- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Bridging the Care Gap Between Pediatric and Young Adult Cancer
Through a multi-site, multidisciplinary approach, AYA@USC addresses the unique needs of young adult cancer patients, improving outcomes and bridging the care gap in this population.
Background
About 70,000 adolescent and young adult (AYA) cancer patients, aged 15 to 39 years, are newly diagnosed annually in the United States; this includes an estimated 4000 or more in the Los Angeles Basin alone. Despite tremendous advancements achieved in pediatric and older adult cancers, the relative improvement in the survival rates and outcomes for AYA patients has not kept pace. For instance, from 1975 to 1997, the average annual improvement in 5-year survival rates for invasive cancers was 1.5% for all ages; however, improvement averaged only 0.5% for cancers in the entire AYA population, and survival actually decreased by -0.18% for individuals aged 30 to 34 years.1
During the past 10 years, the so-called “AYA gap” has become the subject of national focus and attention. It has been well documented that AYA patients with cancer often fall through gaps in their clinical and supportive care.2-5 An understanding of the unique characteristics and outcomes of this group is a continued need. The shared norms, attitudes, and beliefs that determine their behavior as well as the stressors encountered on a daily basis (such as identity formation, body image concerns, sexual relationships, independence from parents, autonomous decision making, as well as educational, career, and personal growth goals) impact the ability of an AYA to cope with cancer.3
Problems that care providers face, including a lack of multidisciplinary teams, limited availability of therapeutic clinical trials focused on the AYA population, and even a lower rate of drug and device approvals for the less common cancer types seen in AYA patients can all lead to more suboptimal treatment planning. Consequently, AYA patients have been treated based on guidelines and recommendations developed exclusively for pediatric or adult oncology patients with cancer, without any regard for differences in host tolerance to treatments, tumor biology, and psychosocial developmental stage.6-9 The unaddressed needs of this population can result in increased likelihood of misdiagnosis, late stage diagnosis, and reduced adherence to treatment and follow-up.4,6,10
In an effort to mitigate these gaps in care and to develop a national agenda for AYA oncology, the National Cancer Institute, in collaboration with the LIVESTRONG Young Adult Alliance, established the Adolescent and Young Adult Oncology Progress Review Group (PRG). The PRG outlined 5 imperatives for improving the outcomes of AYA patients with cancer, one of which includes a recommendation to ensure excellence in service delivery across the cancer control continuum.11 Further, the National Comprehensive Cancer Network (NCCN) AYA Guidelines Panel strongly advises that AYA patients be referred to cancer centers with expertise and experience in treating patients in this age group and the cancers that affect them. There is a definite need for comprehensive models of cancer care that have this population’s diverse needs in mind.1,11-16
Through the systematic and proactive provision of age-appropriate support services and a multidisciplinary approach to clinical care, the Adolescent and Young Adult Cancer Program at the University of Southern California (AYA@USC) has developed a care model to bridge the gaps experienced by this population.
Model and Intervention
From its inception, the care model has been sponsored by the USC Norris Comprehensive Cancer Center and structured with joint pediatric and medical oncology leadership spanning 2 major USC-affiliated academic medical centers: the Norris Cancer Hospital at the Keck Medical Center (USC) and Children’s Hospital Los Angeles (CHLA). Both are private nonprofit medical institutions.
The AYA@USC clinical team works collaboratively with existing disease-specific oncology teams to bring the AYA perspective to patient care, focusing on the unique needs of this population such as fertility and psychosocial concerns. The team, comprised of 2 medical directors (pediatric oncologist and adult oncologist), a program manager, 3 part-time nurse navigators (NNs), and a social worker (SW), have streamlined resource utilization through the development of efficient algorithms within the USC and CHLA community networks. This algorithmic model of care ensures that protocol-defined patients are appropriately assessed by both nursing and social work disciplines as they assist patients with gaining access to needed services, referrals, follow-up care, and provide education uniquely tailored to AYAs. Each disease-specific oncology team identifies an AYA “champion” and provides feedback to AYA@USC.
