- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
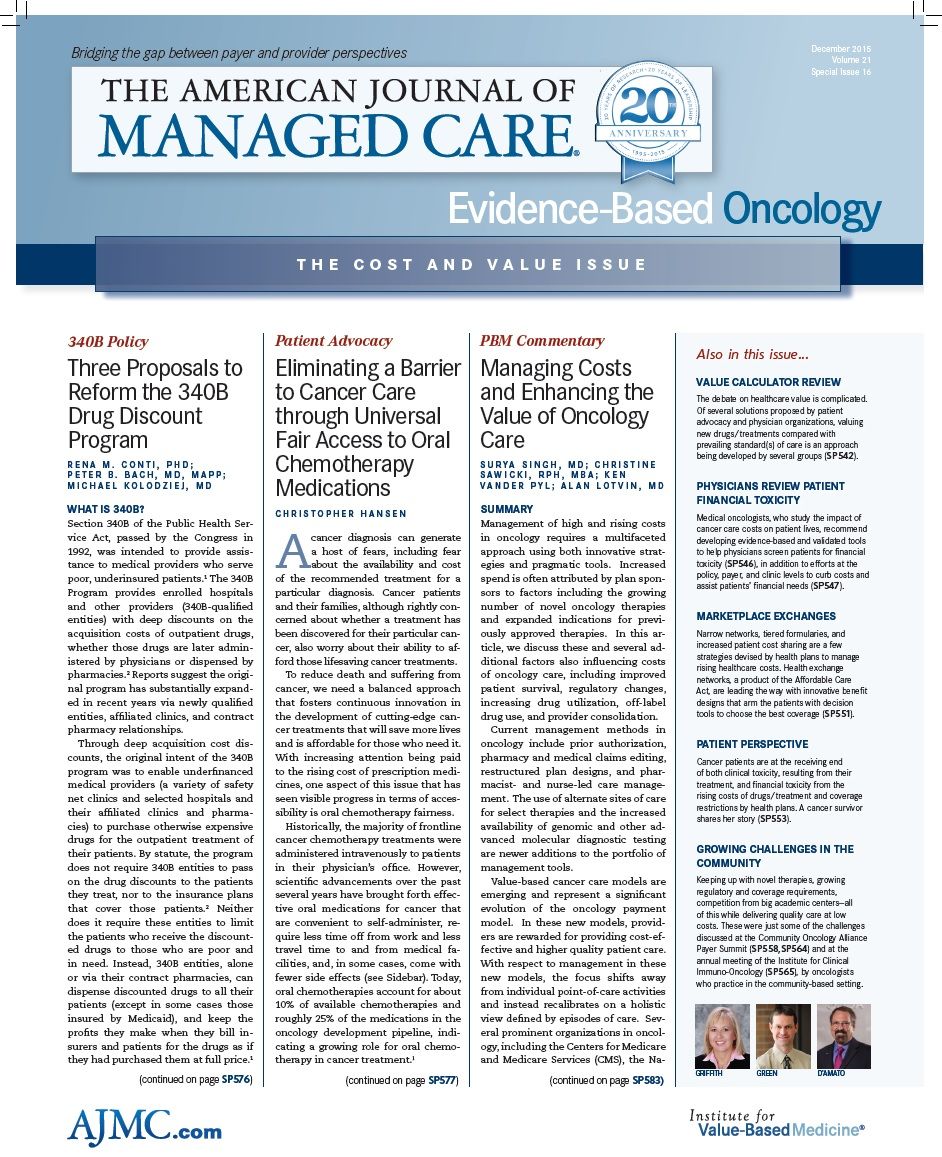
Managing Costs and Enhancing the Value of Oncology Care
Management of high and rising costs in oncology requires a multifaceted approach using both innovative strategies and pragmatic tools. In this article, we discuss several factors that influence the costs of oncology care.
SUMMARY
Management of high and rising costs in oncology requires a multifaceted approach using both innovative strat­egies and pragmatic tools. Increased spend is often attributed by plan spon­sors to factors including the growing number of novel oncology therapies and expanded indications for previ­ously approved therapies. In this ar­ticle, we discuss these and several ad­ditional factors also influencing costs of oncology care, including improved patient survival, regulatory changes, increasing drug utilization, off-label drug use, and provider consolidation.
