- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
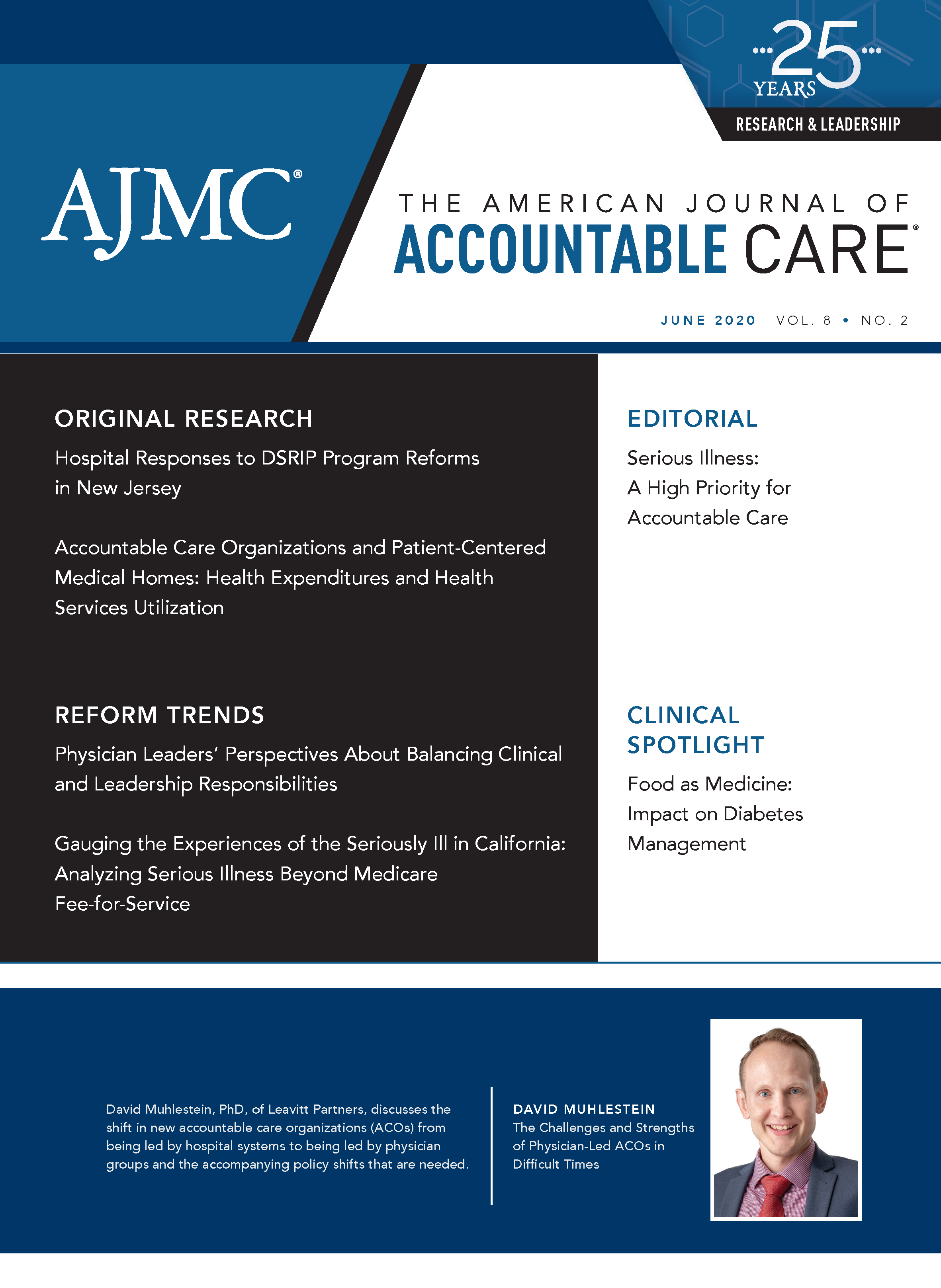
Food as Medicine: Impact on Diabetes Management
This article addresses what employers need to know about food as medicine and offers practical steps to reduce barriers for their employee populations.