During the nascent stages of program development, stakeholders across the healthcare spectrum were engaged in a collaborative forum in which principles were developed to ensure the successful implementation of the program. These principles include:
1. A resource or space-efficient decentralized care model in which disease-based treating oncologists continue to manage patient care.
2. AYA clinical team provides supportive care planning and recommendations.
3. AYA physician champions serve in each specialty area to align their group’s AYA practice and processes.
4. Fluid and collaborative communication between the AYA clinical team and treating oncology teams.
Figure 1
5. Multidisciplinary and collaborative approach to program development with input from all partnering stakeholders ().
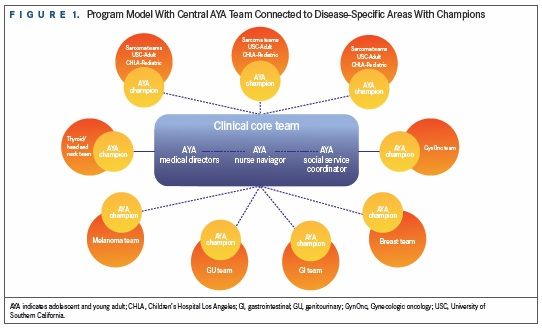
Figure 2
Based on these guiding principles, program enrollment began in November 2013 and several hundred AYA patients have since been referred to the program. An overview of the clinical care and services provided to patients can be found below and in .
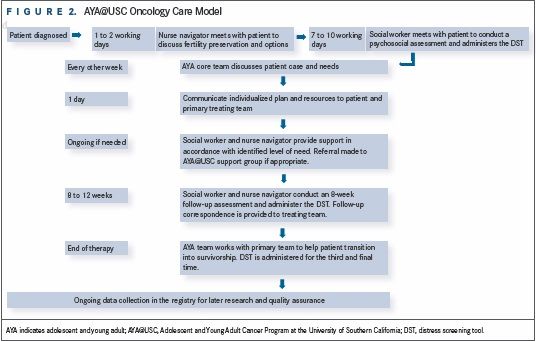
1. Oncology patients (15 to 39 years old) are either referred by healthcare professionals or identified from an electronic medical record. The NN and/or SW seek permission from the treating oncology team prior to providing AYA services.
Figure 3
2. The NN aims to contact the patient within 1 to 2 working days to provide fertility preservation education consistent with guidelines by the American Society of Clinical Oncology and acts as a conduit to perform a preliminary evaluation with referrals.17 See for the fertility education algorithm.
3. The SW conducts an in-depth psychosocial assessment within 10 days, including the Distress Screening Tool and Thermometer (DT), adjusted for the AYA population. If a patient scores >7 on DT, immediate SW intervention occurs.18,19
4. Information gathered from the initial NN and SW assessments are presented at a bimonthly AYA team case conference; identified needs are addressed, and resources and referrals are made. Recommendations are communicated to the treating oncology team and the patient.
5. Referral to AYA@USC or regional support group is made if appropriate.
6. About 8 to 12 weeks later, an additional assessment is conducted to follow up on previously identified concerns and assessments for new issues. The DT is administered again and addressed accordingly.
7. The NN and SW contact the patient once active treatment has been completed to provide resources, education, and support while transitioning into survivorship. The DT is administered and addressed for the third time.
8. Biweekly AYA team meetings are held to discuss key findings of referred patients, challenging cases, controversies, and new evidence-based literature and developments.