Current management methods in oncology include prior authorization, pharmacy and medical claims editing, restructured plan designs, and phar­macist- and nurse-led care manage­ment. The use of alternate sites of care for select therapies and the increased availability of genomic and other ad­vanced molecular diagnostic testing are newer additions to the portfolio of management tools.
Value-based cancer care models are emerging and represent a significant evolution of the oncology payment model. In these new models, provid­ers are rewarded for providing cost-ef­fective and higher quality patient care. With respect to management in these new models, the focus shifts away from individual point-of-care activities and instead recalibrates on a holistic view defined by episodes of care. Sev­eral prominent organizations in oncol­ogy, including the Centers for Medicare and Medicare Services (CMS), the Na­tional Comprehensive Cancer Network (NCCN), Memorial Sloan-Kettering Can­cer Center (MSKCC), and the American Society of Clinical Oncologists (ASCO) have created and launched new tools and initiatives intended to help facili­tate the adoption of value-based cancer care models.
BACKGROUND
Cancer care represents a central source of growth in spending on specialty med­ications. Approximately 29% of health care costs in the United States stem from oncology, which has seen spend­ing grow at a rate of 15% annually.1 De­spite the prominence of oncology, how­ever, the marketplace has not coalesced around a unified, effective, and scalable approach to oncology trend manage­ment. It is clear that a multifaceted and adaptable approach is necessary to help ensure that patients have access to high-quality compassionate cancer care that minimizes waste and inappropriate use of resources, while simultaneously taking full advantage of ongoing sci­entific advances and multidisciplinary, well-coordinated care.
DIAGNOSIS OF INFLATION
FIGURE 1
The high and rising cost of oncology medications is buoyed by several factors (), which include:
• Drug development pipeline
• Improved rate of survival
• Regulatory process changes
• Drug utilization variation
• Off-label drug utilization
• Oncology practice and hospital con­solidation
Drug Development Pipeline
FIGURE 2
The robust drug development pipeline includes more than 5400 products in clinical development, with an estimated 55% for use in oncology. This includes both new molecular entities and ex­panded indications based on additional clinical studies of approved drugs or combinations of drugs. Approximately 45% of new molecular entities are first-in-class therapies, with 80% of these for use in oncology.2 The number and breadth of oncology medications en­tering the market each year continues to expand, with many more drugs cur­rently in various phases of development ().3,4
Improved Rate of Survival
Survival rates for several cancer sub­types, including some in breast and lung cancer, have increased in recent decades. The overall 5-year relative survival rate for female breast cancer patients has improved from 75% in the 1970s to 90% in the 2000s.5 This in­crease in survival is largely attributed to improvements in treatment (hormonal treatment and molecularly targeted therapies) and earlier diagnosis from screening (driven by the widespread use of mammography).6 The 1-year relative survival for all lung cancers combined increased over the same 30-year time span from 34% to 45%, largely due to im­provements in surgical techniques and combined therapies.7
Regulatory Process Changes
FIGURE 3
In recent years, the pipeline has deliv­ered new oncology treatments, almost all of which have been “targeted thera­pies,” or drugs aimed at a specific mo­lecular target within tumor cells. The speed with which some novel treat­ments and expanded indications have reached the market has been quickened by the “Breakthrough Therapy” designa­tion created by the FDA in 2012, further increasing the total spending on oncol­ogy ().8,9 The advocacy group Friends of Cancer Research reports that 133 of the 304 total requests between 2013 and 2015 for breakthrough status have been granted by the FDA. Of these 133, there have been 30 approvals, 14 of which are cancer treatments (46.1%).10 Looking forward, there are 36 antici­pated approvals for cancer treatments in the remainder of 2015 and 2016, 3 of which are for breakthrough-designated treatments.