ABSTRACT
When we think of medicine to treat diabetes, we typically think of pills and insulin injections to improve glycemic control. Evolving science is now pointing to a new medicine for diabetes and other chronic conditions: food. Although it is encouraging to offer alternatives to medications to individuals who face chronic conditions such as type 2 diabetes, many Americans are negatively affected by social determinants of health and do not have access to healthy foods. Existing concerns about comorbidities are heightened during the coronavirus disease 2019 pandemic, as those with diabetes who are diagnosed with the virus face particularly poor prognoses. This article addresses what employers need to know about food as medicine and offers practical steps to reduce barriers for their employee populations.
The American Journal of Accountable Care. 2020;8(2):34-37. https://doi.org/10.37765/ajac.2020.88442
When we think of medicine to treat diabetes, we typically think of pills and insulin injections to improve glycemic control. Evolving science is now pointing to a new medicine for diabetes and other chronic conditions: food. Paying attention to calories, fat, and carbohydrates is important to a person with diabetes, but food as medicine goes further. Affordable, nutritious food that is anti-inflammatory, is aligned with an individual’s genetic makeup and microbiome, and complements rather than conflicts with medication not only affects a person’s future health but also affects ongoing diabetes treatment and outcomes.
In helping individuals prevent and manage diabetes, we need to consider food as medicine in addition to the more standard treatment modalities. Unfortunately, 49 million people in United States lack access to affordable, nutritious food, which is a major cause for concern given the impact of food on both the prevention and management of diabetes.1 It is difficult to use food as medicine when barriers exist to nutritious food. These barriers are part of what we call the social determinants of health (SDOH), which, as defined by the World Health Organization, include the conditions in which people are born, grow, live, work, and age.2 These factors can affect our health and health care outside of the traditional treatment environment.
Food insecurity is defined as when a person cannot meet their dietary needs on a consistent basis regardless of socioeconomic status or employment status.3 This factor and other SDOH are not just an issue for those of low socioeconomic status. In fact, approximately 50% of those with food insecurity are employed. Individuals experiencing food insecurity often consume a nutrient-poor diet, which may contribute to the development of obesity, heart disease, hypertension, diabetes, and other chronic diseases.4 People who live in food-insecure households also have difficulties in managing diet-related chronic conditions.5
Food insecurity can be due to a variety of factors including reliable and affordable transportation, mobility issues, inconvenient access to healthy foods, financial struggles, lack of time, and inadequate cooking expertise. These needs are fluid and may change over time. Studies about food insecurity have shown that more than 80% of those who cannot routinely meet their dietary needs will need varying levels of nutrition support over a 12-month time frame.1 People with type 2 diabetes may find themselves limited to purchasing inexpensive, high-calorie, nutritionally poor foods, including foods high in refined carbohydrates, instead of items that are more healthful, such as vegetables, lean proteins, and whole grains.6 During the coronavirus disease 2019 (COVID-19) pandemic, millions face temporary or permanent job loss and more have sought food assistance, exacerbating the documented 2-way connection between diabetes and COVID-19, which can contribute to the worsening of glucose control.7
So, how can employers realistically have an impact on SDOH, including food insecurity? There are small steps employers can take, as well as many public and community resources available to positively affect the workforce.
Take for example, a midsize manufacturer located in the Midwest with a diverse, predominantly male employee population in which a large percentage ranges from having prediabetes to having uncontrolled diabetes. This employer realized that despite offering healthy food options in the onsite cafeteria, employees routinely left campus to buy food across the street at a local ethnic grocery store. Instead of fighting the competition, the employer partnered with the local grocer to offer greater accessibility to affordable nutritious foods by launching its own healthy meal preparation program.
This service provides a once-a-week healthy meal that serves a family of 4 for under $20. Employees can choose from 3 healthy meal options—they receive the meal fixings and recipes, all packaged and ready to take home at the end of the workday. The employer works with an onsite wellness provider to develop weekly menus/recipes, and the onsite cafeteria features a healthy meal each week. In this example, participation in the program grew through word of mouth, a comprehensive communications campaign, and weekly raffle prizes for participants.
Moving the needle on SDOH requires instituting policies and programs that have “evidence of effectiveness” to improve health factors that lead to improved outcomes. But what does “evidence of effectiveness” really mean? Employers can use County Health Rankings & Roadmaps8 as a resource to understand the challenges faced in their communities and to launch initiatives that are scientifically proven to be effective, which is important, given the limited time and resources that employers have available to devote to workplace health (Figure9).
