- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
The Promise of Telehealth—a Cautionary Tale
Implications of Telehealth Use on the Future of Oncology Care
Editor’s Note: This is the second installment of a 2-part series on the rise of telehealth during COVID-19 and its implications. Part I appeared on ajmc.com on September 15, 2022. See https://bit.ly/3R3fMaV
Optimizing telehealth post COVID-19 will be a balancing act. Despite its meteoric rise during the height of the pandemic, telehealth’s application in complex, chronic, and/or life-threatening conditions may continue to present challenges.1
Clear opportunities and advantages of telehealth for ambulatory patients or those in remote or rural areas are already evident. Providing diagnostic evaluations and follow-up consultations through virtual visits delivers value and efficiency. Easier and increased access to care may boost medication adherence, which can improve patient outcomes and potentially reduce the overall cost of care.
Many oncology practices embraced telehealth during COVID-19 as a cornerstone of safety for patients with cancer, many of whom are immunocompromised, only to discover added value. Beyond merely limiting unnecessary in-person patient visits to clinics, some practices report a more comprehensive and effective application of telehealth.
An oncologist from a multi-site, community-based practice in Texas shared with the authors:
“We have used [telehealth] to diagnose cancer, support patients through their cancer treatment, modify therapy, and engage caregivers in conversations about diagnosis and treatment. It will forever make high-quality health care more accessible to the patients we serve.”
But extending the concept of at-home care to the administration of medications poses safety and practice management concerns for oncologists. Of note is the relationship-based nature of cancer care, which favors in-person communication, especially for difficult conversations with patients, such as delivery of bad news.
Although standards for use of telehealth in oncology care previously did not exist, oncology care stewards are working together to align on best practices. The American Society of Clinical Oncology published its standards and practice recommendations in September 2021, providing discrete suggestions for topics and services that can be performed in a virtual vs a face-to-face setting.2 Authors of an article published in Clinical Cancer Research point to a future in which virtual visits are augmented by wearable digital tracking devices that provide insightful data.3
More study is needed to better understand the broader impact telehealth can have on outcomes for patients with cancer. In the meantime, it also is important to consider the consequences of an overreliance on telehealth observed in 2020-2021 on current and future diagnoses and prognoses of oncolytic conditions.
The Looming Crisis in Oncology Care
In oncology, telehealth has been essential to the response to COVID-19, enabling aspects of needed care to continue safely for patients. As noted above, the potential benefits of greater integration of telehealth solutions in oncology likely will be an important long-term effect of the COVID-19 pandemic.
Diagnoses and prognoses. A more concerning consequence of the pandemic is the significant decline in cancer screenings and cancer detection, especially in the early months of COVID-19, as patients avoided nonurgent health care activities. As patients return to their prepandemic routine and preventive care, there is a likelihood that cancers will be diagnosed in later stages where the disease has progressed and may be more difficult to manage. The National Cancer Institute (NCI) predicted that this will result in an increase of 10,000 breast and colon cancer deaths over the next decade (Figure).4
Figure.
