- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
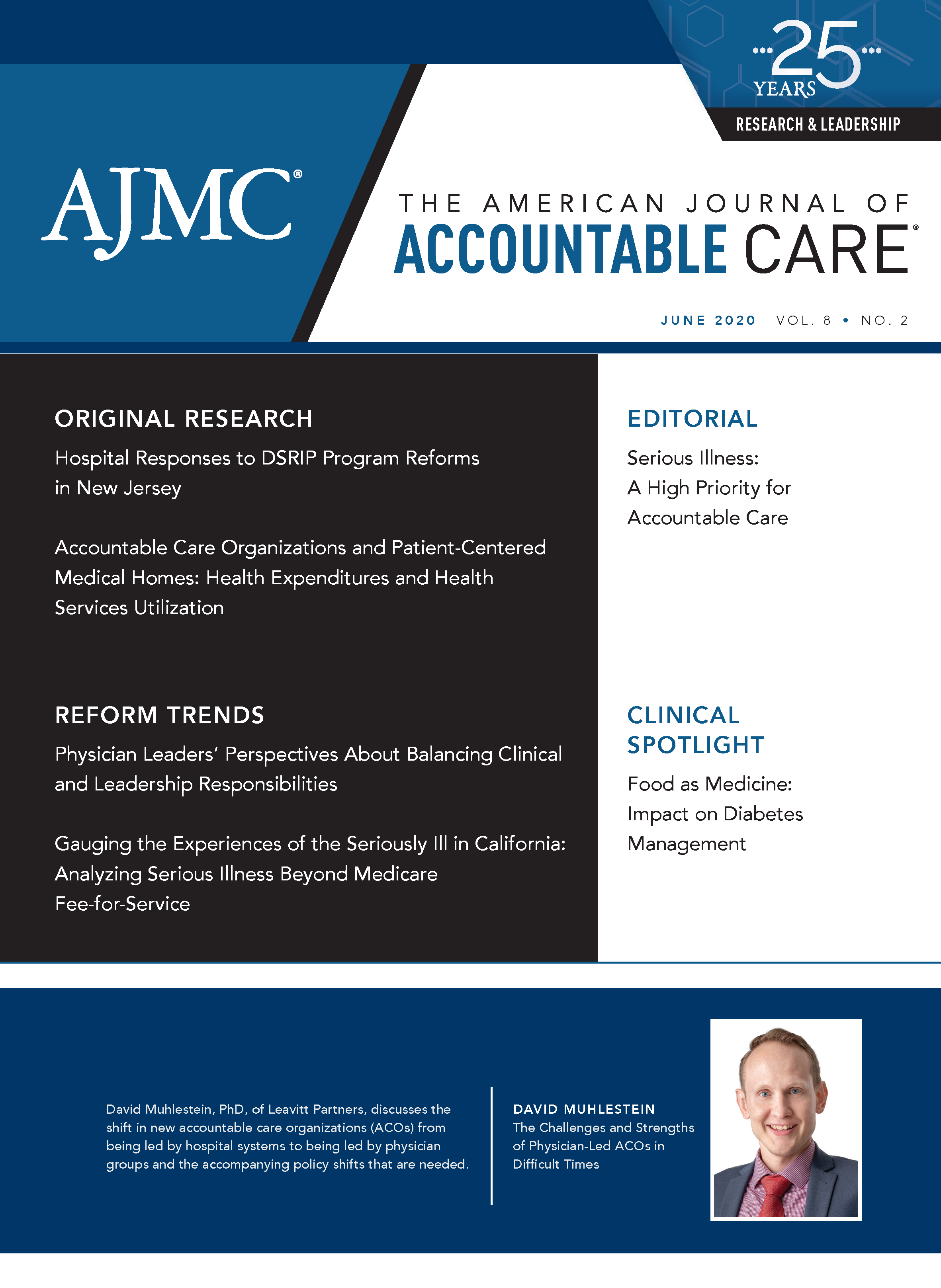
Serious Illness: A High Priority for Accountable Care
Accountable health care organizations are increasingly recognizing that the care of individuals with serious illness represents a prime opportunity for improvement.
The American Journal of Accountable Care. 2020;8(2):32-33. https://doi.org/10.37765/ajac.2020.88441
At least 12 million adults and half a million children in the United States are living with a serious illness.1,2 A serious illness is a health condition that carries a high risk of mortality and commonly affects a patient for several years, such as metastatic cancer, heart failure, chronic obstructive pulmonary disease, and dementia.3 As the authors of “Gauging the Experiences of the Seriously Ill in California: Analyzing Serious Illness Beyond Medicare Fee-for Service” have highlighted in the current issue,4 individuals living with a serious illness are the disproportionate users of our health care system: 911 calls, emergency department visits, repeated hospitalizations, and polypharmacy occur 4 to 5 times more frequently in this population. Yet despite high utilization and spending, those with serious illnesses often receive low-value—even distressing—service from our health care system.5,6 In particular:
- Symptoms are often inadequately addressed. For example, 64% of people with metastatic cancer report high levels of pain, despite being under the active care of an oncology team.7
- Communication and shared decision making are insufficient. For example, fewer than 50% of hospitalized patients with a serious illness were ever asked what their personal preferences would be if a critical situation should arise,8 and only 47% of discharged patients report fully understanding their discharge instructions.9
- The outsized responsibilities placed on family caregivers are taking an enormous toll. More than 1 in 5 cite adverse impacts on their own health,10 and formal studies conclude that caregivers face a 63% increased risk of mortality.11
Fortunately, accountable health care organizations are increasingly recognizing that the care of individuals with a serious illness represents a prime opportunity for improvement. Value-driven providers, accountable care organizations, Medicare Advantage plans, and others are implementing effective strategies that improve quality of life while decreasing costs.