Case Example 1
Patient is a 32-year-old female, diagnosed with a gastrointestinal stromal tumor; status is post complete resection. Patient rated her initial distress at 8 on a scale of 1 through 10, and her top concerns were fertility, living arrangements, finances, family dynamics, relationship status, isolation, anxiety, insomnia, and diarrhea. At initial encounter, the treatment plan was still being formulated, and it was unknown if fertility-harming therapy would be prescribed. NN provided fertility preservation education and addressed her fertility concerns. Because the patient strongly desired future biological children, she came to the decision to pursue fertility preservation prior to the start of additional therapy in order to safeguard the possibility of having a biological offspring. Referral to a reproductive endocrinologist was arranged, and the patient successfully cryopreserved oocytes prior to the start of adjuvant therapy with imatinib (Gleevec). SW addressed the practical, familial, and emotional concerns by connecting the patient with AYA resources and providing 8 individualized, brief therapy sessions to address relationship stressors. NN addressed the insomnia and diarrhea concerns by suggesting a variety of nursing interventions.
At the 8-week follow-up, the patient’s distress fell to a 3 with self-reported decreased anxiety and increased family engagement. Patient utilized various resources in the community including meditation or yoga and connected with another survivor through Imerman Angels, a national nonprofit that provides peer support to cancer patients. The patient is still in active treatment, and AYA@USC will help bridge the transition into survivorship when treatment is completed.
Case Example 2
Patient is a 31-year-old male, diagnosed with sarcoma that presented with a 2-month history of increasing abdominal girth, pelvic pain, and malaise. CT scan revealed a retroperitoneal mass with metastasis to lymph nodes and lungs. Patient received 6 cycles of standard of care chemotherapy followed by surgical resection.
Patient expressed interest in having future biological children and was counseled on fertility preservation by the NN who then made arrangements for sperm banking while the patient was hospitalized. However, the patient was unsuccessful at obtaining a sperm sample due to the impact of disease on ejaculatory function.
The patient rated his initial distress at 8, citing career, finances, emotional distress, exercise ability, sexual concerns, and nutrition as top issues. He was provided with financial assistance applications, career resources, AYA-specific support resources, and individualized social work support. Through education and provision of resources, the NN addressed concerns with erectile dysfunction and decreased libido; the patient declined urological consult. AYA@USC was able to assist with referrals to occupational and physical therapies to address his exercise concerns. Referral to a nutritionist was completed.
Eight weeks later, the patient rated his distress at 5. While the patient’s financial concerns remained, he had not pursued any of the financial resources previously provided. Patient verbalized new concerns surrounding his social life and, per AYA recommendation, began participating in the AYA@USC patient support group. Emotional concerns persisted and individualized social work support was utilized again. Occupational and physical therapy were continued to address the patient’s persistent concern with his ability to exercise.
The patient is currently pursuing surgical intervention for additional treatment. AYA@USC will continue to follow him and eventually will bridge the transition into survivorship.
Discussion
AYAs with cancer have not benefited comparably from the increased survival and reduced mortality experienced by both older and younger cancer patients.1 Tremendous gaps concerning how best to treat AYA patients with cancer exist while supportive care services, when available, can often be fractured and uncoordinated. In general, without a coordinated AYA program, patients who already experience lower levels of insurance coverage and health care access further experience referral issues, problems with copay and negotiation of covered services, and lack of specialized services such as fertility preservation.20-23 Additionally, in the academic medical system setting, available clinical trials are typically targeted to either the pediatric or adult end of the age spectrum—AYA@USC was conceived in response to these gaps.
Downstream benefits of the AYA program include the impact on health limitations experienced by survivors. Kirchhoff et al highlight how AYA survivors are not receiving primary medical care services and report cost barriers to care at levels beyond these general age differences. Hidden costs related to prolonged economic loss of productivity, transportation issues for patients getting to treatment and follow-up appointments, and fluctuations in caregiver or childcare services can compound and present barriers associated with healthcare for AYAs.20,22,24,25 The AYA@USC clinical team serves as a bridge to AYA survivorship services when treatment is completed. In the LIFE Cancer Survivorship & Transition Program at USC, detection and management of late effects, assessment of psychosocial functioning, health-related education, and financial and employment challenges are all addressed to improve outcomes for AYA survivors.26
Conclusion
The AYA@USC program was developed to ensure excellence in care across the cancer control continuum for AYAs. Programmatic development was guided by recommendations outlined in the PRG report to adopt AYA patient-centered approaches to care, in collaboration with the NCCN clinical practice guidelines in AYA oncology.11,16 Sustaining these standards of cancer care for AYAs has required the ongoing communication and commitment of a diverse array of stakeholders.