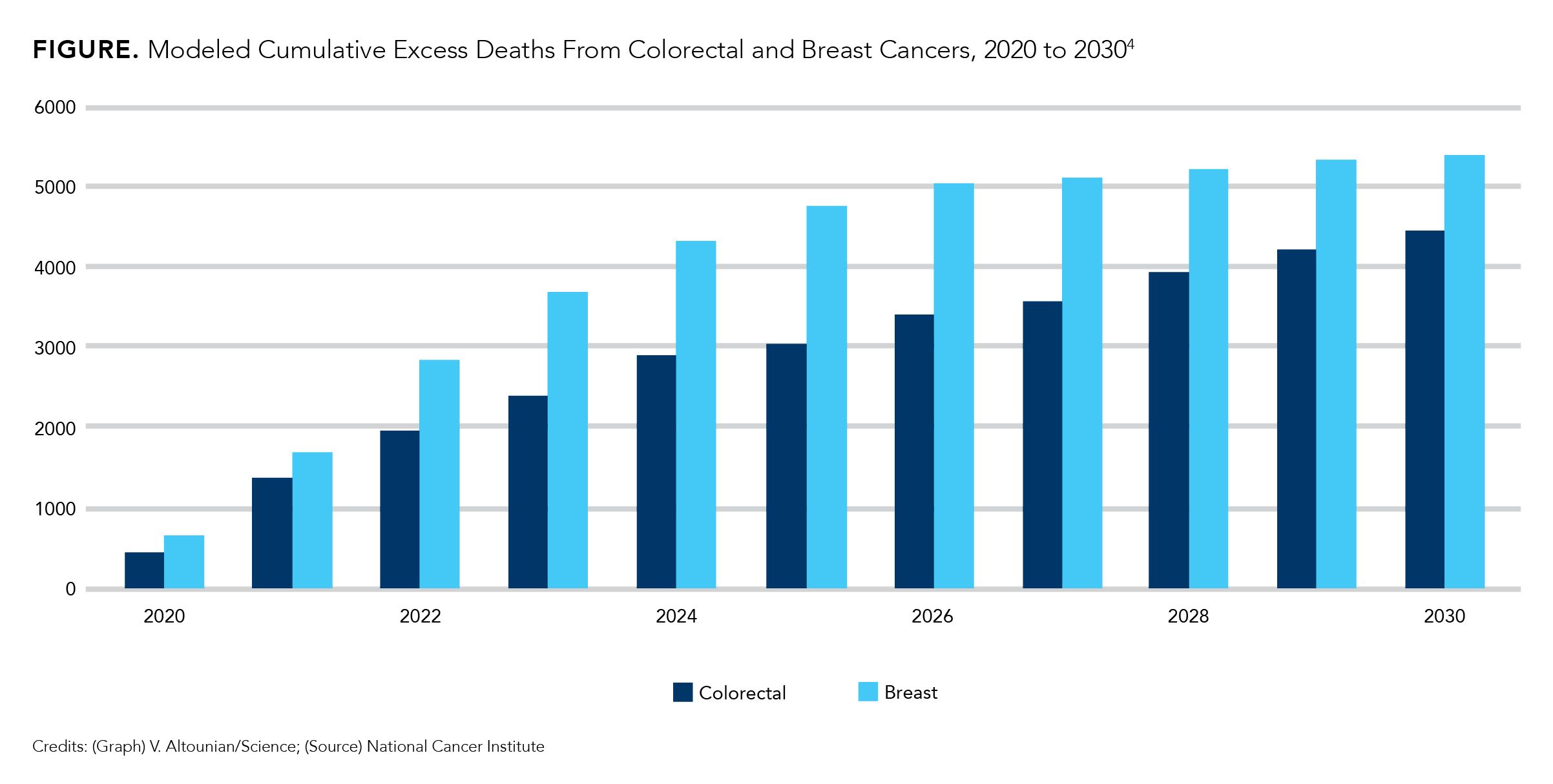
The alarm has been sounded among leading voices in cancer prevention. Then-NCI director Norman E. Sharpless, MD, outlined the problem in a Science column in June 2020: “There already has been a steep drop in cancer diagnoses in the United States since the start of the pandemic, but there is no reason to believe the actual incidence of cancer has dropped. Cancers being missed now will still come to light eventually, but at a later stage (‘upstaging’) and with worse prognoses.”4
In a March 2021 interview with NPR, Therese Bevers, MD, medical director of the Cancer Prevention Center at The University of Texas MD Anderson Cancer Center in Houston, declared, “A woman is more likely to die from an advanced-stage breast cancer than she is from COVID-19.”5
Site-of-care Effects. The increase in patients with later-stage cancer will constitute a lingering pandemic-related disruption in oncology care. Providers and hospital systems must plan for the impact on operations, revenue cycle, and even reputation management as patients experience more challenging illnesses and more deaths.
Total Cost of Care. The cost of care for patients diagnosed with later stages of oncolytic conditions may increase as more robust, complex treatments will be required. Planning for a different oncology care environment could create greater demand for certain drugs, affecting drug production and manufacturing cycles.
