- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
The Challenge of Palliative Care for Adolescents and Young Adults
End-of-life care for adolescents and young adults requires an approach that addresses the unique developmental and spiritual issues seen in that population.
During the last 20 years, the field of palliative care (PC) has enjoyed a period of scientific growth. Diseases such as Acquired Immunodeficiency Syndrome, combined with new technologies to combat cardiovascular disease, infection, and cancer, have minimized death from acute events and have led to the majority of adult patients dying from chronic, debilitating illnesses.1 Since approximately 70% of Americans who die each year are elderly, a great majority of palliative care research has been directed toward the care of adults.2 In pediatric oncology, it is recognized that the needs of children are often overlooked despite the acknowledgment that “children are not just small adults.”3 Despite the expertise gained over the last decade for evidence-based delivery of PC to children, there remains a gap in care for adolescents and young adults (AYA). Strategies utilized for children or adults often miss the complex needs (eg, psychosocial changes, emerging sexuality, and existential loss of future) of the AYA.
Adolescents and Young Adults as the “Lost Tribe”
AYA have been described as the “lost tribe” in both oncology and in palliative care.4 This transition period between childhood and adulthood is often defined as 15 to approximately 30 years of age and is marked by tremendous physiologic, developmental, and psychosocial changes.4 Pediatric PC services are often focused on children under 16 years of age, leading to widening of the gap in care experienced by AYA.5 This focus on the delivery of PC to children is particularly evident in the American Academy of Pediatrics position statement from 2000, where palliative care for adolescents is mentioned only in the context of requests for euthanasia.6 The existing PC data for young people between the ages of 15 and 30 years is limited and additional research is therefore necessary to define the specific needs of the AYA population, the goal being to provide optimal service to this population that bridges the transition from childhood to adulthood.
Developmental Stages in AYA Are Vulnerable to Chronic or Life-Threatening Illness
Normal development in the AYA is impacted by life-threatening illness. Widely acknowledged normal adolescent developmental milestones include pubertal development, higher cognitive abilities such as abstract reasoning and risk taking, emerging sense of identity, increasing ability to function independently from parents, and an increasing importance and intimacy in peer relationships. Emerging milestones of adulthood include the establishment of meaningful and enduring relationships; an exploration of identity issues in the worldview, love, and work; a decrease in risky behaviors; and obtaining the appropriate training and education for an occupation.7,8 For the AYA experiencing chronic and life-threatening illness, these milestones are imperiled. Their growing need for privacy and autonomy is met by invasive procedures, hospitalizations, and increased reliance on parents. When self-esteem and positive body image should normally be increasing, the chronically ill AYA is experiencing amputation, hair loss, and weight loss or gain. Most importantly, in the period of time the AYA would normally develop independence, peer relations, and sexual identity, chronic illness limits—or completely prevents—achieving these important milestones. The conflicts of development caused by chronic or life-threatening illness can lead to acting out, high-risk behaviors, and even poor compliance with treatment.
Domains of Palliative Care in Adults Versus AYA
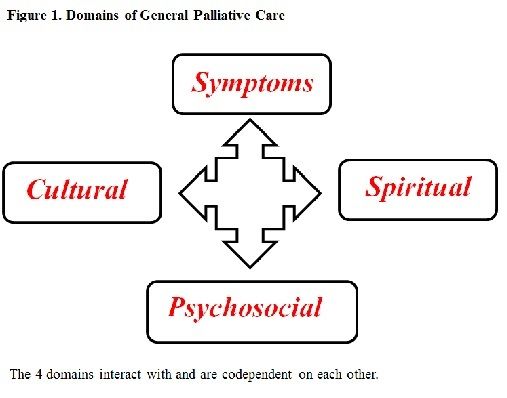
In the last 2 decades, PC for adults has experienced significant growth and 4 specific, interdependent domains of care have been commonly identified (Figure 1).