These strategies entail first identifying the population living with serious illnesses early enough to impact the course of their trajectory; the article in this issue provides important insight into a useful identification process. Once the population is identified, clinicians with appropriate training should work to clarify patients’ goals of care and assess both symptom and caregiver burden. Nurse care managers are often best situated to these conversations and can then work with the treating teams to modify care plans accordingly. For those with high levels of need, specialty palliative care teams should consult or comanage the care, including providing home-based care when appropriate.
Together, building early identification processes, training key clinicians in communication and symptom management skills, and ensuring access to specialty palliative care when warranted make a dramatic difference in both the quality and the cost of care for individuals living with a serious illness.12
Author Affiliation: Center to Advance Palliative Care, New York, NY.
Source of Funding: None.
Author Disclosures: Ms Silvers has received a grant to educate on serious illness care.
Authorship Information: Concept and design; drafting of the manuscript; and literature/citation review.
Send Correspondence to: Allison Silvers, MBA, Vice President, Payment and Policy, Center to Advance Palliative Care, 55 W 125th St, Ste 1302, New York, NY 10027. Email: allison.silvers@mssm.edu.
REFERENCES
1. Hayes SL, Salzberg CA, McCarthy D, et al. High-need, high-cost patients: who are they and how do they use health care? a population-based comparison of demographics, health care use, and expenditures. Issue Brief (Commonw Fund). 2016;26:1-14.
2. Institute of Medicine. When Children Die: Improving Palliative and End-of-Life Care for Children and Their Families. The National Academies Press; 2003.
3. Institute of Medicine. Dying in America: Improving Quality and Honoring Individual Preferences Near the End of Life. The National Academies Press; 2015.
4. Anderson D, Yanagihara D, Japinga M, Saunders R. Gauging the experiences of the seriously ill in California: analyzing serious illness beyond Medicare fee-for-service. Am J Accountable Care. 2020;8(2):22-25.
5. Teno JM, Clarridge BR, Casey V, et al. Family perspectives on end-of-life care at the last place of care. JAMA. 2004;291(1):88-93. doi:10.1001/jama.291.1.88
6. Meier DE. Increased access to palliative care and hospice services: opportunities to improve value in health care. Milbank Q. 2011;89(3):343-380. doi:10.1111/j.1468-0009.2011.00632.x
7. van den Beuken-van Everdingen MH, Hochstenbach LM, Joosten EA, et al. Update on prevalence of pain in patients with cancer: systematic review and meta-analysis. J Pain Symptom Manage. 2016;51(6):1070-1090.e9. doi:10.1016/j.jpainsymman.2015.12.340
8. Being seriously ill in America today. Harvard T.H. Chan School of Public Health. October 2018. Accessed October 30, 2018. https://cdn1.sph.harvard.edu/wp-content/uploads/sites/94/2018/10/CMWF-NYT-HSPH-Seriously-Ill-Poll-Report.pdf
9. Summary of HCAHPS survey results. Hospital Consumer Assessment of Healthcare Providers and Systems. October 31, 2018. Accessed November 30, 2018. https://hcahpsonline.org/globalassets/hcahps/summary-analyses/summary-results/2018_10_summary-_analysis_states_results.pdf
10. Caregiving in the U.S. National Alliance for Caregiving. June 2015. Accessed November 30, 2018. https://www.caregiving.org/wp-content/uploads/2015/05/2015_CaregivingintheUS_Final-Report-June-4_WEB.pdf
11. Schulz R, Beach SR. Caregiving as a risk factor for mortality: the Caregiver Health Effects Study. JAMA. 1999;282(23):2215-2219. doi:10.1001/jama.282.23.2215
12. Lustbader D, Mudra M, Romano C, et al. The impact of a home-based palliative care program in an accountable care organization. J Palliat Med. 2017;20(1):23-28. doi:10.1089/jpm.2016.0265
Quality of Life: The Pending Outcome in Idiopathic Pulmonary Fibrosis
February 6th 2026Because evidence gaps in idiopathic pulmonary fibrosis research hinder demonstration of antifibrotic therapies’ impact on patient quality of life (QOL), integrating validated health-related QOL measures into trials is urgently needed.
Read More
Building Trust: Public Priorities for Health Care AI Labeling
January 27th 2026A Michigan-based deliberative study found strong public support for patient-informed artificial intelligence (AI) labeling in health care, emphasizing transparency, privacy, equity, and safety to build trust.
Read More
Ambient AI Tool Adoption in US Hospitals and Associated Factors
January 27th 2026Nearly two-thirds of hospitals using Epic have adopted ambient artificial intelligence (AI), with higher uptake among larger, not-for-profit hospitals and those with higher workload and stronger financial performance.
Read More
Motivating and Enabling Factors Supporting Targeted Improvements to Hospital-SNF Transitions
January 26th 2026Skilled nursing facilities (SNFs) with a high volume of referred patients with Alzheimer disease and related dementias may work harder to manage care transitions with less availability of resources that enable high-quality handoffs.
Read More

