- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Real-World Treatment Sequences, Cost Analysis of Covalent BTK Inhibitors in CLL
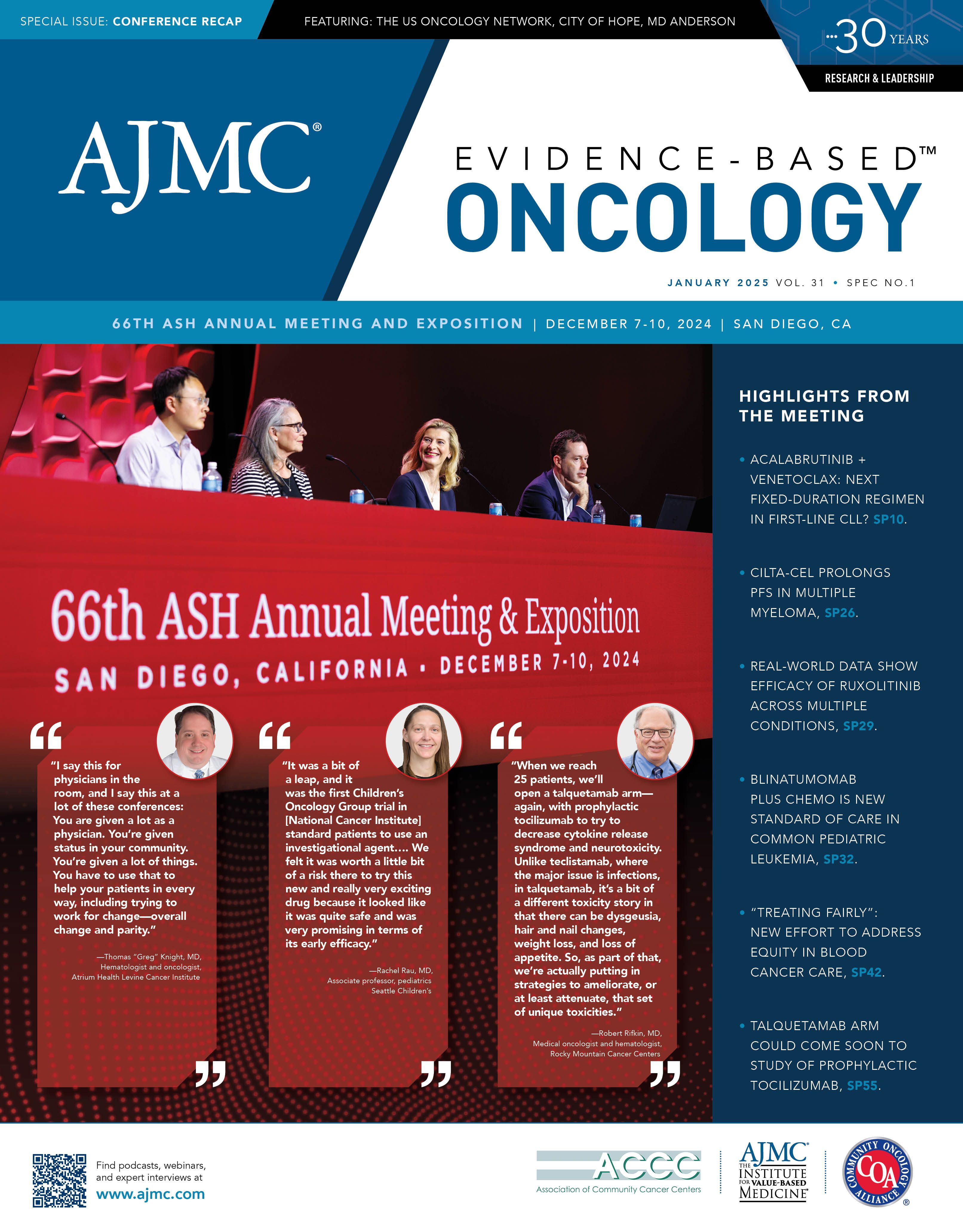
Two posters presented at the 66th American Society of Hematology (ASH) Annual Meeting and Exhibition focused on overall survival associated with real-world treatment sequences in patients with chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL) and the cost offset of covalent Bruton tyrosine kinase (BTK) inhibitors among patients with Medicare living with CLL.