Drug Utilization Variation
The high degree of drug-utilization variation between oncology practices is another factor driving the cost of cancer care. In a study of 2012 data for Medi­care beneficiaries, researchers analyzed administrative claims to evaluate varia­tion in the use of chemotherapy and supportive care agents, acute hospital­izations, and advanced imaging among 1534 oncology practices. Between the practices at the 25th and 75th percen­tiles, there was a $3866 (26%) difference in the cost of drugs used for cancer treatment (inclusive of chemotherapy, supportive care, and administrative fees for infusions). Cost variation for acute medical hospitalizations (surgical ones were excluded) and imaging were slight­ly larger on a percent basis; however, as the authors pointed out, on an absolute basis, the drug cost variation was by far the largest and most meaningful.11
Off-Label Drug Utilization
While off-label use of chemotherapy is permitted by the FDA, treatment usually includes newer higher-cost therapies and may be administered after comple­tion of an approved protocol. Off-label use is often a major focus of attention in discussions of cancer care economics, but there have been few large-scale pub­lished analyses quantifying the degree of this use. In one of the largest such studies to date, a group from MSKCC used prescribing data for 19,500 cancer patients treated by 570 oncologists, and categorized the utilization of 10 chemo­therapy agents into “on-label,” “off-label and National Comprehensive Cancer Network (NCCN) supported,” and “off-label and NCCN unsupported.” Based on this sample, they found 30% of the utilization was off-label, split into 14% NCCN supported and 16% NCCN unsup­ported.12
Oncology Practice and Hospital Consolidation
Consolidation of providers in the cancer care delivery system has caused many stakeholders to raise concerns about both access and cost. First, consolida­tion often leads to a reduction in the available options for patients to access care. Secondly, the comparatively high cost of care in hospital outpatient cen­ters is likely a driver of this cost trend. In October 2014, based on 6 years of moni­toring, the Community Oncology Alli­ance reported that 544 oncology prac­tices have been acquired by hospitals and 313 outpatient clinics have closed.13 Hospital acquisition of practices results in immediate revenue growth based on the typically higher reimbursement rates for oncology services that hospi­tals have in place with payers.
MANAGEMENT APPROACHES
FIGURE 4
Against this evolving array of cost driv­ers, managed care organizations and pharmacy benefit managers have cre­ated a portfolio approach to oncology management in which 1 or more of several approaches are applied in an ef­fort to increase the value of cancer care delivered to patients. These approaches include the following and have been listed in :
1. Prior authorizations are increas­ingly applied to chemotherapeutic medications in an effort to reduce off-label prescribing of these drugs and utilization that is not support­ed by the NCCN guidelines. During the prior authorization process, in addition to addressing the indica­tion for use of a specific agent, the duration of therapy is also typically addressed, rather than granting long or open-ended authorization intervals.14
2. Claims editing is another approach that is used to ensure payment for on-label dosing and indications. While not uniformly adopted, to be most effectively implemented, edits must be deployed against all oncology drugs whether they are infused, injected, or orally admin­istered, or adjudicated under the pharmacy or medical benefit.
3. Plan design is playing an increas­ingly significant role in oncology management. Recent years have seen the introduction of some fre­quently prescribed generic drugs in oncology (e.g., capecitabine in co­lon and breast cancers), and there is accelerating activity in this area. Coupled with the first biosimilar Zarxio (filgrastim)15 in 2015, there is likely to be an increased need for multi-tiered plan design and po­tential formulary exclusions (with appropriate medical exceptions) in oncology.
4. Care management of oncology pa­tients can be quite complex, but es­sential to achieve high-quality care. During this time, patients rely heav­ily on their health care providers. Further, disease progression and response to treatment vary, which leads to highly individualized pa­tient needs. These complexities ne­cessitate a sophisticated nurse-led care management approach, which provides support to patients in sev­eral areas, including, but not limited to: assessment and management of side effects, compliance with nutri­tional plan and recommendations, interventions for reducing infection risk, and facilitation of end-of-life care discussions.
5. Adherence to oral and infused treat­ments in oncology can be optimized through proactive consultation to identify and address potential barriers to compliance and persis­tence. A comprehensive nurse-led care management approach also includes tools and resources to ad­dress root causes that may lead to non-adherence, such as unrealistic patient expectations, inadequate levels of health literacy, existence of comorbid conditions, concurrent drug therapies, and the need for as­sistance with financial concerns.