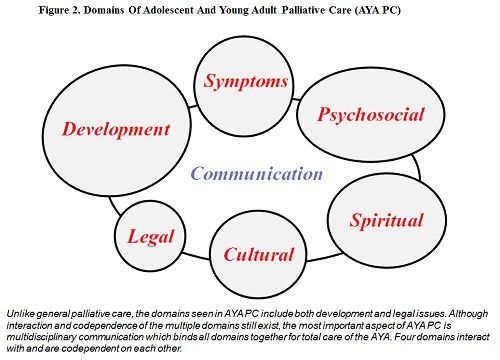
In the AYA, the domains of PC become more complex (Figure 2) with the realms of developmental and legal issues added, and a stronger role of communication between the multidisciplinary healthcare team and the AYA becomes imperative. Even though AYA <18 years of age are considered “minor,” most experts conclude that children >14 years (or even younger if experiencing prolonged chronic illness) have the functional capacity to make medical decisions.9 In particular, the domain of spirituality is enlarged secondary to existential issues (loss of future, loss of sexual or relationship milestones) commonly observed in the AYA population.
Symptom control in the AYA has the most PC data in published literature. In oncology, symptoms experienced by the AYA are quite often linked with the location of the cancer (eg, bone tumor vs leukemia vs brain tumor) with frequency of symptoms in adolescents with cancer being as follows: fatigue (86%), reduced mobility (76%), pain (73%), poor appetite (71%), and shortness of breath (21%), with 50% of patients suffering 3 or more symptoms.10 Although symptoms at the end of life are treated as for any child or adult, the interaction of the physical suffering with the psychological, developmental, spiritual, or cultural influences common to the AYA demographic may uniquely impact and worsen the degree of total suffering experienced by the AYA.11 This concept of AYA-specific stressors leading to worsened symptom control must be an important consideration in all AYAs treated for cancer, especially at the end of life.
The psychology of dying is also influenced by AYA-specific stressors. The dying AYA faces the challenges of not being able to socially mature (overly protective parents, learned passivity), social rejection by peers (which undermines self-esteem), social isolation, and lack of sexual outlets.9 The end result can be high-risk behavior (HRB), regression, poor compliance, anxiety, and depression. HRB includes high-risk sexual experimentation, violence, illicit drug use, and potentially self-harming activities (eg, snowboarding when orthopedically contraindicated). Protective factors (high intelligence, cohesive family, good role models, and religious beliefs) that reduce the chance of HRB often relate to stable social factors and premorbid development of healthy coping skills.12 Lastly, sexual behavior and risk taking is often overlooked by health professionals in the chronically or terminally ill AYA patient—up to 26% of chronically ill patients ages 14 to 18 years, and up to 43% of visibly ill patients (eg, suffering from cerebral palsy or multiple dystrophy) are known to be sexually active.12,13 A majority of AYA who are sexually active report no formal discussion about contraception or safe sex practice. In addition, the sexually transmitted disease (STD) rate has been documented as being higher in the visibly ill AYA patient and is possibly related to the chronically ill being more susceptible to infection.13 The desire for normalcy, intimacy, and acceptance likely puts the chronically or terminally ill AYA at risk for STDs, and therefore communication about sexual practice and increased screening for sexually transmitted infections needs to be included as part of the global assessment for this population, particularly in the early phases of their disease trajectory.
Spirituality in AYA Palliative Care
Spiritual crisis or existential loss is a major theme that AYA face during a life-limiting disease. Spirituality integrates mind, body, and spirit into a sense of wholeness and well- being.14 In the context of AYA palliative care, the extent of the loss of self and future dreams and goals (eg, marriage, career, family, interacting with peers, or loss of limb through amputation) is not known. Although most healthcare professionals believe in the importance of spiritual assessment,14,15 few address spiritual needs beyond religious beliefs and practice.
Sexuality must be considered a component of spirituality in the AYA patient. In the early phases of the illness trajectory, it may be difficult for parents and the healthcare team to consider the AYA as a sexual being, leading to embarrassment (eg, masturbation during hospitalization), guilt (eg, yet undisclosed sexual orientation or gender issues), or even morbidity (eg, unprotected sex with high-risk partners). When acting out or noncompliance is seen in the AYA patient, it might be a sign of existential (spiritual) crisis that warrants further discussion and acknowledgment to ultimately address the overall domain of spirituality in the AYA patient. During later phases of the terminal illness, sexual issues may be overshadowed by physical suffering (eg, pain), but communication should remain open particularly to diffuse negative influences on the AYA patient’s spirituality (eg, guilt, sense of being punished, or imposition of parental beliefs).