The first study evaluated overall survival outcomes associated with commonly observed real-world treatment sequences in patients with CLL/SLL in the US.1 Utilizing the nationwide Flatiron Health electronic health record–derived database, the analysis included 2354 adults who initiated systemic therapy on or after 2016 and received at least 2 lines of therapy.
Treatment sequences were categorized based on drug class, with the most frequent 16 sequences analyzed. Key findings revealed that treatment sequences involving chemoimmunotherapy (CIT) followed by CIT, anti-CD20 antibody (aCD20ab) monotherapy followed by CIT, and covalent BTK inhibitor monotherapy followed by aCD20ab monotherapy were associated with significantly worse overall survival compared with patients treated with covalent BTK inhibitor monotherapy followed by a B-cell lymphoma 2 inhibitor plus aCD20ab.
Specifically, adjusted HRs for these sequences ranged from 2.47 (95% CI, 1.32-4.63) to 2.87 (95% CI, 1.54-5.34), indicating an elevated risk of mortality. Median overall survival was estimable only for patients receiving covalent BTK inhibitor monotherapy followed by aCD20ab monotherapy at 63 months.
Despite the availability of targeted therapies, many patients in the real-world setting continue to receive nontargeted regimens within earlier lines of treatment, which may impact survival outcomes. These findings underscore the importance of aligning treatment strategies with evolving guidelines to improve survival in CLL/SLL.
This second study assessed cost offsets associated with covalent BTK inhibitors—acalabrutinib, ibrutinib, and zanubrutinib—among Medicare patients with CLL.2 The analysis simulated health and economic outcomes over a 1-year period for treatment-naive and patients with relapsed/refractory CLL, incorporating treatment pathways, adverse event rates, and Medicare costs.
Acalabrutinib demonstrated significant cost savings compared with ibrutinib of $16,919 per patient, totaling $313 million, due to lower treatment costs and reduced adverse event–related expenses, particularly in rates of hypertension, infections, and atrial fibrillation. Compared with zanubrutinib, acalabrutinib achieved smaller but notable savings of $2529 per patient, totaling $47 million, driven by fewer hypertension and infection-related adverse events, which offset slightly higher treatment costs.
In subgroup analyses of disabled, end-stage renal disease, and terminally ill Medicare populations, acalabrutinib consistently reduced grade 3 or higher adverse events and achieved substantial cost savings compared with ibrutinib ($187 million, $13 million, and $42 million, respectively) and zanubrutinib ($31 million, $2.1 million, and $6.3 million, respectively).
Sensitivity analyses using matching-adjusted indirect comparison adverse event rates confirmed these findings, showing continued cost savings over 3- and 5-year horizons. Overall, the study highlights that acalabrutinib’s favorable safety profile, combined with reduced adverse event–related costs, translates to significant economic benefits for Medicare. These findings reinforce acalabrutinib as a cost-effective choice for treating patients with CLL, supporting its use in optimizing health care resource utilization.
References
1. Rhodes J, Bhandari N, Khanal M, et al. Overall survival associated with real-world treatment sequences in patients with CLL/SLL in the United States. Presented at: 66th ASH Annual Meeting and Exposition; December 7-10, 2024; San Diego, CA. Abstract 5114.
2. Kittai A, Patel D, Shafrin A, et al. Cost-offset analysis performed utilizing covalent Bruton’s tyrosine kinase inhibitors safety profiles among Medicare patients with chronic lymphocytic leukemia. Presented at: 66th ASH Annual Meeting and Exposition; December 7-10, 2024; San Diego, CA. Abstract 5031.