The treatment of cancer frequently requires medication infusion and/or in­jection by a clinician, for which a site of care must be selected. This decision is usually made based on the preference of the treating medical oncologist. For some aspects of patient care—including supportive drugs, such as antiemetics and blood cell growth factors—an alter­native site of care for drug administra­tion can be offered, such as home or am­bulatory infusion centers. These sites offer greater comfort and convenience to certain patients, while also being cost effective.
Personalized medicine is an evolving field in which physicians use diagnostic tests to determine which treatments will work best for each patient.16 In breast cancer, a recurrence score based on a 21-gene assay (“Oncotype DX”) has been shown to determine whether chemother­apy, in addition to hormone therapy, will be incrementally beneficial in lymph-node negative, hormone-receptor posi­tive patients. In essence, Oncotype DX allows physicians to identify those pa­tients in the relevant subpopulation who would best respond to chemotherapy (in addition to well-tolerated and relatively inexpensive hormone therapy). This may also help reduce the unnecessary cost of treating non-responders.17 Recently published results from the prospective TAILORx trial of this assay demonstrate that women with low recurrence scores (16% of the studied population) had a 98% survival with hormone therapy alone, as well as a rate of freedom from cancer re­currence of almost 99%, providing sup­port for the clinical validity of this test, and its ability to lower the cost of care when used appropriately.18
EMERGENCE OF VALUE-BASED CANCER CARE MODELS
Sustainably addressing the oncol­ogy cost drivers also requires new ap­proaches that not only incorporate tra­ditional management approaches, but also go beyond the existing methods. Some degree of redesign in how cancer care is delivered is necessary in order to enable the iterative enhancement and measurement of value through new ap­proaches. If providers are expected to meaningfully alter their practice pat­terns, they must be rewarded for higher quality and/or more efficient care. In­stead of simply paying more for greater volume for individual point of care ac­tivities, the focus should be more holis­tic, at the patient or episode level. While experimentation with 2 such models— cancer care pathways and bundled pay­ments for cancer episodes of care—have been most popular, other models and tools aimed at enhancing the value of oncology care are emerging.
Cancer care pathways aim to reward providers for performance, offering greater reimbursement for following es­tablished, evidence-based care recom­mendations. Some payers have seen measurable success with pathways while others have experienced barri­ers in pathways adoption. Aetna and The US Oncology Network’s cancer-care management program is one such ex­ample of a pathways program that re­ported a modest reduction in hospital­izations and treatment costs for lung, breast, and colorectal cancers, but the firm evidence for substantial impact on costs attributable to oncology pathway programs has been minimal.19
Payers continue to experiment with bundled payments for all care delivered to patients. Such an approach offers a single payment for the full episode of care, creating incentives to reduce to­tal health care costs. UnitedHealthcare recently reported the results of such a study in 5 medical groups, and their in­tervention also featured a stronger data feedback loop to providers to improve care management. The experiment led to substantially reduced healthcare costs, but paradoxically led to increases in prescription drug spending.20
FIGURE 5
Meanwhile CMS, the nation’s largest payer, has announced its intention to test a value-based approach.21 While it will be challenging for a single com­mercial insurer to create sufficient in­centives to encourage practice change in a given provider community (because any 1 plan only impacts a modest pro­portion of a provider’s population), CMS is the exception. Due to its enormous market share, particularly for Medicare beneficiaries (where the greatest can­cer burden is found), CMS has the abil­ity to promote meaningful change. As part of the value-based approach being pursued, CMS plans to evaluate a model that offers bundled payments for oncol­ogy episodes of care. The test, a prod­uct of the CMS Innovation Center, will be implemented and evaluated, offering the US Department of Health & Human Services Secretary the opportunity to scale the program, nationwide, if there is evidence of cost savings without com­promising the quality of care delivered. CMS’ Oncology Care Model also offers a monthly care coordination payment to practices to support the complex care coordination needs of their cancer pa­tients. Further, CMS has encouraged commercial payers to participate in the model, with the goal of reducing frag­mentation of incentives. Of note, Medi­care’s decision to leave out prescription drugs from total cost-of-care calcula­tions that determine provider payments may weaken incentives to impact pre­scribing practices ().22