These rankings are based on a model of population health that considers many factors that, if improved, can help make communities healthier places to live, learn, work, and play. Strategies are generally assessed in terms of their effect on health factors, those things we can modify to improve length and quality of life, rather than on health directly. For example, employers may not be able to directly impact diabetes, but they can provide their employees with ample time for lunch and snack breaks and affordable healthy foods; these efforts may lead to better nutrition and an improvement in health factors that include glycated hemoglobin (A1C) values, stress, and body weight, which will ultimately help employees manage diabetes more effectively.
In the County Health Rankings,8 strategies are assigned an evidence rating based on the quantity, quality, and findings of relevant research. The most effective strategies get a rating of “scientifically supported” and those with insufficient results receive an “evidence of ineffectiveness” rating (Table10). Employers who seek the most “bang for their buck” can use these ratings to prioritize workplace initiatives.
For example, a multicomponent obesity intervention led by a trained professional and competitive pricing of healthy foods in the employee cafeteria are most likely to make a difference—both are “scientifically supported.” Other worksite strategies have “some evidence” and are likely to work but need further research, including providing fruit and vegetable taste testing, displaying point-of-purchase prompts for healthy foods, including nutrition labels on cafeteria foods, offering fresh fruits and vegetables at a workplace farmers’ market, providing incentives for adopting healthy behaviors, and taxing sugar-sweetened beverages and unhealthy snacks.
Other interventions that are recommended by credible experts but have limited research documenting their impact include community weight loss challenges and offering healthy foods at catered events—these are given an “expert opinion” rating. On the far end of the spectrum, offering nutrition education and/or cooking classes through a community kitchen and providing access to an online grocery store to purchase healthy foods are given an “insufficient evidence” rating. Unless an organization has unlimited funds for nutrition interventions, programs on this end of the scale will likely not have a significant impact on health factors, including reversing the course of prediabetes and helping those with diabetes manage their condition.
Recently, new initiatives have been launched to meet people where they live and shop, such as St Joseph Hoag Health’s “Shop with Your Doc” program in California.11 This program stations doctors, nurses, and registered dietitians in local grocery stores to provide right-on-time advice and consultation on a variety of health topics, including how to read a label and what it means to have prediabetes.
We have known for a long time that food can affect blood sugar, which is why employers often provide health plan coverage for diabetes educators and/or diabetes-focused nutritionists. This modality of nutrition support has been based on population health models but is not personalized at the individual level. What is evolving is the nutritional science, which shows that food can affect high blood sugar and A1C in ways that were not known in the past.
The unique nutritional needs of a person with diabetes depend on several factors. Blood sugar control through precision-based nutrition based on an individual’s microbiome has shown great promise. Microbiomes in humans can be found in the gastrointestinal tract, skin, nose, and other areas of the body. The microbiomes in our gastrointestinal tract influence how our bodies respond to stress, how we digest food, and the health of our immune systems. Positive results have been realized by creating a nutritional plan that will create and support healthy bacteria in the gut, allowing it to break down foods in a manner that reduces and controls blood sugar spikes. This has been shown to allow people with diabetes to reduce their medication load, and it can potentially put prediabetes into remission as well.
Even hospitals that have historically relied on traditional medications to treat chronic health conditions like diabetes have gotten into a “food as medicine” frame of mind. For example, Zuckerberg San Francisco General Hospital recently launched the Therapeutic Food Pantry. Through this clinically based prescription food program, providers prescribe fresh fruits and vegetables as well as other foods aligned to an individual’s specific therapeutic and microbiome needs.12 Upon arrival at the pantry, patients receive nutrition education, food demonstrations, and referrals to other local resources, and then walk away with approximately 25 pounds of food that aligns with their disease state and health goals.12
By seeking opportunities such as this, employers can establish partnerships with local health care organizations and other community agencies to make nutritious, affordable foods a convenient reality for all employees, regardless of their socioeconomic status. Many innovative employers have established such collaboratives that are a win for the employee, the employer, and the community. An example is Kraft Foods, which has partnered with the Chicago Botanic Garden to plant and cultivate vegetable and herb gardens on company grounds. The impact of this initiative is multifaceted, including teaching employees how to plant fruits and vegetables, educating employees on healthy eating, making the harvest available within the company cafeteria, and supporting local food banks with locally grown food.