Research Innovation. The pace of cancer research also slowed during the pandemic, creating a potential indirect, long-term negative impact if new discoveries are delayed. According to a JAMA Network Open research letter, launches of oncology clinical trials of drugs and biologic therapies decreased 60% for 1 commercial clinical trial platform.6 Delayed research can mean delayed cures, as noted in the letter: “…the COVID-19 pandemic may be associated with longer term indirect effects on population morbidity and mortality through pathways such as arrested drug development.”6
The total impact of delayed diagnoses and increases in frequency and cost of treatments is likely to cause significant challenges for patient outcomes, patient journeys, business operations, and revenue cycles of providers, payers, and manufacturers alike.
Conclusion
Telehealth has provided numerous benefits and advantages to patients and providers during the height of the COVID-19 pandemic, and its value should not be diminished. However, the limitations of virtual health care services, particularly for patients with oncolytic conditions, are likely to have long-term consequences, which have yet to be fully realized.
It is imperative to consider the potential impact on all stakeholders in the health care space:
- Payer and employer organizations should continue to evaluate reimbursement parity for telehealth and in-person visits. They also should plan for a potential increase in total spend in oncology
- Community practices, hospitals, and health systems should evaluate their staffing and infusion chair capacity to ensure they are able to meet increased demand without compromising treatment expediency.
Manufacturers should continue research and development efforts for pipeline therapeutics, but also assess patient assistance programs and other resources they may need to expand to provide appropriate support to patients, providers, and payers. The true impact of the pandemic on oncology outcomes will become evident with time. The ability to strategically plan for likely scenarios and develop flexible and feasible solutions for the potential spike in demand for oncolytic treatments will help secure operational efficiencies necessary for continued excellence in oncology care.
Author Information
Neil Minkoff, MD, served a chief medical officer at COEUS Consulting Group and has been a senior physician leader at Harvard Pilgrim Health Care. Joshua Greenblatt, MFA, is the chief business officer of COEUS Consulting Group. Yana Volman, MBA, is the senior vice president of access strategy and communications with COEUS Consulting Group.
The authors gratefully acknowledge Edward Bryson for editorial assistance.
References
1. Minkoff N, Greenblatt J, Volman Y. Part I: the promise of telehealth – a cautionary tale. The American Journal of Managed Care®.
Published September 15, 2022, Accessed, September 15, 2022.
https://bit.ly/3R3fMaV
2. Zon RT, Kennedy EB, Adelson K, et al. Telehealth in oncology: ASCO standards and practice recommendations. JCO Oncol Pract. 2021;17(9):546-564. doi:10.1200/OP.21.00438
3. Knudsen KE, Willman C, Winn R. Optimizing the use of telemedicine in oncology care: postpandemic opportunities. Clin Cancer Res. 2021;27(4):933-936. doi:10.1158/1078-0432.CCR-20-3758
4. Sharpless NE. COVID-19 and cancer. Science. 2020;368(6497):1290. doi:10.1126/science.abd3377
5. Kendrick K. The coronavirus crisis. 5 medical appointments you
should stop putting off. NPR. March 2, 2021. Accessed July 27, 2022. https://www.npr.org/sections/health-shots/2021/03/02/969215577/5-medical-appointments-you-should-stop-putting-off
6. Lamont EB, Diamond SS, Katriel RG, et al. Trends in oncology clinical trials launched before and during the COVID-19 pandemic. JAMA Netw Open. 2021;4(1):e2036353. doi:10.1001/jamanetworkopen.2020.36353
Quality of Life: The Pending Outcome in Idiopathic Pulmonary Fibrosis
February 6th 2026Because evidence gaps in idiopathic pulmonary fibrosis research hinder demonstration of antifibrotic therapies’ impact on patient quality of life (QOL), integrating validated health-related QOL measures into trials is urgently needed.
Read More
Exploring Racial, Ethnic Disparities in Cancer Care Prior Authorization Decisions
October 24th 2024On this episode of Managed Care Cast, we're talking with the author of a study published in the October 2024 issue of The American Journal of Managed Care® that explored prior authorization decisions in cancer care by race and ethnicity for commercially insured patients.
Listen
Building Trust: Public Priorities for Health Care AI Labeling
January 27th 2026A Michigan-based deliberative study found strong public support for patient-informed artificial intelligence (AI) labeling in health care, emphasizing transparency, privacy, equity, and safety to build trust.
Read More