Beyond cancer care pathways and bundled payments, additional efforts are underway to help determine the value of cancer care with a focus on assessing cancer drugs and regimens. With patients bearing more of the cost of care, these new efforts seek to pro­vide increased physician and patient education in order to allow for more informed treatment decisions. NCCN, MSKCC, and ASCO have recently intro­duced tools and frameworks for assess­ing cancer drugs to determine the best overall value—value is assessed differ­ently within each tool or framework. The NCCN Evidence Blocks were pub­lished in the NCCN Clinical Practice Guidelines in Oncology for Chronic Myelogenous Leukemia and Multiple Myeloma in October 2015. This tool de­termines value based upon assigning scores to each drug in 5 areas—price, effectiveness, safety, quality, and con­sistency of clinical data.23,24 The tool is meant to supplement the widely used NCCN guidelines for oncology care. The ASCO tool is a points-based framework that defines value based on 3 elements articulated by the Institute of Medicine: clinical benefit (efficacy), toxicity (safe­ty), and cost (efficiency). ASCO believes the 3 elements are readily measured and ascertainable.25 The MSKCC pub­lished a web-based comparative cancer care pricing tool called the DrugAbacus, which provides drug pricing by episode of care based on several attributes and treatment needed to achieve outcomes in published clinical studies. Currently, DrugAbacus includes 54 cancer drugs (approved between 2001 and 2013) with a list of comparative features that in­clude drug efficacy, toxicity, novelty, re­search and development costs, disease incidence, population health burden, treatment duration, and total sales. The DrugAbacus price is a calculation based on values for each comparative feature. Expansion of the drug list, provider, and expert feedback will continue to be in­corporated in future enhancements to the tool.26
EBO
While it may be too soon to fully un­derstand how these new tools for as­sessing value can be used directly or in­directly to inform patient and physician care decisions or shape reimbursement policies, they, along with the other ap­proaches described, must be iteratively refined if we are to truly create a system that supports and incents value-based oncology care.
Surya Singh, MD, is vice president of specialty client solutions and trend management at CVS Health, Lincoln, Rhode Island.
Christine Sawicki, RPh, MBA, is director of specialty clinical innovation and product development at CVS Health, Lincoln, Rhode Island.
Ken Vander Pyl, is director of specialty product development at CVS Health, Florham Park, New Jersey.
Alan Lotvin, MD, is executive vice president for specialty pharmacy at CVS Health, Lincoln, Rhode Island.
Address for correspondence:
Surya Singh, MD
695 George Washington Highway
Lincoln, RI 02865
E-mail:
surya.singh@cvshealth.com
REFERENCES
1. CVS Health, 2015. Analysis of internal data from 2012 to 2014.
2. Innovation in the biopharmaceutical pipeline: a multidimensional view. Analysis Group website. http://www.analysisgroup.com/uploadedfiles/content/insights/publishing/2012_innovation_in_the_biopharmaceutical_pipeline.pdf. Accessed October 12, 2015.
3. Buffery D. The 2015 oncology drug pipeline: innovation drives the race to cure cancer. Am Health Drug Benefits. 2015;8(4):216-222.
4. CVS Health internal pipeline data. September, 2015.
5. Berry DA, Cronin KA, Plevritis SK, et al. Effect of screening and adjuvant therapy on mortality from breast cancer. N Eng J Med. 2005;353(17):1784-1792.
6. Cancer treatment and survivorship facts & figures, 2014-2015. American Cancer Society website. http://www.cancer.org/acs/groups/content/@research/documents/document/acspc-042801.pdf. Accessed October 8, 2015.
7. Howlader N, Noone AM, Krapcho M, et al. SEER cancer statistics review, 1975-2010. National Institutes of Health website. http://seer.cancer.gov/csr/1975_2010/.
8. Sherman RE. Expediting drug development—the FDA’s new “breakthrough therapy” designation. N Eng J Med. 2013;369(20):1877-1880. November 14, 2013.
9. Fast track, breakthrough therapy, accelerated approval, priority review. US Food and Drug Administration FDA website. http://www.fda.gov/forpatients/approvals/fast/ucm20041766.htm. Accessed October 7, 2015.