EBO
Future plans for the program include the analysis of clinical data (distress levels, fertility consults, and pain scores), financial data (length of stay, inpatient readmission rates, and health-related quality of life), and patient and staff satisfaction surveys to inform future interventions and best practices. The AYA@USC model was designed to be exportable to other facilities including Los Angeles County Hospital+USC—the largest single provider of healthcare in the county—to build a regional network for AYA patient care. The hope is models such as these will contribute to the impending national standard of care for AYAs with cancer.
Laurel Barosh, MPH, is founding program manager, Adolescent and Young Adult Oncology Program, USC Norris Comprehensive Cancer Center
Terry Church, MA, MS, is interim program manager, Adolescent and Young Adult Oncology Program, USC Norris Comprehensive Cancer Center
Deborah Morgan, MSN, RN, OCN, is lead nurse navigator, Adolescent and Young Adult Oncology Program, USC Norris Comprehensive Cancer Center
Megan Bianchetti, MSW, is lead social worker, Adolescent and Young Adult Oncology Program, USC Norris Comprehensive Cancer Center
James Hu, MD, FACP, is co-medical director, Adolescent and Young Adult Oncology Program, USC Norris Comprehensive Cancer Center
Debu Tripathy, MD, is founding co-medical director, Adolescent and Young Adult Oncology Program, USC Norris Comprehensive Cancer Center; chair, Breast Medical Oncology, University of Texas MD Anderson Cancer Center
Stuart E. Siegel, MD, is co-medical director, Adolescent and Young Adult Oncology Program, USC Norris Comprehensive Cancer Center; founding director, Children's Center for Cancer and Blood Diseases and the Center for International Health at Children’s Hospital Los Angeles.
Acknowledgments
The authors would like to thank Stephanie Morley for her diligent work as program assistant and database manager, as well as Julia Sturgeon and Sharon Jiang for their assistance in data analysis.
Corresponding Author
Stuart E. Siegel, MD
USC Norris Comprehensive Cancer Center
1441 Eastlake Ave, Los Angeles, CA
E-mail: ssiegel@chla.usc.edu
Funding Sources
UniHealth Foundation, Concern Foundation, and USC Norris Auxiliary Board.
References
- Bleyer A, O'Leary M, Ries LAG (eds). Cancer Epidemiology in Older Adolescents and Young Adults 15 to 29 Years of Age, Including SEER Incidence and Survival: 1975-2000. 2006; National Cancer Institute, NIH: Bethesda, MD.
- Parsons HM, Harlan LC, Lynch CF, et al. Impact of cancer on work and education among adolescent and young adult cancer survivors. J Clin Oncol. 2012;30(19):2393-2400.
- Zebrack B and Isaacson S. Psychosocial care of adolescent and young adult patients with cancer and survivors. J Clin Oncol. 2012;30(11):1221-1226.
- Keegan TH, Lichtensztajn DY, Kato I, et al. Unmet adolescent and young adult cancer survivors information and service needs: a population-based cancer registry study. J Cancer Surviv. 2012;6(3):239-250.
- Bleyer A and Barr R. Cancer in young adults 20 to 39 years of age: overview. Semin Oncol. 2009;36(3):194-206.
- Bleyer A. The adolescent and young adult gap in cancer care and outcome. Curr Probl Pediatr Adolesc Health Care. 2005;35(5):182-217.
