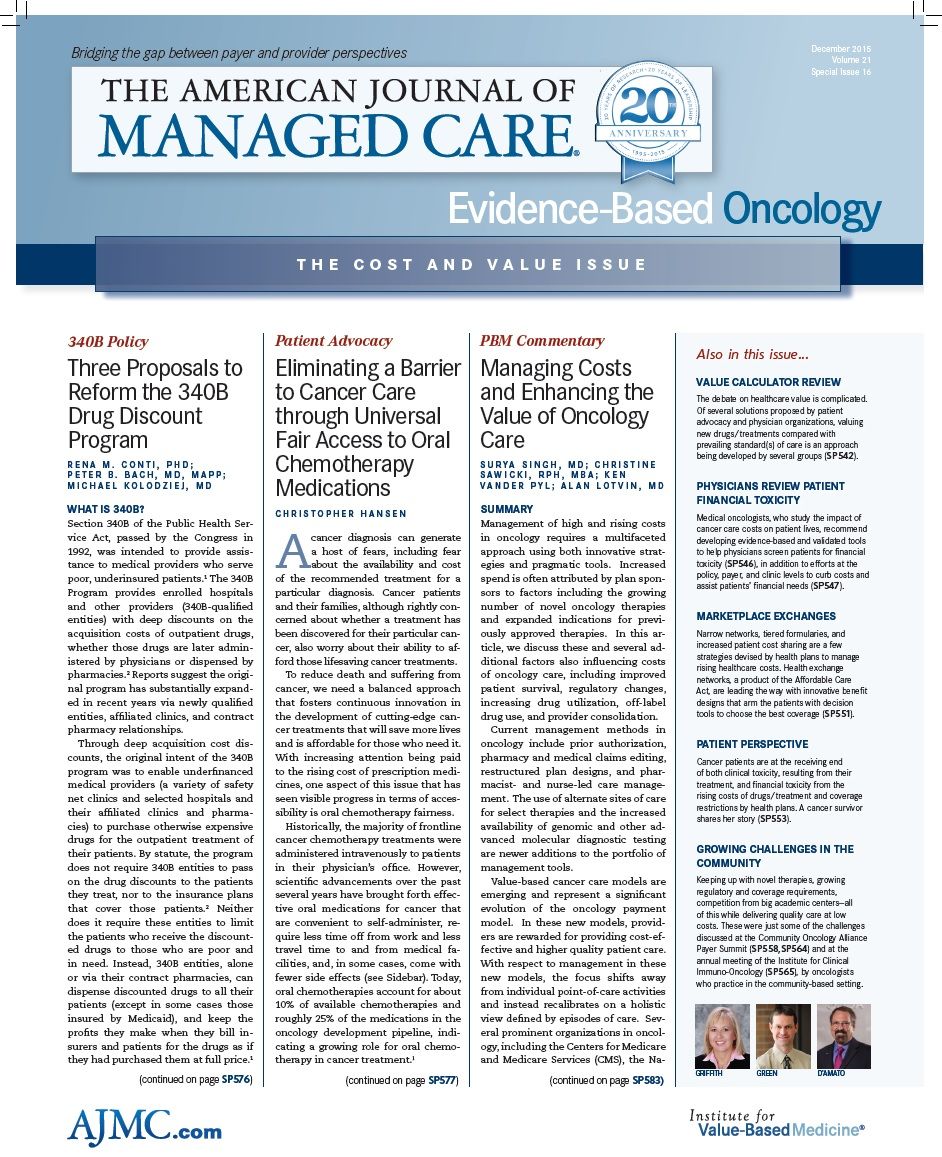
Evidence-Based Oncology’s mission is to further advance the conversation among stakeholders, so that we can create effective responses to the cancer cost/value conundrum. In this issue, Dr Bruce Feinberg of Cardinal Health reviews some of the new value calculators related to the cost versus value debate. Dr Veena Shankaran of the University of Washington and Dr Jonas de Souza of the University of Chicago review the patient burden of cancer care costs. Dr Constantine Mantz reviews the importance and effectiveness of developing a greater collaboration between providers and cancer care facilities.
While cost is an important component of value, it tells only a small part of the cancer care story. By focusing on issues of payment and cost alone, we miss our opportunity to engage cancer care stakeholders in the process of creating a more effective system of care. Given the breadth of stakeholders and the complexity of cancer care in the United States, cost-effective care that is robust enough to empower personalized medicine solutions can only be achieved by engaging stakeholders in a process that increases the “systemness” of care.6 The term “systemness” refers to a model of care in which all of the constituent parts function with maximum transparency, efficiency, effectiveness, and patient centeredness. It is this quest for perfect alignment of people, resources, information, and capital that forms the basis for a sustainable care delivery system.7
EBO
At the recent Patient-Centered Oncology Care meeting in Baltimore,8 hosted by The American Journal of Managed Care, stakeholders had an opportunity to gather and discuss these issues from a multi-stakeholder perspective that provided an excellent foundation for understanding the cost conundrum, and also pointed a way forward. What we ultimately seek is a cancer care delivery system that places patients’ risk-adapted care needs first, creates systems to ensure economically sustainable care delivery, and provides each stakeholder with the information necessary to bring such a system to life. Joseph Alvarnas, MD, is associate clinical professor and director of medical quality and qualtity, risk, and regulatory management, City of Hope. Dr Alvarnas is also the editor in chief of Evidence-Based Oncology.
REFERENCES
1. Cancer costs projected to reach at least $158 billion in 2020 [press release]. Bethesda, MD: National Institutes of Health; January 12, 2011. http://www.nih.gov/newsevents/ news-releases/cancer-costs-projected-reach-least-158-billion-2020.
2. Ubel PA, Abernethy AP, Zafar SY. Full disclosure— out-of-pocket costs as side effects. N Engl J Med. 2013;369(16):1484-1486.
3. NCCN unveils Evidence Blocks for CML and multiple myeloma. National Comprehensive Cancer Network website. Accessed November 25, 2015. http://www.nccn.org/ about/news/newsinfo.aspx?NewsID=546
4. Schnipper LE, Davidson NE, Wollins DS, et al. American Society of Clinical Oncology statement: a conceptual framework to assess the value of cancer treatment options. J Clin Oncol. 2015;33(23):2563-2577.
5. Flatiron website. http:// www.flatiron.com. Accessed November 25, 2015.
6. What policymakers need to know about “systemness” in health care. Kaiser Permanente Institute for Health Policy website. http://www.kpihp.org/wp-content/uploads/ 2012/12/In_Focus_HC-systemness-020708.pdf. Published January 2008. Accessed November 25, 2015.
7. Porter ME and Lee TH. The strategy that will fix healthcare. Harvard Business Review. https://hbr.org/2013/10/ the-strategy-that-will-fix-health-care. Published October 2013. Accessed November 25, 2015.
8. Patient-Centered Oncology Care 2015. The American Journal of Managed Care website. http://www.ajmc.com/meetings/ past-event/PCOC15. Accessed November 27, 2015.