At the end of the day, it is up to an individual to decide what to eat, when to eat, and how much to eat. Employers can and should support healthy nutrition both within the corporate space and within the community. Only when the full ecosystem is on board will “food as medicine” help reverse the growing trend of diabetes, which not only costs employers significantly but also diminishes quality of life for the more than 34.2 million Americans with this chronic condition.13
Author Affiliations: Midwest Business Group on Health (JEB, DG, DW), Chicago, IL.
Source of Funding: None.
Author Disclosures: The authors report no relationship or financial interest with any entity that would pose a conflict of interest with the subject matter of this article.
Authorship Information: Concept and design (JEB, DG, DW); drafting of the manuscript (JEB, DG, DW); critical revision of the manuscript for important intellectual content (JEB, DG, DW); administrative, technical, or logistic support (JEB); and supervision (DG).
Send Correspondence to: Jan E. Berger, MD, MJ, Midwest Business Group on Health, 125 S Wacker Dr, Ste 1350, Chicago, IL 60606. Email: info@mbgh.org.
REFERENCES
1. Coleman-Jensen A, Rabbitt MP, Gregory CA, Singh A. Household food security in the United States in 2018. US Department of Agriculture Economic Research Service. September 27, 2019. Accessed June 1, 2020. https://www.ers.usda.gov/publications/pub-details/?pubid=94848
2. About social determinants of health. World Health Organization. Accessed September 20, 2019. https://www.who.int/social_determinants/sdh_definition/en/
3. Understand food insecurity. Feeding America. Accessed September 25, 2019. https://hungerandhealth.feedingamerica.org/understand-food-insecurity/
4. Heerman WJ, Wallston KA, Osborn CY, et al. Food insecurity is associated with diabetes self-care behaviours and glycemic control. Diabet Med. 2016;33(6):844-850. doi:10.1111/dme.12896
5. Herman D, Afulani P, Coleman-Jensen A, Harrison GG. Food insecurity and cost-related medication underuse among nonelderly adults in a nationally representative sample. Am J Public Health. 2015;105(10):e48-e59. doi:10.2105/AJPH.2015.302712
6. Seligman HK, Schillinger D. Hunger and socioeconomic disparities in chronic disease. N Engl J Med. 2010;363(1):6-9. doi:10.1056/NEJMp1000072
7. Pal R, Bhadada SK. COVID-19 and diabetes mellitus: an unholy interaction of two pandemics. Diabetes Metab Syndr. 2020;14(4):513-517. doi:10.1016/j.dsx.2020.04.049
8. Strategies. County Health Rankings & Roadmaps. Accessed September 20, 2019. https://www.countyhealthrankings.org/take-action-to-improve-health/what-works-for-health/strategies
9. County health rankings model. County Health Rankings & Roadmaps. Accessed June 1, 2020. https://www.countyhealthrankings.org/resources/county-health-rankings-model
10. Our ratings: evidence rating, disparity rating. County Health Rankings & Roadmaps. Accessed June 1, 2020. https://www.countyhealthrankings.org/take-action-to-improve-health/what-works-for-health/our-ratings
11. Gorn D. Food as medicine: it’s not just a fringe idea anymore. National Public Radio. January 17, 2017. Accessed June 1, 2020. https://www.npr.org/sections/thesalt/2017/01/17/509520895/food-as-medicine-it-s-not-just-a-fringe-idea-anymore
12. SFGH Therapeutic Food Pantry. San Francisco Health Network. Accessed June 1, 2020. https://sfhealthnetwork.org/sfghfoodpantry/
13. National Diabetes Statistics Report, 2020. CDC. Accessed June 1, 2020. https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf
Quality of Life: The Pending Outcome in Idiopathic Pulmonary Fibrosis
February 6th 2026Because evidence gaps in idiopathic pulmonary fibrosis research hinder demonstration of antifibrotic therapies’ impact on patient quality of life (QOL), integrating validated health-related QOL measures into trials is urgently needed.
Read More
Exploring Pharmaceutical Innovations, Trust, and Access With CVS Health's CMO
July 11th 2024On this episode of Managed Care Cast, we're talking with the chief medical officer of CVS Health about recent pharmaceutical innovations, patient-provider relationships, and strategies to reduce drug costs.
Listen
Building Trust: Public Priorities for Health Care AI Labeling
January 27th 2026A Michigan-based deliberative study found strong public support for patient-informed artificial intelligence (AI) labeling in health care, emphasizing transparency, privacy, equity, and safety to build trust.
Read More