10. Breakthrough therapies. http://focr.org./breakthrough-therapies. Friends of Cancer Research website. Accessed October 2015.
11. Clough JD, Patel K, Riley GF, et al. Wide variation in payments for Medicare beneficiary oncology services suggests room for practice-level improvement. Health Aff (Millwood). 2015;34(4):601—608.
12. Conti RM, Bernstein AC, Villaflor VM, et al. Prevalence of off-label use and spending in 2010 among patent-protected chemotherapies in a population-based cohort of medical oncologists. J Clin Oncol. 2013;31(9):1134-1139.
13. Community Oncology practice impact report: the changing landscape of cancer care. Community Oncology Alliance website. http://www.communityoncology.org/pdfs/Community_Oncology_Practice_Impact_Report_10-21-14F.pdf. Published October 21, 2014. Accessed April 14, 2015.
14. EMD Serono specialty digest, 11th edition: managed care strategies for specialty pharmaceuticals. EMD Serono website. http://www.specialtydigest.emdserono.com/. Accessed October 29, 2015.
15. Sandoz launches Zarxio (filgrastim-sndz), the first biosimilar in the United States. Novartis website. https://www.novartis.com/news/media-releases/sandoz-launches-zarxiotm-filgrastim-sndz-first-biosimilar-united-states. Accessed October 9, 2015.
16. Personalized medicine 101: improving patient care in the 21st century. Personalized Medicine Coalition website. http://www.personalizedmedicinecoalition.org/Userfiles/PMC-Corporate/file/Personalized_Medicine_101_fact-sheet.pdf. Accessed October 9, 2015.
17. Paik S, Tang G, Shak S, et al. Gene expression and benefit of chemotherapy in women with node-negative, estrogen receptor-positive breast cancer. J Clin Oncol. 2006;24(23):3726-3734.
18. Sparano JA, Gray RJ, Makower DF, et al. Prospective validation of a 21-gene expression assay in breast cancer [published online September 28, 2015]. N Engl J Med. doi:10.1056/NEJMoa1510764.
19. Aetna, The US Oncology Network provide more evidence that clinically proven, integrated cancer care enhances quality and controls costs [press release]. Hartford, CT, and The Woodlands, TX: Aetna and The US Oncology network; December 06, 2012. https://news.aetna.com//news-releases/aetna-the-us-oncology-network-provide-more-evidence-that-clinically-proven-integrated-cancer-care-enhances-quality-and-controls-costs/.
20. Newcomer LN. Changing physician incentives for cancer care to reward better patient outcomes instead of use of more costly drugs. Health Aff (Millwood). 2012;31(4):780-785.
21. Oncology care model. CMS website. http://innovation.cms.gov/initiatives/Oncology-Care/. Accessed April 20, 2015.
22. Medicare advantage value-based insurance design model. CMS website. http://www.cms.gov/Newsroom/MediaReleaseDatabase/Fact-sheets/2015-Fact-sheets-items/2015-09-01.html. Accessed September 1, 2015.
23. Beasley D. New tool will compare costs and benefits of cancer treatments. Reuters website.
http://www.reuters.com/article/2015/08/21/us-usa-healthcare-cancer-idUSKCN0QQ1X820150821. Published August 21, 2015. Accessed October 29, 2015.
24. Nelson, R. NCCN unveils new 'Evidence Blocks' initiative. Medscape website. http://www.medscape.com/viewarticle/853052. Published October 21, 2015. Accessed November, 2015.
25. Schnipper LE, Davidson NE, Wollins DS, et al. American Society of Clinical Oncology statement: a conceptual framework to assess the value of cancer treatment options. J Clin Oncol. 2015;33(23):2563-2577.
26. DrugAbacus. Memorial Sloan Kettering Cancer Center website. http://www.drugabacus.org/methods/. Accessed November 2015.
©2015 CVS Health. All rights reserved. This document contains confidential and proprietary information of CVS Health and cannot be reproduced, distributed or printed without written permission from CVS Health.
This document contains references to brand-name prescription drugs that are trademarks or registered trademarks of pharmaceutical manufacturers not affiliated with CVS Health.
Plan member privacy is important to us. Our employees are trained regarding the appropriate way to handle members’ private health information.