Multidisciplinary Model to Deliver AYA Palliative Care
EBO
The dying AYA represents a developmentally unique patient group that requires a fully functional multidisciplinary team to assess and deliver high-quality end-of-life care. Communication between the AYA and the healthcare team may be challenged by barriers inherent to AYA psychology. Ultimately, appropriate education of healthcare staff with an emphasis on communication, compassionate delivery of emotional or psychological symptom relief, and development of skill sets to address spiritual suffering is needed to deliver optimal palliative care to these AYA patients.
Clarke P. Anderson, MD, is assistant clinical professor and staff physician, Department of Pediatrics, City of Hope National Medical Center.
Address for correspondence
Clarke P. Anderson, MD
City of Hope National Medical Center
Department of Pediatrics
1500 E. Duarte RD
MOB 4th Floor
Duarte, CA 91010
E-mail: canderson@coh.org
Funding Source: None
References
- Ferrell BR. Overview of the domains of variables relevant to end-of-life care. J Palliat Med. 2005:8 Suppl 1:S22-S29.
- Institute of Medicine; Field MJ and Behrman RE, eds. When Children Die. Washington, DC: National Academies Press; 2003:690.
- Bleyer WA. Cancer in older adolescents and young adults: epidemiology, diagnosis, treatment, survival, and importance of clinical trials. Med Pediatr Oncol. 2002:38(1):1-10.
- Michelagnoli MP, Pritchard J, Phillips MB. Adolescent oncology—a homeland for the “lost tribe.” Eur J Cancer. 2003:39(18):2571-2572.
- Goldman A, Hewitt M, Collins GS, et al. Symptoms in children/young people with progressive malignant disease: United Kingdom Children's Cancer Study Group/Paediatric Oncology Nurses Forum survey. Pediatrics. 2006:117(6):e1179-e1186.
- American Academy of Pediatrics. Committee on Bioethics and Committee on Hospital Care. Palliative care for children. Pediatrics. 2000:106(2 Pt 1):351-357.
- Holmbeck GN, Devine KA, Bruno EF. (2010). Developmental issues and considerations in research and practice. In Weisz JR and Kazdin AE (eds). Evidence-based psychotherapies for children and adolescents (2nd ed.; pp. 28-39). New York: Guilford.
- Rowland J. Developmental stage and adaptation child and adolescent model. Oxford: Oxford University Press; 1990:519-543.
- Freyer D. Care of the dying adolescent: special considerations. Pediatrics. 2004;113(2):381-388.
- Wein S, Pery S, Zer A. Role of palliative care in adolescent and young adult oncology. J Clin Oncol. 2010;28(32):4819-4824.
- George R, Hutton S. Palliative care in adolescents. Eur J Cancer. 2003;39(18): 2662-2668.
- Valencia LS, Cromer BA. High-risk behavior (HRB) in chronically ill adolescent and young adult patients. J Peds Adol Gyn. 2000;13(2):53-64.
- Suris JC, Resnick MD, Cassuto N, Blum RW. Sexual behavior of adolescents with chronic disease and disability. J Adolesc Health. 1996;19(2):124-131.
- Davies B, Brenner P, Orloff S, Sumner L, Worden W. Addressing spirituality in pediatric hospice and palliative care. J Palliat Care. 2002;18(1):59-67.
- Lambrecht T, Anderson C. Multidisciplinary attitudes toward cultural and spiritual beliefs in pediatric palliative care. Proceedings of the European Association of Palliative Care. 2003; Den Hague.
Subjective and Objective Impacts of Ambulatory AI Scribes
January 8th 2026Although the vast majority of physicians using an artificial intelligence (AI) scribe perceived a reduction in documentation time, those with the most actual time savings had higher relative baseline levels of documentation time.
Read More
Exploring Racial, Ethnic Disparities in Cancer Care Prior Authorization Decisions
October 24th 2024On this episode of Managed Care Cast, we're talking with the author of a study published in the October 2024 issue of The American Journal of Managed Care® that explored prior authorization decisions in cancer care by race and ethnicity for commercially insured patients.
Listen