- Bleyer A. Young adult oncology: the patients and their survival challenges. CA Cancer J Clin. 2007;57(4):242-255.
- Tai E, Pollack LA, Townsend J, et al. Differences in non-Hodgkin lymphoma survival between young adults and children. Arch Pediatr Adolesc Med. 2010;164(3):218-224.
- Thomas DM, Seymour JF, O'Brien T, Sawyer SM, Ashley DM. Adolescent and young adult cancer: a revolution in evolution? Intern Med J. 2006;36(5):302-307.
- Zebrack BJ, Block R, Hayes-Lattin B, et al. Psychosocial service use and unmet need among recently diagnosed adolescent and young adult cancer patients. Cancer. 2013;119(1):201-214.
- Adolescent and Young Adult Oncology Progress Review Group. Closing the gap: research and care imperatives for adolescents and young adults with cancer. L.A.F. National Cancer Institute, Editor. 2006, US Department of Health and Human Services.
- Evan EE and Zeltzer LK. Psychosocial dimensions of cancer in adolescents and young adults. Cancer. 2006;107(7 Suppl):1663-1671.
- Zebrack B, Hamilton R, Smith AW. Psychosocial outcomes and service use among young adults with cancer. Semin Oncol. 2009;36(5):468-477.
- Tricoli JV, Seibel NL, Blair DG, Albritton K, Hayes-Lattin B. Unique characteristics of adolescent and young adult acute lymphoblastic leukemia, breast cancer, and colon cancer. J Natl Cancer Inst. 2011;103(8):628-635.
- Zebrack B, Mathews-Bradshaw B, Siegel S; LIVESTRONG Young Adult Alliance. Quality cancer care for adolescents and young adults: a position statement. J Clin Oncol. 2010;28(32):4862-4867.
- Coccia PF, Altman J, Bhatia S, et al. Adolescent and Young Adult Oncology: Clinical Practiec Guidelines in Oncology. J Natl Compr Canc Netw. 2012;10(9):1112-1150.
- Loren AW, Mangu PB, Beck LN, et al. Fertility preservation for patients with cancer: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol. 2013;31(19):2500-2510.
- Bleyer A. How NCCN guidelines can help young adults and older adolescents with cancer and the professionals who care for them. J Natl Compr Canc Netw. 2012;10(9):1065-1071.
- National Comprehensive Cancer Network. Distress management. Clinical practice guidelines. J Natl Compr Canc Netw. 2003;1(3):344-374.
- Daniel LC, Barakat LP, Brumley LD, Schwartz LA. Health-related hindrance of personal goals of adolescents with cancer: the role of the interaction of race/ethnicity and income. J Clin Psychol Med Settings. 2014;21(2):155-164.
- Guy GP, Yabroff KR, Ekwueme DU, et al. Estimating the health and economic burden of cancer among those diagnosed as adolescents and young adults. Health Aff. 2014;33(6):1024-1031.
- Kirchhoff AC, Lyles CR, Fluchel M, Wright J, Leisenring W. Limitations in health care access and utilization among long-term survivors of adolescent and young adult cancer. Cancer. 2012;118(23):5964-5972.
- Parsons HM, Schmidt S, Harlan LC, et al. Young and uninsured: insurance patterns of recently diagnosed adolescent and young adult cancer survivors in the AYA HOPE study. Cancer. 2014;120(15):2352-2360.
- Kinahan KE, Sanford S, Sadak KT, et al. Models of cancer survivorship care for adolescents and young adults. Semin Oncol Nurs. 2015;31(3):251-259.
- Nass SJ, Beaupin LK, Demark-Wahnefried W et al. Identifying and addressing the needs of adolescents and young adults with cancer: summary of an Institute of Medicine workshop. Oncologist. 2015;20(2):186-195.
- Freyer DR. Transition of care for young adult survivors of childhood and adolescent cancer: rationale and approaches. J Clin Oncol. 2010;28(32):4810-4818.